- 1Division of Movement Disorders, Department of Neurology, Yale School of Medicine, Yale University, New Haven, CT, United States
- 2Center for Neuroepidemiology and Clinical Neurological Research, Yale School of Medicine, Yale University, New Haven, CT, United States
- 3Department of Chronic Disease Epidemiology, Yale School of Public Health, Yale University, New Haven, CT, United States
Objective: We (1) report whether a companion (i.e., spouse, relative, aide) accompanied our consecutive outpatients with a range of movement disorders, (2) identified the set of patient characteristics that was associated with the need for a visit companion, and (3) characterized the role(s) of these companions during the visit. Our overarching goals were to further understand patient needs and the extent of their support networks, and to enrich the clinician-patient interface.
Methods: Two-hundred consecutive patients were enrolled from the Movement Disorders Clinic at Yale School of Medicine. We noted whether patients were accompanied by another person during the visit and documented the role of the visit companion during the encounter.
Results: One-hundred-twenty-eight of 200 patients (64.0%) brought a companion, with these being spouses (44.8%), adult children (24.1%) or an aide, nurse or social worker (14.5%). Patients who were unemployed (odds ratio [OR] = 5.32, p = 0.019), had a diagnosis of Parkinson's disease or other Parkinsonian syndromes (OR = 10.61, p = 0.001), or were dependent in any instrumental activities of daily living (iADLs) (OR = 4.99, p = 0.005) or basic activities of daily living (bADLs) (OR = 5.81, p = 0.02), had increased odds of presenting to the clinical visit with a visit companion. Visit companions' main roles involved communication (86.7%) and transportation (84.4%).
Conclusion: Visit companions were commonly present during movement disorders outpatient visits–two-thirds of patients were accompanied. A number of factors increased the odds of requiring such a companion by 4- or 5-fold.
Introduction
Movement disorders (e.g., Parkinson's disease [PD], essential tremor [ET]) are common neurological conditions that often affect motor independence (1, 2) and may also be accompanied by cognitive difficulties (3) and behavioral comorbidities (4, 5). Therefore, patients with movement disorders are considered a vulnerable population whose quality of life is often reduced by their burden of disease and disease-associated comorbidities (6–8).
Several studies have focused on the importance of family participation in patient care (5–8). For example, family members are partners in preventing hospital errors and in improving surveillance of adverse effects (9). However, studies of family involvement during outpatient medical visits are few in number and mainly oriented toward patients in geriatric and primary care settings, (10, 11) although some work has been done in neurology settings (12–15). These studies suggest an important role of family members both in enhancing patient-physician communication and in serving as agents of patient satisfaction with physician care (16).
There is a curious gap in knowledge. There are a limited number of studies of family participation in patients with neurological disorders (12–15). How often are such patients accompanied to their outpatient visit and what role(s) do companions play during these visits? In movement disorders in particular, motor, cognitive, and behavioral issues are quite common (1–5, 8). However, these issues are patchily distributed across these disorders (e.g., more common in some disorders than others, and dependent on the duration and stage of each disorder), leading to a complex mélange of patient conditions and needs. A priori, we hypothesized that older patients, patients with cognitive impairment, patients with functional dependency, and patients with certain disorders (e.g., PD) would most frequently be accompanied during their encounter. However, we had no a priori sense of the percentage of patients with each condition who might require a companion.
In this study of 200 outpatient movement disorder visits, we aimed to (1) report whether a companion (i.e., spouse, relative, aide) accompanied our patients with a range of movement disorders, (2) identify the set of patient characteristics that was associated with the need for a visit companion, and (3) characterize the role(s) of these companions during the visit. Our overarching goals were to contribute to information regarding patient needs, their health care behaviors, and their support networks, and to enrich the clinician-patient interface.
