- 1Division of Neurosurgery, St. Michael's Hospital, Toronto, ON, Canada
- 2Faculty of Medicine and the Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada
- 3Department of Occupational Science and Occupational Therapy, University of Toronto, Toronto, ON, Canada
- 4Department of Community Health and Epidemiology, Dalhousie University, Halifax, NS, Canada
Objective: The goal of this research was to assess the effectiveness of available concussion educational resources in Canada, the means used to disseminate this knowledge and the impact of these educational resources on players' concussion prevention knowledge.
Methods: We assessed concussion knowledge before and after exposure to one or more of 19 resources introduced through a national program aimed to increase awareness and knowledge of concussion. The effectiveness of the mode of delivery was measured by changes in concussion knowledge scores (CKS) between pre and pro scores.
Measures: Concussion knowledge scores (CKS) were calculated for pre- and post- exposure to concussion educational resources and used as a measure of both, the effectiveness of each resource as well as the effectiveness of the delivery method. The effectiveness of each educational resource was also measured by the respondents' rating of each concussion educational resource.
Results: Respondents in post-survey had higher CKS than those in pre-survey. Two out of the 19 newly developed concussion educational resources were effective in improving the resource users' CKS. Linear regression showed that using more resources further increased CKS. Four out of six modes of delivery enhanced respondents' concussion knowledge.
Conclusion: Our findings demonstrate that the newly developed Canadian concussion educational resources were effective at improving users' concussion knowledge. Our data demonstrates that using three or more resources further enhanced the users' concussion knowledge. Future research, however, is critical to assess whether concussion prevention knowledge is sufficient to reduce injuries and factors influencing it.
Introduction
Traumatic Brain Injury (TBI) is a significant public health concern (1) and a “silent epidemic” (2) that affects approximately 1.7 million people in the United States each year from which about 275,000 are hospitalized and 52,000 die (3). In 2010 alone, it was estimated that the cost of TBIs in the United States was about $76.5 billion and $10 billion in Canada (4–6). Despite the tremendous healthcare and economic burden of TBI, a lack of knowledge in recognizing TBI or concussion is quite common and worrisome. For example, in one study, it was observed that more than half of the study's participants underestimated the prevalence of concussion and more than 30% were unaware of any return-to-play protocols (7). Other studies have identified several gaps in concussion awareness and knowledge (8, 9) including the lack of awareness of the effects of concussion on psychosocial functioning post injury, and the lack of care management post-concussion among athletes (10). However, researchers have also proposed that through educational interventions or knowledge translation activities, it may be possible to improve concussion knowledge (11–13). In a recent systematic review focusing on the effectiveness of interventions in preventing injuries in hockey (14) it was observed that rule changes could lead to a reduction in injury rate. However, only 11 studies provided conclusive evidence supporting the effectiveness of increasing concussion knowledge or awareness by educational intervention. Delivery of this knowledge was achieved through mobile app, or pamphlet (15), website (16), information sheet or seminar/presentation (17–19), physical education class (20), poster or other formats (21–25). In spite of some attempts to increase players' education, a recent study showed that over the last 20 years, old misconceptions about concussion continue to persist among school educational professionals surveyed between 1997 and 2017 (26). Although a multimodal educational intervention has been shown to positively influence primary care providers to adhere to the consensus-based guidelines in their concussion management practice (27), even after the legislation that mandated concussion education for student athletes, athletes fail to recognize concussion symptoms (28). Little is known whether or not the format of educational intervention (e.g., video vs. text) can play a role and whether or not the combination of different formats of educational interventions would be more effective in changing the behavior of non-medical professionals. Furthermore, overall little information exists to evaluate concussion educational resources with the ultimate goal to better translate concussion knowledge to the general public. To this end, the Public Health Agency of Canada (PHAC) engaged four Partners consisting of Hockey Canada (HC), Coaching Association of Canada (CAC), Canadian Centre for Ethics in Sport (CCES), and Think First (now a part of Parachute) to develop various concussion educational resources and survey thousands of Canadians about these resources. Our research group has reported the survey results and respondents' concussion knowledge previously (29, 30). The analyses we present here, however, extend previous reports by evaluating the effectiveness of the newly developed concussion resources individually to deliver concussion education, their added value to concussion knowledge, as well as evaluating the effectiveness of their different formats of delivery. We hypothesized that exposure to concussion educational resources would improve participants' knowledge and understanding of concussion.
Methods
Ethics
The study received approval from the Research Ethics Board of St. Michael's Hospital. Participants provided consent prior to completion of the survey.
