- Department of Neurology, China-Japan Union Hospital of Jilin University, China
Background: Levodopa has been widely used and regarded as the most effective therapy for Parkinson's disease (PD), but long-term treatment with oral levodopa may result in motor fluctuations and involuntary movements (dyskinesias). There is evidence to suggest that Continuous infusion of levodopa-carbidopa intestinal gel (LCIG) can effectively manage motor and non-motor complications in PD, but clinical studies investigating this have yielded inconsistent results. This systematic review and meta-analysis was performed to examine the efficacy and safety of LCIG for patients with PD.
Methods: A systematic search was conducted to retrieve published data in the EMBASE, PubMed, and the Cochrane Library up to March 2018. Both efficiency and safety of LCIG were analyzed using pooled standardized mean differences (SMDs) or odds ratio (ORs) with 95% confidence interval (CIs).
Results: Eight trials with 384 PD patients were included in the present study. Compared with the control group, LCIG significantly decreased off-time (SMD, −1.19; 95% CI, −2.25 to −0.12; p = 0.003) and increased on-time without troublesome dyskinesia (SMD, 0.55; 95% CI, 0.20 to 0.90; p = 0.002). However, no significant difference of LCIG was found in on-time with troublesome dyskinesia. There were no significant differences in UPDRS, Hoehn & Yahr and PDQ-39 scores. Besides, no significant differences in the drop-out and adverse effects.
Conclusions: Continuous delivery of LCIG may offer a promising option for PD patients. More randomized double-blind controlled studies with large sample sizes were needed to further confirm the efficacy and safety of LCIG for PD patients.
Introduction
Parkinson's disease (PD) is the second most common chronic neurodegenerative diseases characterized by resting tremor, bradykinesia, rigidity, and postural instability. About 1% of the subjects aged over 60 years suffer from PD worldwide (1, 2). According to the survey from National Parkinson's Foundation in 2010, there were ~1 million patients suffering from PD and 50,000 to 60,000 new cases that are diagnosed with PD every year in the USA. The prevalence of PD for people aged over 65 years was 1.7% in China (3) and it is predicted to increase because of the population aging.
Levodopa is the amino-acid precursor of dopamine and replenishes the depleted striatal dopamine. Since more than 40 years, levodopa has been widely used as the most effective treatment for advanced Parkinson's disease (4–6). However, due to its short plasma half-life, oral levodopa may cause pulsatile striatal receptor stimulation, and thereby lead to dyskinesias, troublesome motor fluctuations, and unpredictable swings from mobility to immobility (7, 8). Levodopa-carbidopa intestinal gel (LCIG) was developed by using a percutaneous pump and helps to offer more continuous dopaminergic stimulation and leads to more constant plasma levels of levodopa (9). Clinical evidence suggests that LCIG results in significant decrease in off-time and on-time with troublesome dyskinesias and motor fluctuations (10–12). Surgical- or device-related complications are the most common side effects, but there are also anecdotal reports on neuropathy in LCIG-treated patients (13).
In recent years, increasing evidence has described the pharmacokinetics (14–16), efficacy and safety after LCIG treatment in patients with PD (12–14, 17–27). However, these results are variable and controversial. No clear consensus has been reached on the efficacy and safety of LCIG. Therefore, we performed this systematic review and meta-analysis to investigate the efficacy, safety, and tolerability of LCIG for PD patients based on the reported evidence.
Materials and Methods
Search Strategy
A comprehensive literature search was performed to collect the potential reports in electronic databases PubMed, Embase, and the Cochrane Library up to March 2018. The reference lists of retrieved studies were also reviewed and identified. Both subject terms and free terms were used in the search progress, including “Parkinson disease,” “Parkinson's,” “carbidopa,” “levodopa,” “gel,” and “intestines.” No study types were restricted during the search. No language restrictions were set.
Eligibility Criteria
Studies were eligible when they met the following entry criteria: (1) patients with Parkinson's disease; (2) exposure to LCIG; (3) studies with a control group; (4) sample size > 10; (5) reported the efficacy and/or safety of LCIG after treatment. No sex and ethnicity of patients were restricted. These eligibility criteria were verified based on the search results.
Data Extraction
Two review authors independently performed the data extraction from included trials. The information included (1) the first author and publication date, (2) study design, (3) treatment arms, (4) the country where the study conducted, (5) sample size and the sex ratio, (6) treatment duration, (7) outcomes of interest, and (8) main findings of each selected trial. For the outcomes, we further collected the following parameters: on time, off time, UPDRS, Hoehn & Yahr, PDQ-39, and adverse effects. The disagreement between two reviewers was resolved by discussion with another author.