Materials and Methods
Study Design
Patients were consecutively recruited by AV-R, a movement disorders fellow, from September–December 2017 from the Movement Disorders Clinic at Yale School of Medicine. AV-R had an average of four half-day clinics per week with four different movement disorder neurologists (including EDL). The study was reviewed and approved by the Yale University Institutional Review Board (IRB) (IRB #2000024723). The Yale IRB committee approved a written informed consent waiver. Subjects provided informed assent and were permitted to withdraw from participation at any time.
At the end of the clinic visit, demographic and clinical information were collected directly from the patient and their clinical records, including age, gender, distance from our medical center, type of insurance (e.g., Medicare, Medicaid), median annual income in county of residence, ethnicity, visit type (e.g., routine visit, botulinum toxin clinic), initial, or follow up visit, number of canceled medical visits in previous year, diagnosis, patient mobility, and functionality/dependence, employment status, presence of a prior diagnosis of mild cognitive impairment or dementia (by history and chart review), whether or not the patient was accompanied to their appointment by another person, and if so, that person's relationship to the patient. A visit companion was defined as a person 18 years or older who came to the clinic visit with the patient.
Patient mobility was categorized based on how the patient entered the examination room (walking independently, using a cane, using a walker, or using a wheelchair). Patients were categorized as dependent in instrumental activities of daily living (iADLs) if they required assistance with one or more of the following activities: grocery shopping, household finances, driving/using public transportation, household chores, using the telephone, or taking medication. Patients were categorized as dependent in basic activities of daily living (bADLs) if they required assistance with one or more of the following activities: eating, bathing, getting dressed, toileting, and personal mobility (17, 18).
AV-R documented the roles of the visit companion during the encounter and categorized them into one or more of the following: (1) transportation, if the companion drove or picked the patient up in order to bring him/her to the appointment; (2) communication, if the companion provided medication history, gave additional medical history or if the companion directed the conversation for the patient; (3) moral support, if the companion provided reassurance after a disclosure of the diagnosis or re-framed difficult questions or statements for the patient; and (4) physical assistance, if the companion helped the patient get in/out of the chair or if the companion wheeled the patient into the office.
Sample Size Determination and Data Analysis
Patients were enrolled consecutively until the targeted sample of 200 patients was reached. There were no refusals. Sample size was calculated according to the method proposed by Peduzzi et al. (19, 20) which is based on the expected proportion for the primary outcome and the number of variables that need to be accounted for in regression models during the analysis of data. Based on the most common movement disorders treated in our clinic and the age of our patients, we expected that the proportion of accompanied patients to be similar to that reported in geriatric outpatient encounters (~40%) (11, 16, 21). We expected to include eight independent variables in the final multivariate logistic regression model (described below).
Analyses were performed in Stata (Version IC 15.1). To facilitate data analysis, diagnoses were collapsed into 5 categories: (1) PD and other parkinsonian syndromes, (2) dystonia, (3) ET, (4) other degenerative disorders or disorders with spasticity/gait impairment (e.g., cerebellar ataxias and Huntington's disease), and (5) other non-degenerative disorders without gait impairment (e.g., tardive dyskinesia and restless legs syndrome).
We first reported the proportion of patients who had a visit companion. Then, bivariate analyses were performed using Mann-Whitney and chi-square tests to evaluate differences between patients for whom a visit companion was present vs. patients for whom a visit companion was not present. A series of bivariate logistic regression analyses assessed the association between clinical variables and the presence vs. absence of a visit companion (dependent variable), resulting in odds ratios (ORs), 95% confidence intervals (CIs), and p-values. Significance was set at p <0.05. Finally, after identifying statistically significant variables from the bivariate analysis, multivariate logistic regression models were constructed to determine which factors were independently associated with visit companionship.