National Surveys and Concussion Educational Resources
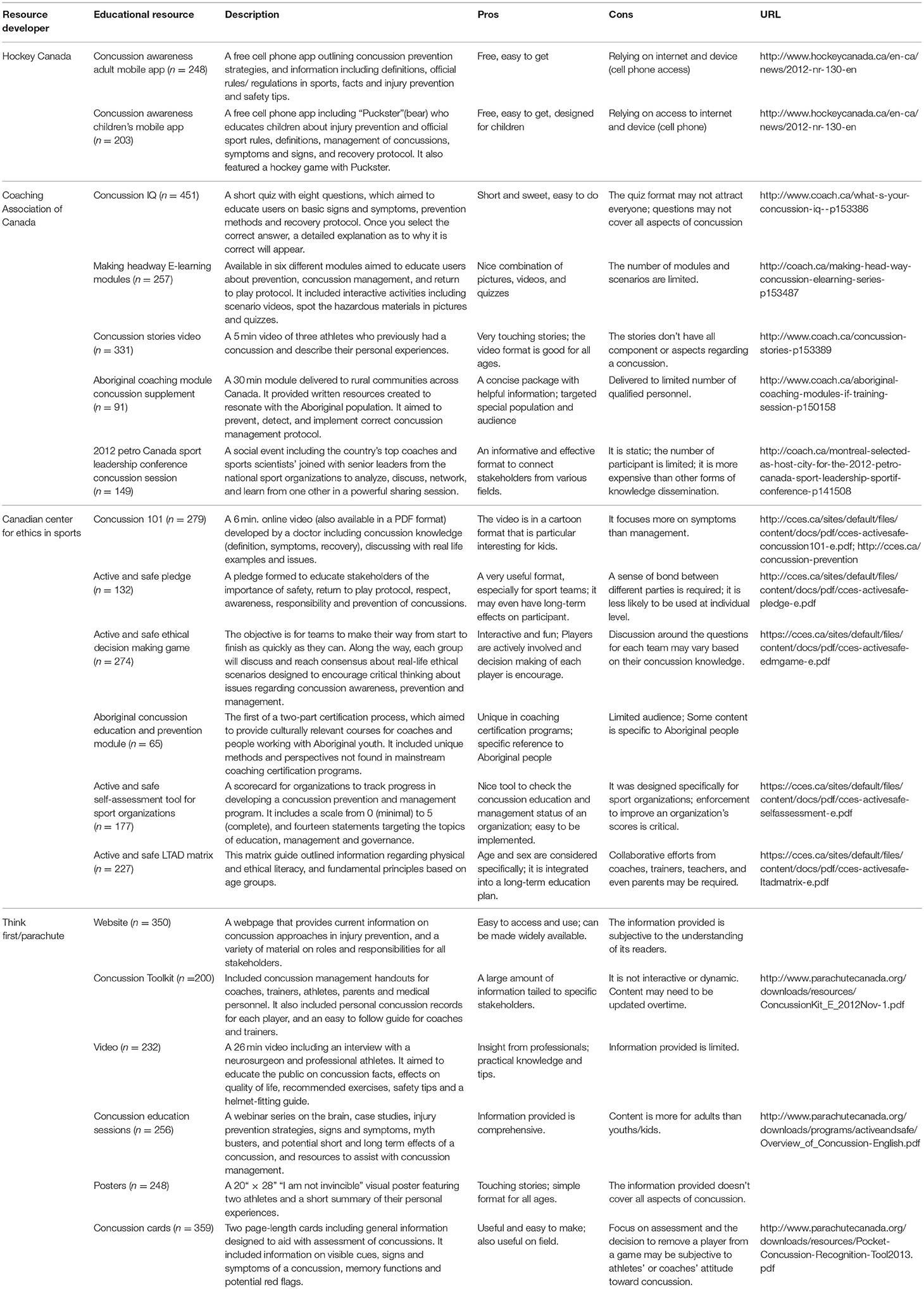
This study reports on the results of two Canadian cross-sectional surveys that were administered before and after the respondents' exposure to concussion educational resources. Pre-survey responses were completed by 7,258 respondents whereas post-survey were completed by 6,031 respondents, respectively. Both surveys were described previously (29, 30). The 19 concussion educational resources evaluated are described in Table 1. A cross-sectional, anonymous, voluntary, open survey with a convenience sample of the stakeholders in the sports community in Canada, was conducted in two waves as described previously.
Study Sample
As the surveys were conducted anonymously, the computer's IP address was used as a proxy for user's identification. Based on the survey data, 1,186 unique IP addresses were identified from which 503 were used in both the pre- and post-survey and 180 were used only in the pre-survey. The analysis reported here was conducted using the data set from the 503 survey respondents who completed the pre and post survey. The sample size obtained for each resource is indicated in Table 1.
Measures
Demographic and Social Characteristics
Language, age, sex, ethnicity, education, annual household income, geographic location, and the non-medical community role the survey respondent most strongly identified with in their community were collected.
Changes in concussion knowledge scores (CKS) between pre- and post-survey testing as a measure of the effectiveness of concussion resources. As described previously (29, 30). CKS were calculated by summing the correct answers to 27 items that surveyed concussion knowledge related to physical/cognitive/mental health symptoms, concussion treatment modality, return-to-sport following a concussion, or diagnosis of concussion post head injury. The 27 items were evaluated using a dichotomous scoring process. Correct responses were given a score of one and incorrect responses were given a score of zero. Higher CKS scores indicated better knowledge of concussion. The CKS changes pre- and post- survey between the resource users and non-users as well as all respondents was used as a measure of resource effectiveness.