Quality Assessment
Two authors evaluated the quality of each study included in this meta-analysis. The standard scoring criteria proposed by the Cochrane Back Review Group (28) were used for the four RCTs, and the Newcastle-Ottawa Quality Assessment Form (29) was used to for the other four cohort studies. The scoring criteria for RCTs included five domains, i.e., (1) selection bias, (2) performance bias, (3) attrition bias, (4) reporting bias, and (5) outcome assessor blinding and timing of outcome assessment. There are 12 items which scored a total of 12 points. A study scored more than 8 points was regarded as a high-quality study. A study scored fewer than 5 points was regarded as a low-quality study. The Other studies can be regarded as moderate-quality studies.
The Newcastle-Ottawa Quality Assessment Form included three domains, i.e., selection (4 points), comparability (2 points), and outcome (3 points). There are 12 items which scored a total of 12 points. A high-quality study scored more than 7, whereas a low-quality study scored less than 6. Other studies scored 6–7 were rated as a moderate grade. Uncertainty or disagreement was resolved by discussion to reach a consensus.
Outcome Measures
This meta-analysis focused on the efficacy and safety of LCIG for PD. The primary efficacy outcomes were the changes in ON time and OFF time; secondary endpoints were the changes in UPDRS, Hoehn & Yahr, and PDQ-39. Safety outcomes included the incidences of adverse event (AE) and serious AEs, and treatment withdrawal for any reasons and for AEs. Other parameters of pharmacokinetics and laboratory tests were narratively reviewed.
Statistical Analysis
Chi-squared test and the I2 statistics were used for the assessment of heterogeneity among the included studies (2, 30, 31). When I2 ≥ 50% or p ≤ 0.1, there was a significant heterogeneity and a random-effects model was utilized. Otherwise, a fixed-effects model was adopted when I2 < 50%. For continuous variables, standardized mean differences (SMDs), which are more suitable than weighted mean differences (WMDs) when the mean differences were large across studies (32), and the 95% confidence intervals (CIs) were used. For dichotomous outcomes, pooled odds ratios (ORs) and corresponding 95% CIs were calculated for the measurement of differences compared with control groups. Data analysis was performed using a Review Manager software, version 5.3 for Windows (Cochrane Collaboration, Oxford, United Kingdom). Reported probability values were two-sided, with significance set at p ≤ 0.05. We did not perform the sensitivity analyses because of the limited number of eligible articles (33).
Results
Study Selection
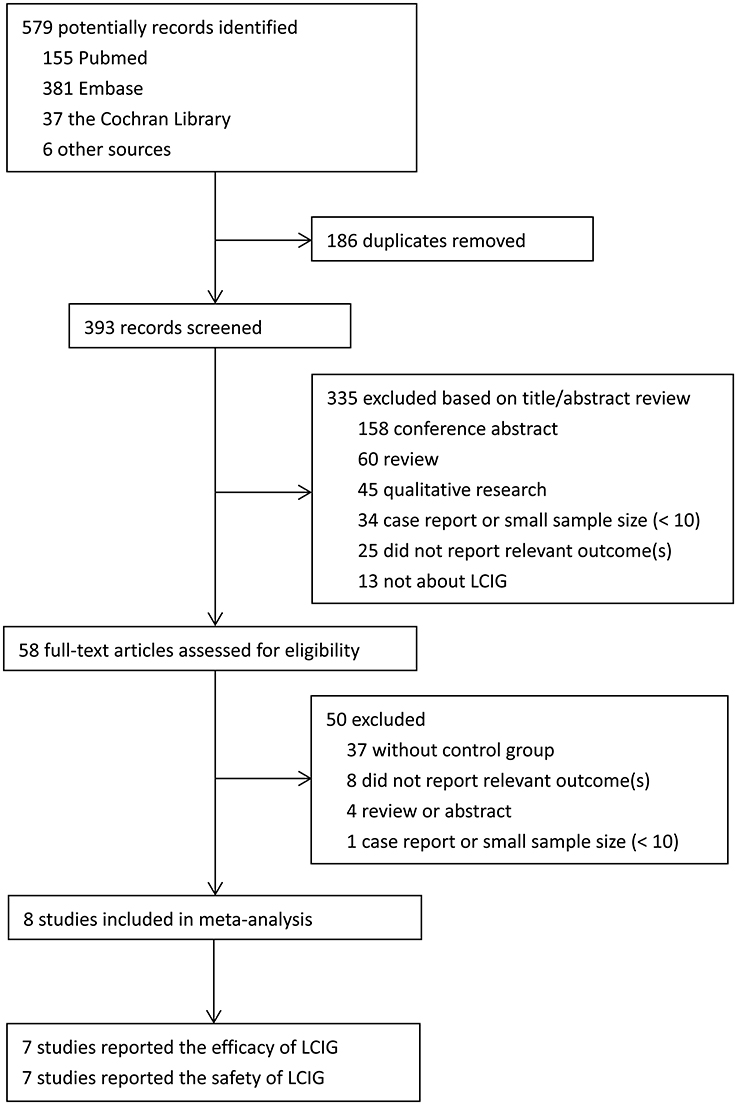
Literature selection process was performed as shown in the PRISMA flow diagram (Figure 1). Briefly, a total of 579 studies were collected from various electronic databases and the reference lists of retrieved studies. Then EndNote X7 software was used for the removal of duplicated studies. The potential studies were screened by two authors based on the title/abstract. They further identified the selected studies by reading the full text. The disagreements were discussed with a third author to reach a consensus. Finally, eight trials with 384 Parkinson's disease patients were included in the present meta-analysis (12, 14, 17, 18, 21, 23, 24, 27). Among them, seven studies reported the efficacy of LCIG (12, 14, 17, 18, 21, 23, 24), and seven studies reported the safety of LCIG (12, 14, 17, 21, 23, 24, 27).