Results
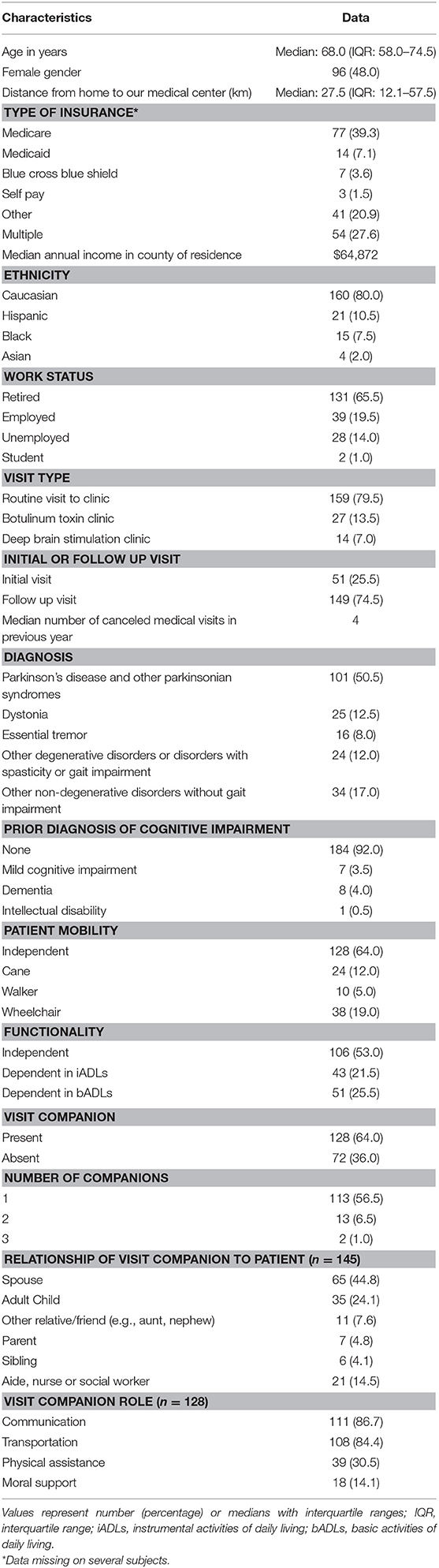
Our targeted enrollment of 200 patients was met after 3 months (Table 1). The median age was 68.0 years (inter-quartile range [IQR] = 58.0–74.5) and both genders were nearly equally represented. The three most frequent diagnoses were PD and other parkinsonian syndromes (n = 101, 50.5%), dystonia (n = 25, 12.5%), and ET (n = 16, 8.0%), accounting for more than two-thirds of enrollees. Median age for these diagnoses were 71 years (IQR = 66–76) for PD, 58 years (IQR = 51–64) for dystonia and 70.5 years (IQR = 66–74) for ET (Kruskal Wallis; p = 0.001). Only the dystonia group had a significant difference in age compared to ET and PD cases (Mann Whitney with Bonferroni correction: ET vs. dystonia p = 0.004; ET vs. PD p = 0.43; dystonia vs. PD p = <0.001). Eight percent of patients reported a previous diagnosis of mild cognitive impairment or dementia. Two-thirds (64.0%) came to the visit walking independently without the use of a cane or walker and 53.0% were independent for both iADL and bADL.
One-hundred-twenty-eight of 200 patients (64.0%) brought a visit companion. The total number of visit companions was 145 (i.e., some patients had more than one visit companion). Spouses were the most frequent type of companion (65 of 145, 44.8%), followed by adult children (24.1%), or aides, nurses, or social workers (14.5%). In two cases, the visit companion provided transportation but stayed in the waiting area during the encounter. Among companions who were family members (n = 124), 86 (69.4%) were female and 38 (30.6%) were male.
Among 128 patients who came in with a visit companion, the companions' main roles involved communication (111 of 128, 86.7%) and transportation (84.4%). Only 30.5% of patients who had a companion required physical assistance from the companion during the encounter.