Respondents' Ratings of the Educational Material as a Measure of the Effectiveness of Concussion Resources
Ratings were based on participants' self- reports on the level of effectiveness (not effective, neutral, or extremely effective) for each concussion educational resource.
Mode of Delivery and Its Effectiveness
Each concussion resource was classified into one of six forms of delivery: (1) webpage (e.g., a website from Parachute); (2) written guidelines (e.g., active and safe self-assessment tool for sport organizations); (3) quizzes (e.g., concussion IQ); (4) videos (e.g., the concussion stories video); (5) phone apps (e.g., the children and adult's concussion awareness mobile apps); and (6) in-person resources (e.g., 2012 Petro Canada sport leadership conference concussion session). Educational mode of delivery effectiveness was evaluated by examining CKS changes between pre- and post- scores for each form of delivery.
Data Analyses
Statistical analyses were performed using SAS 9.4 4 (SAS Institute, Inc., Cary, NC, USA) and STATA 13.0 (StataCorp LLC, College Station, TX, USA). Descriptive statistics of language, sex, age, education, household income, and survey respondent location were used to describe the demographic characteristics of the survey respondents. Pearson's correlation coefficient and Wald's F test were used to compare the effectiveness of each concussion educational resource measured by changes on CKS. Student t-tests were performed to compare CKS between pre- and post- surveillance between the resource users and non-users in the post-survey group. An ordinary linear regression was performed with CKS as the dependent variable and age, sex, level of education, household income, use (or not use) the 19 educational resources as the independent variables. An alpha value of 0.05 or less was considered statistically significant, however, Bonferroni adjustments were applied for significance assessments to correct for experiment-wise error.
Results
Characteristics of Survey Respondents
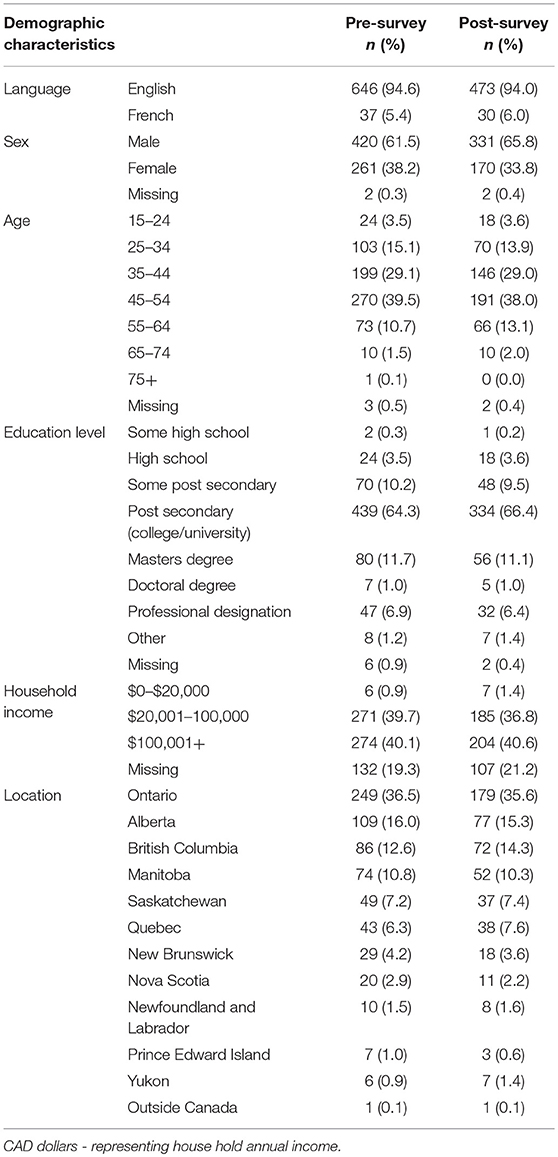
In both pre-and post-survey, the proportion of respondents falling into each age category and the male to female ratio (2:1) remained primarily unchanged. Roughly 78% of respondents wereas between the age of 35 and 54 while less than 4% fell into the younger (< 25 years) or older respondent (>64 years) categories (n = 1,186, Table 2). Almost two thirds of respondents resided in Ontario, Bristish Columbia, or Alberta and reported a post secondary education at a college/university level (about 84%) with a household income greater than $20,000 (Table 2).
Effectiveness of Concussion Resources Measured by CKS Change
Group comparisons were performed and results showed that both resource users and non-users in the post-survey had significantly higher CKS than at pre-survey while users' CKS were significantly higher than that of non-users (Table 3).
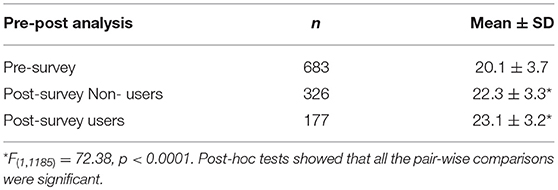
Table 3. Comparison of CKS between respondents of the pre- and post- survey as well as between users and non-users in post-survey.
