
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Neurol. , 28 September 2018
Sec. Headache and Neurogenic Pain
Volume 9 - 2018 | https://doi.org/10.3389/fneur.2018.00819
This article is part of the Research Topic Clinical and Pathophysiological Peculiarities of Headache in Children and Adolescents View all 12 articles
 Romina Moavero1,2*
Romina Moavero1,2* Giorgia Sforza2
Giorgia Sforza2 Laura Papetti1
Laura Papetti1 Barbara Battan1
Barbara Battan1 Samuela Tarantino1
Samuela Tarantino1 Federico Vigevano1
Federico Vigevano1 Massimiliano Valeriani1,3
Massimiliano Valeriani1,3Idiopathic intracranial hypertension (IIH) is characterized by intracranial pressure >28 cmH2O in the absence of identifiable causes. Aim of this paper is to describe the clinical phenotype of pediatric IIH and to analyze the applicability of ICHD-3 criteria in comparison to the ICHD-2. We conducted a retrospective analysis of full clinical data of pediatric patients diagnosed with IIH between January 2007 and June 2018. Diagnostic evaluation included neuroimaging (all patients) and ultrasound-based optic nerve sheath diameter measurement (9 patients). Diagnosis of IIH was verified according to both ICHD-2 and ICHD-3 criteria for headache attributed to IIH, to verify the degree of concordance. We identified 41 subjects with suspected IIH; 14 were excluded due a diagnosis of secondary IH or lack of data. We therefore selected 27 subjects (age 4–15 years, mean 11). All patients presented with headache and bilateral papilloedema. Headache was daily in 22% cases, with diffuse gravative pain in 41%. In 4%, pain was exacerbated by cough, stress or tension. The most common presentation symptoms, in addition to headache, were blurred vision or diplopia (70%), vomiting (33%), and dizziness (15%). Twenty patients (74%) were obese. In 6 patients (22%) neuroimaging showed empty sella. Optic nerve sheath distension was detected in 6 out of 9 patients. Regarding the applicability of the ICHD-2 criteria, 18/27 (71%) patients have criterion A; 24/27 (89%) criterion B; 27/27 (100%) criterion C; 27/27 (100%) criterion D. When the ICHD-3 criteria were used, 27/27 (100%) fitted criterion A; 24/27 (89%) criterion B; 27/27 (100%) criterion C; and 27/27 (100%) criterion D. Our study suggests that, as compared with the ICHD-2, the new ICHD-3 criteria for headache attributed to IIH are better satisfied by pediatric patients with IIH. This is mainly due to the fact that qualitative headache characteristics are no longer considered in ICHD-3. Although the risk of under-rating the symptom of headache in IIH should not be disregarded, in pediatric population headache characteristics are usually less defined than in adults and obtaining a precise description of them is often very difficult.
Idiopathic intracranial hypertension (IIH), also known as pseudotumor cerebri syndrome (PTC), is a rare pediatric neurological disorder (1). It is characterized by increased intracranial pressure (ICP) in the absence of any brain parenchymal lesions, vascular malformations, hydrocephalus, or central nervous system (CNS) infection (2). The diagnosis is usually confirmed by high opening pressure (OP) of cerebrospinal liquid (CSF) (more than 25 cm H2O), provided there are no secondary causes of intracranial hypertension. In 2013, the opening pressure (OP) for children aged from 1 to 18 years of age was redefined, and the upper limit for a normal OP is actually 28 cm H2O in the pediatric population (1, 3).
IIH is more frequent in females (females-males ratio 4:1), especially in the reproductive age, with overweight being a significant adjunctive risk factor. Indeed, in fertile age overweight females, the estimated incidence is 12–20 per 100,000 people per year, vs. a general incidence in the adult population of 0.5–2 per 100,000 (4, 5). The exact prevalence of IIH in the pediatric population is not yet well established. Recently, studies from the United Kingdom applying the Friedman criteria revealed an annual incidence of 0.71 per 100,000 (1, 6).