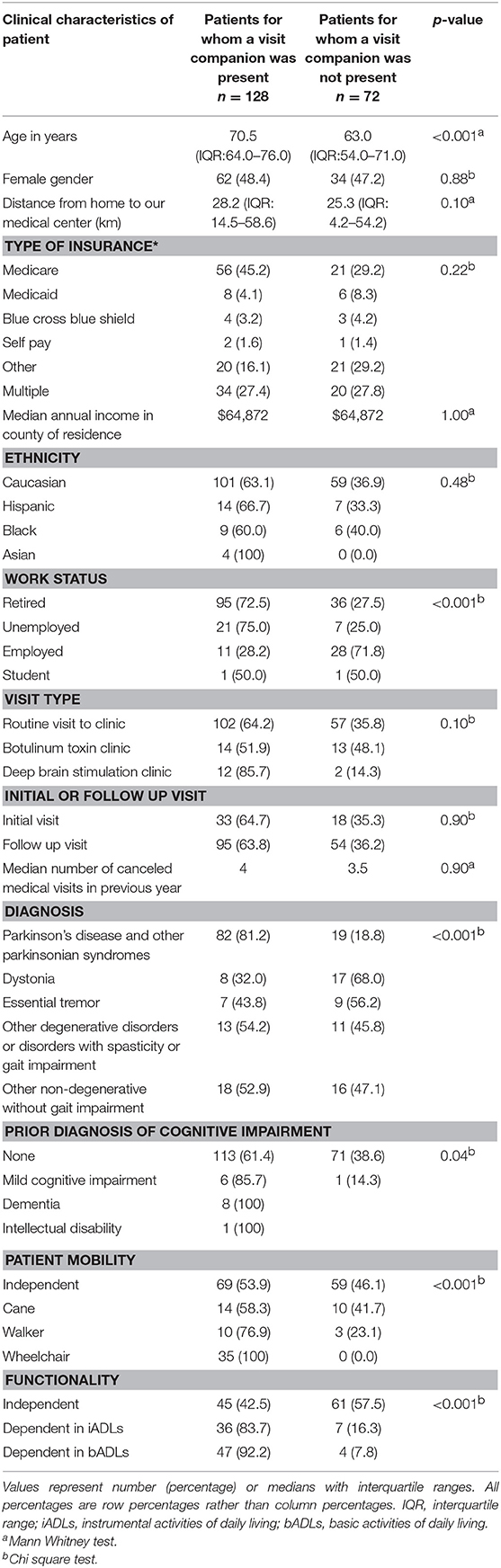
Accompanied vs. unaccompanied patients differed with respect to numerous demographic and clinical characteristics. Accompanied patients were on average older, and were more often retired, parkinsonian, impaired in cognition, impaired in mobility, and functionally dependent (Table 2). They did not differ in numerous respects (e.g., gender, distance from medical center, type of insurance, median annual income in county of residence, median number of canceled medical visits in the previous year).
Of the 16 patients with prior diagnosis of cognitive impairment, 15 (93.8%) were accompanied. Of the 101 patients with a diagnosis of parkinsonism, 81.2% were accompanied in contrast to patients with dystonia and ET who were less frequently accompanied (32.0% [p < 0.001] and 43.8% [p = 0.001], respectively). All patients in a wheelchair had a companion during the visit as compared to 76.9% of patients with a walker, 58.3% of patients with a cane, and 53.9% of patients who were independent with respect to mobility (p < 0.001). Of the 51 patients who required assistance with bADL, 92.2% were accompanied. In contrast, only 42.5% of patients who were fully independent in ADLs were accompanied to the visit (p < 0.001).