Linear regression analyses showed that level of education affected the respondents' CKS. A higher level of education was associated with higher CKS overall. However, age, sex, and income were not statistically significantly associated with changes in the respondents' CKSs from pre to post test. Results also indicated that the use of Concussion IQ and Concussion Cards was the only form of concusion educational resource that statistically significantly increased respondents' CKS from pre to post survey (Table 4).
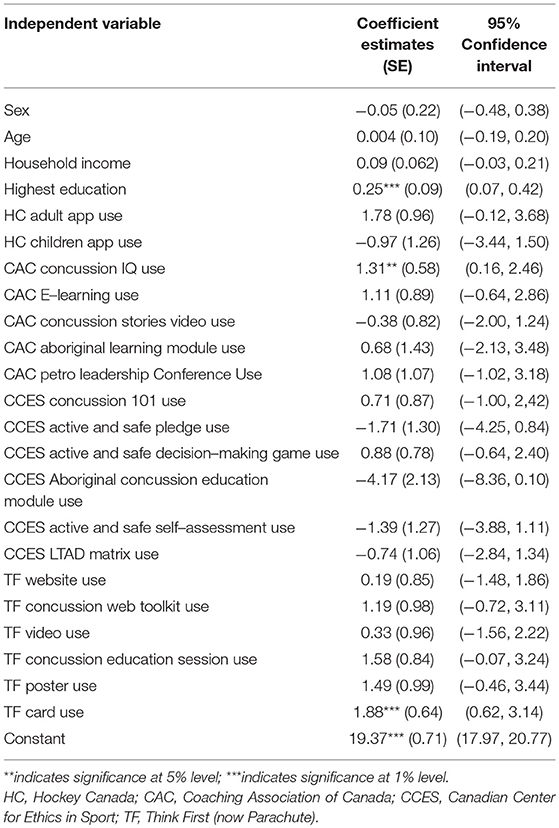
Table 4. Ordinary linear regression analysis of the prediction of CKS based on individual concussion resource use and demographics.
Importantly, using three or more resources was predictive of a statistically significant increase in CKS than using a single resource (Figure 1).
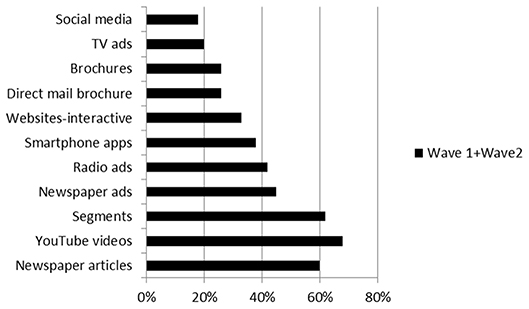
Figure 1. (1.1). Means and standard errors for CKS for the distribution of number of concussion educational resources used by respondents. Figure (1.2). Percentage of concussion educational resources used by respondents.
Effectiveness of Concussion Resources Related to Mode of Delivery
The mode of delivery for all concussion educational resources was analyzed to determine the most effective method of distribution of concussion knowledge and awareness resources. Based on the mode of delivery, CKS of respondents who used any of the concussion resources in post-survey were compared to that of those who were not exposed to such resources in pre-survey (Figure 2) or those who did not use such resources in post-survey (Figure 2).
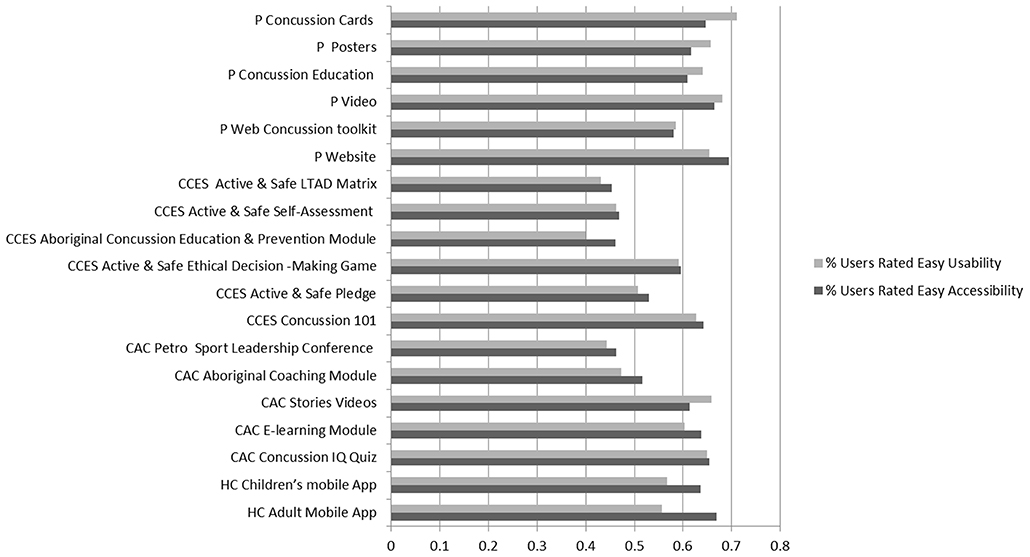
Figure 2. (2.1) Means and standard errors for CKS pre-, post-survey users, and post-survey non-users stratified by mode of delivery. CKS means for both users and non-users post-survey were statistically significantly higher (p < 0.0001) than pre-survey CKS means. *p < 0.05, **p < 0.001. (2. 2) Proportion of concussion educational resources rated by users in terms of ease of usability and accessibility.