The pathogenesis of IIH is still largely unknown. ICP is determined by the balance between production and absorption of CSF. According to the Monro-Kellie rule, an increase in ICP might be related to increased CSF, expanded brain tissue, or increased blood volume (7). Proposed hypotheses include excess of CSF production, CSF outflow reduction, increase in cerebral blood volume and/or brain water content, obstruction to venous system, endocrinological or metabolic causes, chronic inflammation, and obesity (in pre- and post-pubertal females) (8–15).
The characteristic signs and symptoms of IIH were initially described by Dandy and were later organized into the Modified Dandy Criteria by Smith, combining the lack of other causes of increased ICP (such as neoplasms and cerebral venous sinus thrombosis—CVST), with the presence of the following features: symptoms of increased ICP, papilloedema and raised opening cerebrospinal fluid (CSF) pressure at lumbar puncture (LP) (16) (see Table 1). In 2013, revised diagnostic criteria for IIH have been published by Friedman and coworkers, not including symptoms of raised ICP (Table 2) (3). According to these revised criteria, IIH can be classified as “definite” (increased OP and either papilloedema or abducens nerve palsy), “probable” (normal CSF pressure in presence of papilloedema), or “suggestive of” (raised CSF pressure plus at least three valid neuroimaging markers of raised ICP, in the absence of papilloedema and abducens nerve palsy) (3).
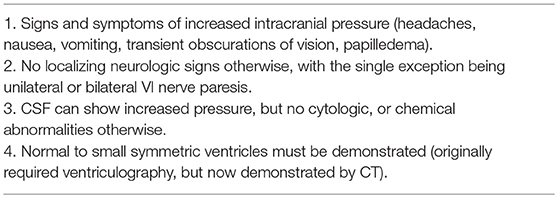
Table 1. Modified Dandy Criteria (16).
Headache is the most common presentation symptom of IIH. However, the characteristics of the headache in IIH patients are widely variable and not specific to IIH. Headache is often referred as unusually severe and can be lateralized and throbbing or pulsatile. It can be intermittent or persistent, occurring daily or less frequently, and nausea and vomiting can be present. Headache can be exacerbated by posture changes, and some patients may report relief with non-steroidal anti-inflammatory drugs and/or rest, although drug refractoriness is common. Therefore, in most cases, headache characteristics are similar to migraine and tension-type headache (17). If retrobulbar pain and pain with eye movement or globe compression are present, they can be highly suggestive of IIH (17). Since headache may be the main symptom of changes in ICP, diagnostic criteria for “Headache attributed to IIH” have been published by the Headache Classification Committee of the International Headache Society (IHS) in the second international classification of migraine disorders in 2004 and subsequently modified in 2018 in the third classification (18, 19) (Tables 3, 4). Some patients, especially younger children, might present intracranial hypertension without headache (20). In the absence of headache, the diagnosis is often suggested by accidental finding of papilloedema during routine ophthalmologic evaluations.
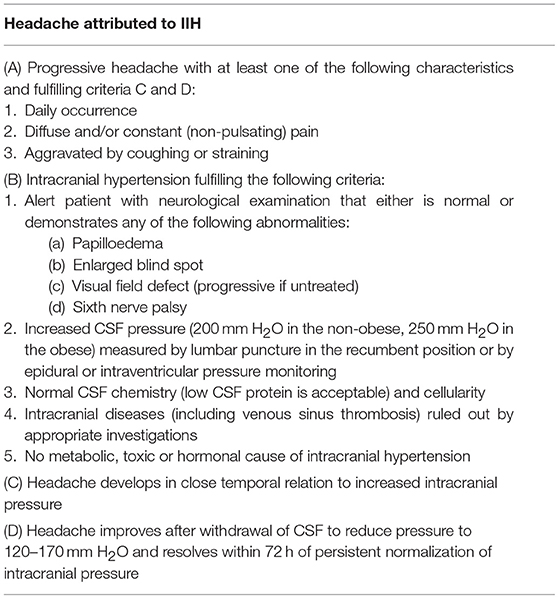
Table 3. ICHD-2 criteria for headache attributed to IIH (19).