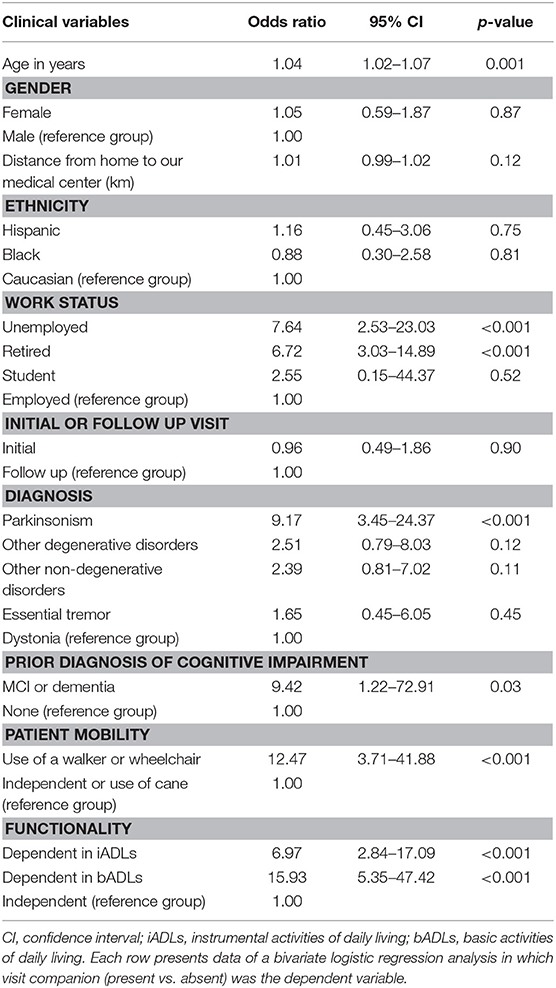
In a series of bivariate logistic regression analyses (Table 3), older age, a diagnosis of parkinsonism, and a presence of any cognitive impairment were associated with higher odds of having a companion during the visit. Retired and unemployed patients were also more likely to be accompanied to the visit (reference group = employed patients). Patients who were dependent with iADLs, bADLs (reference group = independence in daily activities), and patients who required a walker or a wheelchair (reference group = independence in ambulation or use of a cane) had increased odds of having a visit companion present. No association was documented for a diagnosis of ET, other degenerative and other non-degenerative disorders, traveling distance, patient's ethnicity, or visit type.
We performed a multivariate logistic regression analysis including age, gender, work status, diagnosis, presence of cognitive impairment, patient mobility and functionality, and found that only patients who were unemployed (OR = 5.32, p = 0.019, CI: 1.31–21.61), had a diagnosis of PD or other parkinsonian syndromes (OR = 10.61, p = 0.001, CI: 2.68–41.97), or were dependent in any iADLs (OR = 4.99, p = 0.005, CI: 1.63–15.25) or dependent in any bADLs (OR = 5.81, p = 0.02, CI: 1.29–26.04), had increased odds of presenting to the clinical visit with a companion. No association was documented for the use of a walker or a wheelchair for mobility, but a trend was seen (OR = 4.14, p = 0.08, CI: 0.83–20.69).
Discussion
Previous studies performed in primary care and geriatric clinics have reported that 30–50% of patients are accompanied during outpatient visits (10, 11, 21). Though our sample was younger than those of previously described geriatric cohorts [median age of this cohort: 68 years vs. 74–78.5 years in previous studies (11, 16, 22), we documented a higher proportion of patients who brought companions (64.0%). This higher proportion may be due to the progressive nature and comorbidities associated with movement disorders. The prevalence varied considerably across the different movement disorders, from 32.0% in dystonia patients to 81.2% in PD patients. Even in ET patients, which is a disorder that progresses slowly and does not compromise mobility to a marked degree in most patients, the prevalence was more than 40%.
In our study, patients were primarily accompanied by family members (spouse and adult children). As in prior studies, we documented a female predominance in patients' companions (69.4%). This could be related to the fact that women are still described as the predominant care providers for family members with chronic medical conditions or disabilities (23). However, in the parkinsonian group, which had the highest prevalence of visit companions, there was a male predominance among patients who were accompanied (58 males vs. 32 females). This could have potentially shifted the companions' gender in the sample to a female predominance (i.e., their spouses).