When comparing resource users with non-users in the post- survey, we found that 4 out of 6 modes of delivery significantly increased the users' CKS. Quizzes and videos were the only two delivery methods that failed to impact CKS (Figure 2). When compared, there was no significant difference found among different educational format modalities (p > 0.05).
Effectiveness of Concussion Resources Measured by Respondents' Rating
Respondents were asked to rate the effectiveness of each concussion resource (Figure 3). Overall, most resources were rated as “extremely effective” (Figure 3). However, a regression analysis on the correlation between respondents' ratings and their CKS did not reveal a statistically significant associations (p > 0.05).
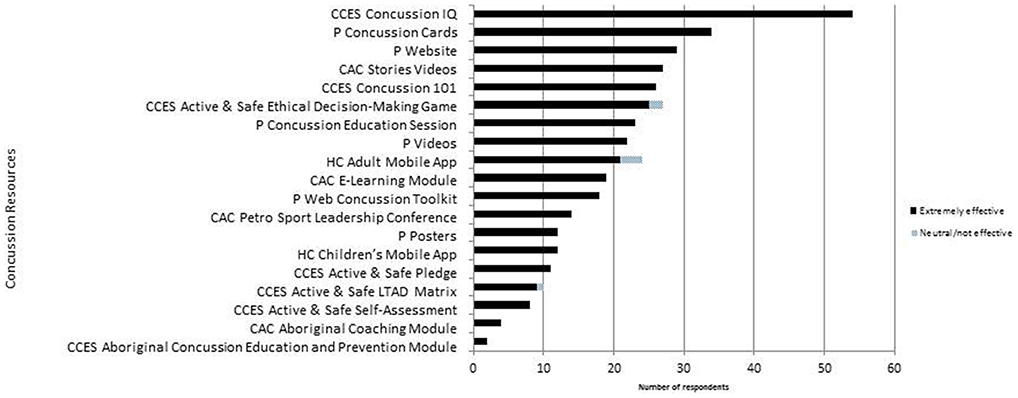
Figure 3. Number of respondents and their perceived effectiveness of the concussion resources evaluated.
Discussion
Main Findings
The results presented illustrate that educational resources delivered at a national level to athletic communities can improve knowledge of concussion. We found that 2 out of 19 resources and 4 out of 6 modes of concussion education delivery were successful in achieving this goal. The webpage educational resource was the most effective mode of delivery concussion knowledge. In addition, our results showed that those who used three or more educational resources had more significant improvements in their concussion knowledge.
Implications
Studies in concussion education have tried various approaches to promote autonomy in online learners (31–33) from written guidelines for athletes, coaches, educators and parents, brochures, quizzes, videos, and websites (34) to tailoring educational interventions to specific needs, skills, preferences, and the culture of the consumer in order to enhance the effectiveness of such educational resources (35). Indeed, autonomous self-regulated learning is emphasized in Piaget's constructivist learning and teaching theory (36) and has been identified as one of the most effective ways to promote behavioral change and active learning, long term (37–39). Yet much remains to be done to change engrained cultural perceptions of concussions and their effects on the individuals, their family and community teaching over time. It takes a community to make changes such as these and stakeholders at all levels that exert an influence on behavior, from the individual, to sport teams, schools, parents, coaches, teams, cities, provinces, and the government of the country in which players reside. Together these bodies of influence could impact greater change and more rapidly than any one level of influence operating alone. Governments through the ministries of education and health, could exert influence through legislation, could collaborate with physician groups to improve levels of education among physicians and other health professionals, school teachers athletic lead trainers. Parents could facilitate collaborations and knowledge translation by becoming engaged at multiple levels of athlete education—schools, clubs, leagues, and provincial and national sports organizations.
The present study supports the need to tailor concussion educational resources for the intended audience but many questions remain unanswered and could be addressed with a larger sample size. For the studied populations, age did not affect their CKS, regardless of the educational resources or mode of delivery used. This may not be the case if very young athletes (e.g., 15 years old or younger) are the targeted population as their knowledge base and reading comprehension are quite different (16). Similarly, income was not a significant predicting factor of CKS for the participants in this study as the group with very low income (< $20,000) was very small (0.9%).