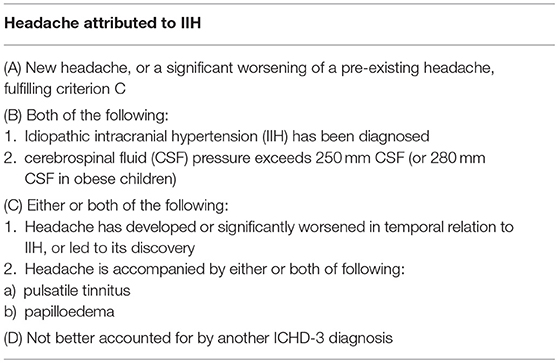
Table 4. ICHD-3 criteria for headache attributed to IIH (18).
The aim of this study was to analyze the applicability of the new ICHD-3 criteria in comparison to the ICHD-2 criteria in a sample of pediatric patients suffering from headache attributed to IIH.
We retrospectively analyzed clinical, laboratory, and neuroimaging data of pediatric patients admitted for headache and finally diagnosed with IIH in the Headache Center of Bambino Gesù Children's Hospital between January 2007 and June 2018. Patients with incomplete data for whom a complete verification of diagnosis was not possible were not included in the present study. Also patients with secondary IH have been excluded. Diagnostic evaluation included neuroimaging studies for all patients, and in some cases ultrasound-based optic nerve sheath diameter (ONSD) measurement. All patients/parents/caregivers have been contacted by phone to evaluate whether they suffered from headache before the acute episode, and to understand if clinical characteristics presented some differences.
In all patients diagnosis of IIH was verified both according to ICHD-2 and ICHD-3 criteria for headache attributed to IIH, to verify the degree of concordance.
We identified a total of 41 subjects diagnosed with IIH. Four patients have been excluded due to the identification of possible causes of IH (including cyclosporin therapy and hypoparathyroidism); 10 patients received a clinical diagnosis based on the presence of headache, papilloedema, and obesity, but have been excluded due to lack of data (lumbar puncture not performed or data not available). We therefore selected 27 subjects (15 F, 12 M), ranging between 4 and 15 years of age (mean age 11 years). All patients presented with headache and physical examination revealed the presence of bilateral papilloedema in all of them. Only 3 of them (patients #3, #10, #19) reported a previous history of headache, but in all of them pain characteristics were quite different with more severe symptoms and unsatisfactory response to analgesic treatment. Despite clinical features were highly suggestive for IIH in all patients, in 3 of them the opening pressure of CSF was < 25 cmH2O thus not satisfying all criteria for the diagnosis of IIH. As for headache characteristics, it was daily in 22% of cases, with diffuse gravative pain in 41% of cases, while throbbing headache was present in 15% of patients. Moreover, in 4% of patients, headache was exacerbated by cough, stress or tension, and in 11% it had a unilateral distribution. The most common presentation symptoms, in addition to headache, were blurred vision or diplopia (70%), vomiting (33%), and dizziness (15%). Twenty patients (74%) were obese (weight centile ≥ 90%).
In the majority of patients neuroimaging was normal, while in 6 patients (22%), MRI or CT showed signs of empty sella syndrome. Ultrasound-based ONSD measurement was obtained only in 9 patients, in six of whom an optic nerve sheath distension could be demonstrated. Clinical characteristics of our sample are summarized in Table 5.
Regarding the applicability of the ICHD-2 criteria, 18/27 (71%) patients have criterion A; 24/27 (89%) criterion B; 27/27 (100%) criterion C; 27/27 (100%) criterion D. When ICHD-3 criteria were used, 27/27 patients (100%) fitted criterion A; 24/27 (89%) criterion B; 27/27 (100%) criterion C; and 27/27 (100%) criterion D.