As anticipated, the presence of a visit companion was associated with a diagnosis of PD or parkinsonian syndromes and functional impairment. Specifically, in multivariate analyses, a diagnosis of PD or other parkinsonian syndromes was associated with more than ten times increased odds of being accompanied to the visit. Parkinsonian syndromes are progressive neurodegenerative disorders that not only affect mobility but also manifest with an array of non-motor symptoms, including depression, apathy, dysautonomia, and cognitive decline. These symptoms can significantly affect quality of life (7, 24).
Furthermore, functional impairment was independently associated with the presence of a visit companion, with a higher association in patients who were dependent in bADLs than in iADLs. Surprisingly, impaired patient mobility did not achieve statistical significance in predicting patient companionship. Though this could simply be due to study power and sample size, one might also infer that patient disability (based on ADLs) plays a more important role among patients requiring companionship.
Unemployed patients had a higher prevalence of companions as well. Upon review of the cases, these corresponded to patients with significant psychiatric or neurological disorders that complicated their ability to work, and many required government assistance. This suggests that the presence of a visit companion during clinical visits could be a marker associated with social risk and functional dependence.
We had hypothesized that older patients as well as patients with cognitive impairment would most frequently be accompanied during their encounters. Indeed, in initial analyses (Tables 2, 3), both variables were significantly associated with presence of a visit companion. However, in multivariate models, neither variable remained. For cognitive impairment, this could be related to the small proportion of patients with a prior diagnosis of cognitive impairment in our cohort (n = 16 or 8.0%). In some ways, it is not surprising that age did not remain significant in the final model either, as it is probably not age itself that is responsible for the need for a visit companion, but rather, age-associated issues such as parkinsonism and difficulty with ADLs, which did remain in the model.
During the clinical encounters, visit companions were most frequently involved with transportation logistics and communication. These aspects appeared to be more important during these visits than physical assistance. As previously described in geriatric populations, visit companions are potential facilitators during clinical visits, actively engaging in the exchange of health information (16). In movement disorders, their presence becomes vital, especially among more vulnerable, and functionally impaired patients.
The data presented here contribute to our understanding of patient needs, their health care behaviors, and their support networks, with the over-arching goal to enrich the clinician-patient interface. The fact that some patients utilize visit companions suggests that they are a vulnerable group, requiring the additional assistance of such companions. The presence of a companion should alert the physician to this fact and forewarn them to spend additional time with that patient to explain treatment plans and to ensure that such plans are practical given limitations in the patient's capacities and circumstances.
To our knowledge, our study is the first to analyze the presence of visit companions during outpatient care in patients with a range of movement disorders. With our large sample size, we managed to enroll the most common movement disorders encountered in clinic and we collected data and were able to analyze a broad range of clinical, demographic, and social variables in the analysis.
A main limitation of this study is that only one clinician oversaw the assignment of the companion's role. Even though we defined specific criteria a priori to avoid subjectivity, our study design could have influenced our results. Second, patients did not provide insight into companion roles, or lack thereof. Therefore, the complexity of the physician-patient-companion relationship was not fully explored; other studies have taken additional steps to define and expand on the role of the companion more fully (12). Third, some variables were determined through chart review (e.g., cognitive impairment) and may not accurately reflect patients' status and other variables were not directly assessed (e.g., medical literacy). Fourth, a range of other social factors could have influenced patient behaviors and use of a visit companion; (14) future studies should explore these issues. Among variables that we did not consider were education and the availability of family members. Fifth, although the sample size was 200, in some cells, the numbers were small, and a larger sample size would have alleviated this issue; the use of Bayesian approaches to the data would also be of value in future studies. Finally, we did not explore how visit companions improved the quality of care. In other words, this was a foundational study of the frequency with which patients used a visit companion and the clinical correlates of that use. This was not a study of the utility of using such a companion or the effects that such companions had on care (i.e., this was not an outcomes study). Future longitudinal studies could review the prognostic value of companions in movement disorders clinics by documenting the association between absence of such companions and medication intake errors, lower treatment adherence, and loss to follow-up.