The finding that respondents were able to improve their concussion knowledge in a short period of time suggests these participants may have been motivated learners. According to the health belief model, they may be motivated by (1) the desire to avoid illness, or get well, if they already have had a concussion, and (2) the belief that knowing more about concussion will help prevent or cure it (40). With the learning paradigm shifted from 3 R's (reading, ‘riting, ‘rithmetic) to 4 Es (exposing knowledge, employing information, expressing ideas compellingly, and ethics-right and wrong on the information highway) in the digital era (41), online concussion educational resources are fashioned with several benefits pertaining to eHealth such as avoiding unnecessary delays in receiving the resources and getting advice/new knowledge from authorities (e.g., concussion experts' opinion and up-to-date concussion guidelines) (42) and reaching a large audience (43). Unfortunately, the knowledge gained from such educational interventions may not last for a long time (44), suggesting that such educational efforts should be made on a regular basis or ongoing, and based on our results, combining different formats of delivery can achieve more knowledge gains. Nevertheless, it is important to note that the effectiveness of concussion educational resources doesn't necessarily translate to attitude or behavioral changes (especially in coaches, results not shown), which has been reported in several studies (45–47).
Limitations
Although we had a large sample size, our desire to do a paired analysis restricted that sample size to just over 1,100 responses before and after educational resource exposure. Readers must be cautions interpreting these results as using a voluntary sampling method may exclude certain demographic or ethical groups and using IP addresses as a proxy for the same respondent may overestimate the number of unique respondents. While the results may not be representative of the entire country, Ontario, British Columbia, and Alberta constitute over half of the Canadian population rendering our results some breadth. Since the distribution of concussion education resources was disseminated via online and mobile applications, the targeted audience was limited by the availability and accessibility of survey respondents to the Internet. Another limitation is the possibility that a respondent's improved knowledge regarding concussion education happened on their own accord and did not stem from the use of the concussion resources we presented. This may have posed a maturational threat of internal validity and potentially impacted the outcome of the study. Further, data were not collected for other events that might have influenced levels of knowledge and awareness. Lastly our results could have been influenced by events such as media reporting of concussion or other education initiatives made available throughout the time period of this survey.
Conclusions
Despite these limitations the results presented here have merit and warrant follow up investigations. Our findings demonstrated that the concussion educational resources we provided, based on respondents' results, were able to improve user concussion knowledge. Using three or more educational resources appeared to be more effective than single resources. Future research is needed to evaluate whether implementing these concussion educational resources translate into fewer injuries short and long term.
Ethics Statement
This study was carried out in accordance with the recommendations of Tri-Council Policy Statement guidelines, Research Ethics Board at St. Michael's Hospital with implied informed consent from all subjects. All subjects gave informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Research Ethics Board at St. Michael's Hospital.
Author Contributions
MC was responsible for conception and design as well as analysis and interpretation of the data and revising the manuscript. JT-V, SZ, RJ, AG and GI contributed to the analysis and interpretation of the data as well as revising of the manuscript.
Funding
This research was supported by the Canadian Institutes of Health Research Strategic Team Grant in Applied Injury Research # TIR-103946 (MC), the Ontario Neurotrauma Foundation (MC), and Public Health Agency of Canada (MC).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are thankful to the technical and statistical support from Ling Ge Chen.
References
1. Centers for Disease Control and Prevention. Severe Traumatic Brain Injury [Online] (2014). Available online at: http://www.cdc.gov/TraumaticBrainInjury/severe.html (Accessed March 24, 2017).
2. Rusnak M. Traumatic brain injury: giving voice to a silent epidemic. Nat Rev Neurol. (2013) 9:186–7. doi: 10.1038/nrneurol.2013.38
3. Coronado V, Faul M, Wald MM, Xu L. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths, 2002-2006 [Online] (2010). Atlanta, GA. Available online at: https://www.cdc.gov/traumaticbraininjury/tbi_ed.html (Accessed March 31, 2017).
4. Canadian Institute of Health Research,. New Opportunities in Traumatic Brain Injury Research: Advancing the National Research Agenda [Online]. Toronto, ON (2012). Available online at: http://braininjurycanada.ca/wp-content/uploads/2012/08/New-Opportunities-in-TBI-Research-Workshop-Report.pdf (Accessed March 31, 2017).
5. Do M, Frechette M, McFaull S, Denning B, Ruta M, Thompson W. Injuries in the North–analysis of 20 years of surveillance data collected by the Canadian Hospitals Injury Reporting and Prevention Program. Int J Circumpolar Health (2013) 72. doi: 10.3402/ijch.v72i0.21090
6. Finkelstein E, Corso PS, Miller TR. The Incidence and Economic Burden of Injuries in the United States. Oxford: Oxford University Press (2006).
7. Brooks BL, Mrazik M, Naidu D, Perra A. Exploring minor hockey players' knowledge and attitudes toward concussion: implications for prevention. J Head Trauma Rehabil. (2015) 30:2190227. doi: 10.1097/HTR.0000000000000018
8. Cantu R, Carman AJ, Comstock RD, Dacks PA, DeKosky ST, Ferguson R, et al. Expert consensus document: mind the gaps—advancing research into short-term and long-term neuropsychological outcomes of youth sports-related concussions. Nat Rev Neurol. (2015) 11:230–44. doi: 10.1038/nrneurol.2015.30
9. Robinson DH, Schraw G. Recent Innovations in Educational Technology that Facilitate Student Learning. Charlotte, NC: Information Age Publishing Inc., (2008).