To the best of our knowledge, this is the first study comparing the applicability of the new ICHD-3 criteria to pediatric headache attributed to IIH. According to the results obtained by our study, the new ICHD-3 criteria seem to be applicable and valid for a higher rate of subjects clinically presenting with symptoms suggestive of IIH. In particular, in our clinical series, the difference was evident in the criterion A, which was fulfilled by all patients when applying ICHD3, but only by 71% when considering the old ICHD2 version. Certainly, this is due to the disappearance of specificity criteria for the headache, which now is no longer required to be daily, diffuse, and/or aggravated by cough or straining. Although this might be considered as a worse reliability and as a risk of under-rating headache as a symptom in IIH (21), it should be underlined that in pediatric population headache characteristics are usually less defined than in adults. Moreover, in younger children obtaining a precise description of headache characteristics could be very difficult. In the ICHD-3, it is only requested that headache must be “new” or show a “significant worsening.” This latter expression, according to ICHD-3 specifications, implies at least a double increase in frequency and/or severity of headache. An objective evaluation of a significant worsening was present in all the 3 patients presenting a previous history of migraine, however it could be difficult to be ascertained in younger patients. The ICHD-3 criterion C states that the new or worsened headache leads to the discovery of IIH, thus helping in evaluating the fulfillment of this criterion. Summarizing, the significant change in criterion A with the abolition of precise qualitative characteristics defining headache could help to include a higher rate of pediatric patients presenting with signs and symptoms suggestive of IIH. Another important difference between ICHD versions 2 and 3 is represented by the increase of ICP cut-off in criterion B, keeping a difference between patients with and without obesity. However, in our sample, although limited, this modification did not determine any difference.
A main feature of the ICHD-2 diagnostic criteria was relief from headache after CSF withdrawal, but this was removed in the recently published ICHD-3 criteria. In our series, all patients had an improvement in symptoms after lumbar puncture and CSF withdrawal, but this can be seen also in patients with other types of headache (presenting a sensitivity and specificity of 72 and 77%, respectively). This criterion has been replaced by the criterion according to which headache should be “no better accounted for by another ICHD-3 diagnosis.” This appeared to be a necessary specification since headache secondary to IIH can be really overlapping to chronic migraine or chronic tension-type headache. Indeed, these disorders often coexist with IIH, and in all patients still complaining of headaches after treatment, migraine should be considered in order to use appropriate treatment and prevent unnecessary overtreatment for suspected IIH relapses (22).
This retrospective study received approval by the Local Ethical Board of Bambino Ges Children's Hospital, IRCCS, Rome, Italy.
RM and MV conceived and wrote the paper. MV, GS, LP, BB, and ST collected the data. RM and GS analyzed the data. FV and MV revised the paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Cleves-Bayon C. Idiopathic intracranial hypertension in children and adolescents: an update. Headache (2018) 58:485–93. doi: 10.1111/head.13236
2. Albakr A, Hamad MH, Alwadei AH, Bashiri FA, Hassan HH, Idris H, et al. Idiopathic intracranial hypertension in children: diagnostic and management approach. Sudan J Paediatr. (2016) 16:67–76.
3. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology (2013) 81:1159–65. doi: 10.1212/WNL.0b013e3182a55f17
4. Kesler A, Gadoth N. Epidemiology of idiopathic intracranial hypertension in Israel. J Neuroophthalmol. (2001) 21:12–4. doi: 10.1097/00041327-200103000-00003
5. Raoof N, Sharrack B, Pepper IM, Hickman SJ. The incidence and prevalence of idiopathic intracranial hypertension in Sheffield, UK. Eur J Neurol. (2011) 18:1266–8. doi: 10.1111/j.1468-1331.2011.03372.x
6. Matthews YY, Dean F, Lim MJ, McLachlan K, Rigby AS, Solanki GA, et al. Pseudotumor cerebri syndrome in childhood: incidence, clinical profile and risk factors in a national prospective population-based cohort study. Arch Dis Child. (2017) 102:715–21. doi: 10.1136/archdischild-2016-312238
7. Walker RW. Idiopathic intracranial hypertension: any light on the mechanism of the raised pressure? J Neurol Neurosurg Psychiatry (2001) 71:1–5. doi: 10.1136/jnnp.71.1.1
8. Dandy WE. Intracranial pressure without brain tumor: diagnosis and treatment. Ann Surg. (1937) 106:492–513. doi: 10.1097/00000658-193710000-00002
10. Oldstone MB. Disturbance of pituitary-adrenal interrelationships in benign intracranial hypertension (pseudotumor cerebri). J Clin Endocrinol Metab. (1966) 26:1366–9. doi: 10.1210/jcem-26-12-1366
11. Calabrese VP, Selhorst JB, Harbison JW. CSF infusion test in pseudotumor cerebri. Trans Am Neurol Assoc. (1978) 103:146–50.
12. Donaldson JO. Pathogenesis of pseudotumor cerebri syndromes. Neurology (1981) 31:877–80. doi: 10.1212/WNL.31.7.877
13. Mokri B. The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology (2001) 56:1746–8. doi: 10.1212/WNL.56.12.1746
14. Bateman GA, Smith RL, Siddique SH. Idiopathic hydrocephalus in children and idiopathic intracranial hypertension in adults: two manifestations of the same pathophysiological process? J Neurosurg. (2007) 107(Suppl. 6):439–44. doi: 10.3171/PED-07/12/439
15. Dhungana S, Sharrack B, Woodroofe N. Cytokines and chemokines in idiopathic intracranial hypertension. Headache (2009) 49:282–5. doi: 10.1111/j.1526-4610.2008.001329.x
17. Wall M. The headache profile of idiopathic intracranial hypertension. Cephalalgia (1990) 10:331–5. doi: 10.1046/j.1468-2982.1990.1006331.x
18. Headache Classification Subcommittee of the International Headache S. The International Classification of Headache Disorders: 2nd edition. Cephalalgia (2004) 24 (Suppl. 1):9–160.
19. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia (2018) 38:1–211.
20. Lim M, Kurian M, Penn A, Calver D, Lin JP. Visual failure without headache in idiopathic intracranial hypertension. Arch Dis Child. (2005) 90:206–10. doi: 10.1136/adc.2003.039305
21. Curone M, Peccarisi C, Bussone G. Headache attributed to intracranial pressure alterations: applicability of the International Classification of Headache Disorders ICHD-3 beta version versus ICHD-2. Neurol Sci. (2015) 36 (Suppl. 1):137–9. doi: 10.1007/s10072-015-2202-5
Keywords: pseudotumor cerebri, idiopathic intracranial hypertension, papilloedema, children, adolescents, ICHD-2, ICHD-3
Citation: Moavero R, Sforza G, Papetti L, Battan B, Tarantino S, Vigevano F and Valeriani M (2018) Clinical Features of Pediatric Idiopathic Intracranial Hypertension and Applicability of New ICHD-3 Criteria. Front. Neurol. 9:819. doi: 10.3389/fneur.2018.00819
Received: 08 June 2018; Accepted: 10 September 2018;
Published: 28 September 2018.
Edited by:
Tim P. Jürgens, Universitätsmedizin Rostock, GermanyReviewed by:
Gudrun Gossrau, Universitätsklinikum Carl Gustav Carus, GermanyCopyright © 2018 Moavero, Sforza, Papetti, Battan, Tarantino, Vigevano and Valeriani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Romina Moavero, cm9taW5hbW9hdmVyb0Bob3RtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.