Conclusion
In this cohort of movement disorders patients, the prevalence of visit companions was higher than previously described in other geriatric populations. Two-thirds of patients required such a companion. The presence of a visit companion was independently associated with a diagnosis of PD or other parkinsonian syndromes, unemployment, and functional impairment. Companions' role during the encounters focused on enhancing communication and assisting with patients' transportation. Several of these factors increased the odds of requiring such a companion by 4- or 5-fold. These data highlight the potential value of visit companions during neurological visits, especially among more vulnerable and functionally impaired patients.
Disclosure
EL receives/has received research support from NIH/NINDS.
Author Contributions
AV-R: drafting/revising the manuscript for content, including medical writing for content, study design, analysis and interpretation of data. DT: drafting/revising the manuscript for content, including medical writing for content, analysis or interpretation of data. EL: drafting/revising the manuscript for content, including medical writing for content, study concept and design, analysis and interpretation of data.
Funding
EL has received research support from the National Institutes of Health: NINDS #R01 NS094607 (principal investigator), NINDS #R01 NS085136 (principal investigator), NINDS #R01 NS073872 (principal investigator), and NINDS #R01 NS088257 (principal investigator).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Boonstra TA, van der Kooij H, Munneke M, Bloem BR. Gait disorders and balance disturbances in Parkinson's disease: clinical update and pathophysiology. Curr Opin Neurol. (2008) 21:461–71. doi: 10.1097/WCO.0b013e328305bdaf
2. Arkadir D, Louis ED. The balance and gait disorder of essential tremor: what does this mean for patients? Ther Adv Neurol Disord. (2013) 6:229–36. doi: 10.1177/1756285612471415
3. Bocanegra Y, Trujillo-Orrego N, Pineda D. Dementia and mild cognitive impairment in Parkinson's disease: a review. Rev Neurol. (2014) 59:555–69. doi: 10.33588/rn.5912.2014082
4. Tan EK, Fook-Chong S, Lum SY, Gabriel C, Koh KK, Prakash KM, et al. Non-motor manifestations in essential tremor: use of a validated instrument to evaluate a wide spectrum of symptoms. Parkinsonism Relat Disord. (2005) 11:375–80. doi: 10.1016/j.parkreldis.2005.04.007
5. Louis ED, Huey ED, Gerbin M, Viner AS. Depressive traits in essential tremor: impact on disability, quality of life and medication adherence. Eur J Neurol. (2012) 19:1349–54. doi: 10.1111/j.1468-1331.2012.03774.x
6. Dodel R, Schrag A. Health-Related Quality of Life in Movement Disorders. In: Handbook of Disease Burdens and Quality of Life Measures, New York, NY: Springer (2010). p. 4013–34. Available online at: https://link.springer.com/referenceworkentry/10.1007/978-0-387-78665-0_234
7. Opara J, Brola W, Leonardi M, Błaszczyk B. Quality of life in Parkinson‘s disease. J Med Life. (2012) 5:375–81.
8. Louis ED, Machado DG. Tremor-related quality of life: a comparison of essential tremor vs. Parkinson's disease patients. Parkinsonism Relat Disord. (2015) 21:729–35. doi: 10.1016/j.parkreldis.2015.04.019
9. Khan A, Coffey M, Litterer KP, Baird JD, Furtak SL, Garcia BM, et al. Families as partners in hospital error and adverse event surveillance. JAMA Pediatr. (2017) 171:372–81. doi: 10.1001/jamapediatrics.2016.4812
10. Schilling LM, Scatena L, Steiner JF, Albertson GA, Lin CT, Cyran L, et al. The third person in the room: frequency, role, and influence of companions during primary care medical encounters. J Fam Pract. (2002) 51:685–90.