10. Carson JD, Frémont P, Garel A, Law M, Libfeld P, Snow CL, et al. Do family physicians, emergency department physicians, and pediatricians give consistent sport-related concussion management advice? Can Fam Physician. (2014) 60:548–52.
11. Dhandapani KM, Kimbler D, Murphy M. Concussion and the adolescent athlete. J Neurosci Nurs. (2011) 43:1–7. doi: 10.1097/JNN.0b013e31823858a6
12. Hunt T. Video educational intervention improves reporting of concussion and symptom recognition. Athletic Training Educ J. (2015) 10:65–74. doi: 10.4085/100165
13. Kaut KP, DePompei R, Kerr J, Congeni J. Reports of head injury and symptom knowledge among college athletes: implications for assessment and educational intervention. Clin J Sport Med. (2003) 13:213–21. doi: 10.1097/00042752-200307000-00004
14. Cusimano MD, Nastis S, Zuccaro L. Effectiveness of interventions to reduce aggression and injuries among ice hockey players: a systematic review. CMAJ (2013) 185:E57–69. doi: 10.1503/cmaj.112017
15. Sahyouni R, Mahmoodi A, Mahmoodi A, Rajaii RR, Hasjim BJ, Bustillo D, et al. Interactive iBook-based patient education in a neurotrauma clinic. Neurosurgery (2017) 81:787–94. doi: 10.1093/neuros/nyx095
16. Agarwal N, Chaudhari A, Hansberry DR, Tomei KL, Prestigiacomo CJ. A comparative analysis of neurosurgical online education materials to assess patient comprehension. J Clin Neurosci. (2013) 20:1357–61. doi: 10.1016/j.jocn.2012.10.047
17. Caron JG, Bloom GA, Falcao WR, Sweet SN. An examination of concussion education programmes: a scoping review methodology. Inj Prev. (2015) 21:301–8. doi: 10.1136/injuryprev-2014-041479
18. Eagles ME, Bradbury-Squires DJ, Powell MF, Murphy JR, Campbell GD, Maroun FB. The impact of a concussion-U educational program on knowledge of and attitudes about concussion. Can J Neurol Sci. (2016) 43:659–64. doi: 10.1017/cjn.2016.263
19. Schneider DK, Grandhi RK, Bansal P, Kuntz GE, Webster KE, Logan K, et al. Current state of concussion prevention strategies: a systematic review and meta-analysis of prospective, controlled studies. Br J Sports Med. (2017) 51:1473–82. doi: 10.1136/bjsports-2015-095645
20. Hachem LD, Kourtis G, Mylabathula S, Tator CH. Experience with Canada's first policy on concussion education and management in schools. Can J Neurol Sci. (2016) 43:554–60. doi: 10.1017/cjn.2016.41
21. Kroshus E, Daneshvar DH, Baugh CM, Nowinski CJ, Cantu RC NCAA. concussion education in ice hockey: an ineffective mandate. Br J Sports Med. (2014) 48:135–40. doi: 10.1136/bjsports-2013-092498
22. Kroshus E, Baugh CM, Hawrilenko M, Daneshvar DH. Pilot randomized evaluation of publically available concussion education materials: evidence of a possible negative effect. Health Educ Behav. (2015) 42:153–62. doi: 10.1177/1090198114543011
23. Kroshus E, Baugh CM. Concussion education in U.S. collegiate sport: what is happening and what do athletes want? Health Educ Behav. (2016) 43:182–90. doi: 10.1177/1090198115599380
24. Macdonald I, Hauber R. Educating parents on sports-related concussions. J Neurosci Nurs. (2016) 48:297–302. doi: 10.1097/JNN.0000000000000212
25. Williamson RW, Gerhardstein D, Cardenas J, Michael DB, Theodore N, Rosseau N. Concussion 101: the current state of concussion education programs. Neurosurgery (2014) 75(Suppl 4):S131–5. doi: 10.1227/NEU.0000000000000482
26. McKinlay A, Buck K. Misconceptions about traumatic brain injury among educators: has anything changed over the last 20 years? Disabil Rehabil. 1–8. doi: 10.1080/09638288.2018.1429500
27. Taylor AM, Nigrovic LE, Saillant ML, Trudell EK, Modest JR, Kuhn M, et al. Educational Initiative to Standardize Concussion Management in Pediatric Primary Care. Clin Pediatr. 57:806–14. doi: 10.1177/0009922817734363
28. Carroll-Alfano M. Mandated high school concussion education and collegiate athletes' understanding of concussion. J Athl Train (2017) 52:689–97. doi: 10.4085/1062-6050-52.3.08
29. Cusimano M, Zhang S, Topolovec-Vranic J, Hutchison M, Jing R. Factors affecting the concussion knowledge of athletes, parents, coaches, and medical professionals. Sage Open Med. (2017) 4:1–9. doi: 10.1177/2050312117694794
30. Topolovec-Vranic J, Zhang S, Wong H, Lam E, Jing R, Russell K, et al. Recognizing the symptoms of mental illness following concussions in the sports community: a need for improvement. PLoS ONE (2015) 10:e0141699. doi: 10.1371/journal.pone.0141699
31. Ayres P, Paas F, Pachman M. Recent Innovations in Educational Technology that Facilitate Student Learning. Charlotte, NC: Information Age Publishing Inc (2008).