11. Clayman ML, Roter D, Wissow LS, Bandeen-Roche K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc Sci Med. (2005) 60:1583–91. doi: 10.1016/j.socscimed.2004.08.004
12. Kluger BM, Persenaire MJ, Holden SK, Palmer LT, Redwine HM, Berk J, et al. Implementation issues relevant to outpatient neurology palliative care. Ann Palliat Med. (2018) 7:339–48. doi: 10.21037/apm.2017.10.06
13. Ward CD, Phillips M, Smith A, Moran M. Multidisciplinary approaches in progressive neurological disease: can we do better? J Neurol Neurosurg Psychiatry. (2003) 74(Suppl 4):iv8–iv12. doi: 10.1136/jnnp.74.suppl_4.iv8
14. Fleisher J, Bhatia R, Margus C, Pruitt A, Dahodwala N. Health literacy and medication awareness in outpatient neurology. Neurol Clin Pract. (2014) 4:71–81. doi: 10.1212/01.CPJ.0000436211.73013.ab
15. Sayers SL, White T, Zubritsky C, Oslin DW. Family involvement in the care of healthy medical outpatients. Fam Pract. (2006) 23:317–24. doi: 10.1093/fampra/cmi114
16. Wolff JL, Roter DL. Hidden in plain sight: medical visit companions as a resource for vulnerable older adults. Arch Intern Med. (2008) 168:1409–15. doi: 10.1001/archinte.168.13.1409
17. Wiener JM, Hanley RJ, Clark R, Van Nostrand JF. Measuring the activities of daily living: comparisons across national surveys. J Gerontol. (1990) 45:S229–37. doi: 10.1093/geronj/45.6.S229
18. Hardy SE. Consideration of Function and Functional Decline. In: Williams BA, Chang A, Ahalt C, Chen H, Conant R, Landefeld CS, editors. Current Diagnosis and Treatment: Geriatrics. 2nd ed. New York, NY: McGraw-Hill Education (2014). p. 3–8.
19. Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol. (1995) 48:1503–10. doi: 10.1016/0895-4356(95)00048-8
20. Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. (1996) 49:1373–9. doi: 10.1016/S0895-4356(96)00236-3
21. Brown JB, Brett P, Stewart M, Marshall JN. Roles and influence of people who accompany patients on visits to the doctor. Can Fam Physician. (1998) 44:1644–50.
22. Greene MG, Majerovitz SD, Adelman RD, Rizzo C. The effects of the presence of a third person on the physician-older patient medical interview. J Am Geriatr Soc. (1994) 42:413–9. doi: 10.1111/j.1532-5415.1994.tb07490.x
23. Sharma N, Chakrabarti S, Grover S. Gender differences in caregiving among family - caregivers of people with mental illnesses. World J Psychiatry. (2016) 6:7–17. doi: 10.5498/wjp.v6.i1.7
Keywords: movement disorders, visit companions, caregiver, Parkinson's disease, essential tremor
Citation: Vives-Rodriguez A, Trujillo Diaz D and Louis ED (2019) Patient Companionship in a Movement Disorders Clinic: Outside Assistance Inside the Office. Front. Neurol. 10:182. doi: 10.3389/fneur.2019.00182
Received: 27 September 2018; Accepted: 13 February 2019;
Published: 05 March 2019.
Edited by:
Huifang Shang, Sichuan University, ChinaReviewed by:
Giovanni Pellegrino, Montreal Neurological Institute and Hospital, McGill University, CanadaAthanasios Alexiou, Novel Global Community Educational Foundation (NGCEF), Hebersham, Australia
Richard B. Reilly, Trinity College Dublin, Ireland
Copyright © 2019 Vives-Rodriguez, Trujillo Diaz and Louis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elan D. Louis, ZWxhbi5sb3Vpc0B5YWxlLmVkdQ==
 Ana Vives-Rodriguez
Ana Vives-Rodriguez Daniel Trujillo Diaz
Daniel Trujillo Diaz Elan D. Louis
Elan D. Louis