32. Malone TW. Toward a theory of intrinsically motivating instruction. Cogn Sci. (1981) 5:333–69. doi: 10.1207/s15516709cog0504_2
33. U. S Department of Health and Human Services Office of Disease Prevention and Health Promotion. Six Strategies for Writing and Designing Easy-to-Use Health Web Sites [Online]. (2010). (Accessed March 24, 2017). Available online at: https://health.gov/healthliteracyonline/
35. Jordan-Marsh M. Health Technology Literacy: A Transdisciplinary Framework for Consumer-Oriented Practice. Sudbury, MA: Jones and Bartlett Learning LLC (2011).
38. Harari P, Legge K. Heinemann Themes in Psychology: Psychology and Education. Oxford: Heinemann Educational Publishers (2000).
39. McLeod S. Bandura-Social Learning Theory [Online]. (2011). Available online at: http://www.simplypsychology.org/bandura.html (Accessed March 31, 2017).
40. Boston University School of Public Health (2013). Behavioral Change Models [Online]. Available online at: http://sphweb.bumc.bu.edu/otlt/MPH-Modules/SB/BehavioralChangeTheories/BehavioralChangeTheories_print.html (Accessed March 31, 2017).
41. Armstrong S, Warlick D. The New Literacy [Online] (2004). Available online at: http://www.techlearning.com/news/0002/the-new-literacy/57197 (Accessed March 31, 2017).
42. Baur C, Kanaan SB. Expanding the Reach and Impact of Consumer E-Health Tools [Online]. (2006). Available online at: http://health.gov/communication/ehealth/ehealthtools/pdf/ehealthreport.pdf (Accessed March 31, 2017).
43. Parker EM, Gilchrist J, Schuster D, Lee R, Sarmiento K. Reach and knowledge change among coaches and other participants of the online course: “concussion in sports: what you need to know.” J Head Trauma Rehabil. (2015) 30:198–206. doi: 10.1097/HTR.0000000000000097
44. Cusimano MD, Chipman M, Donnelly P, Hutchison MG. Effectiveness of an educational video on concussion knowledge in minor league hockey players: a cluster randomised controlled trial. Br J Sports Med. (2014) 48:141–6. doi: 10.1136/bjsports-2012-091660
45. Kerr ZY, Register-Mihalik JK, Marshall SW, Evenson KR, Mihalik JP, Guskiewicz KM. Disclosure and non-disclosure of concussion and concussion symptoms in athletes: review and application of the socio-ecological framework. Brain Inj. (2014) 28:1009–21. doi: 10.3109/02699052.2014.904049
46. Register-Mihalik JK, Guskiewicz KM, McLeod TC, Linnan LA, Mueller FO, Marshall SW. Knowledge, attitude, and concussion-reporting behaviors among high school athletes: a preliminary study. J Athl Train (2013) 48:645–53. doi: 10.4085/1062-6050-48.3.20
47. Register-Mihalik JK, Linnan LA, Marshall SW, Valovich McLeod TC, Mueller, FO, Guskiewicz KM. Using theory to understand high school aged athletes' intentions to report sport-related concussion: implications for concussion education initiatives. Brain Inj. (2013) 27:878–86. doi: 10.3109/02699052.2013.775508
Keywords: concussion, mild traumatic brain injury (mTBI), concussion education and awareness programs, concussion prevention, sports injury prevention
Citation: Cusimano MD, Zhang S, Topolovec-Vranic J, Grosso A, Jing R and Ilie G (2018) Pros and Cons of 19 Sport-Related Concussion Educational Resources in Canada: Avenues for Better Care and Prevention. Front. Neurol. 9:872. doi: 10.3389/fneur.2018.00872
Received: 09 December 2017; Accepted: 27 September 2018;
Published: 02 November 2018.
Edited by:
Mårten Risling, Karolinska Institutet (KI), SwedenReviewed by:
Ralph George Depalma, United States Department of Veterans Affairs, United StatesNancy D. Chiaravalloti, Kessler Foundation, United States
Copyright © 2018 Cusimano, Zhang, Topolovec-Vranic, Grosso, Jing and Ilie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriela Ilie, R2FicmllbGEuSWxpZUBkYWwuY2E=
 Michael D. Cusimano
Michael D. Cusimano Stanley Zhang
Stanley Zhang Jane Topolovec-Vranic3
Jane Topolovec-Vranic3 Rowan Jing
Rowan Jing Gabriela Ilie
Gabriela Ilie