Study Characteristics
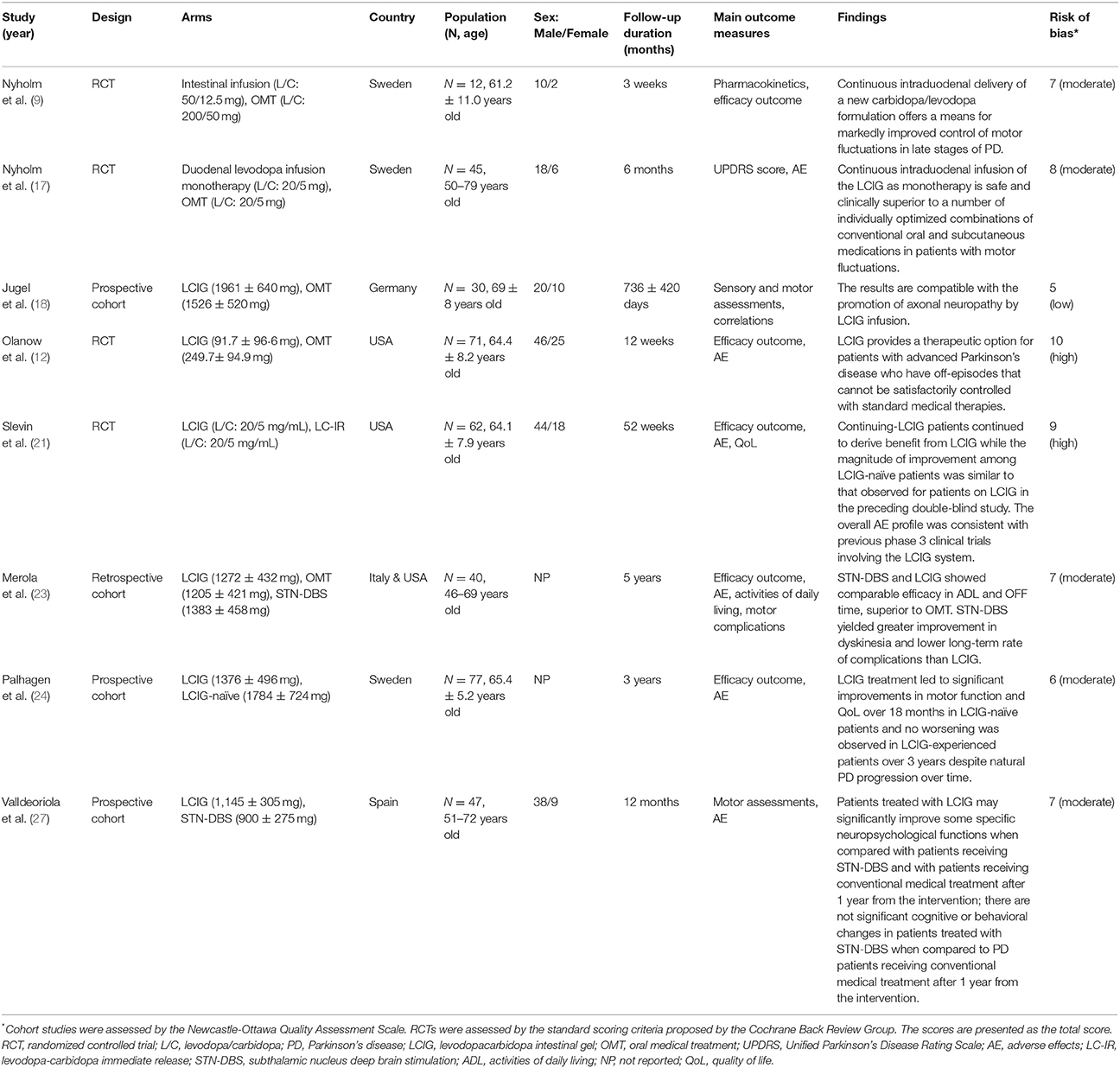
The characteristics of included trials were shown in Table 1. All studies were RCTs (12, 14, 17, 21) or cohorts (18, 23, 24, 27) published between 2003 and 2017. Most studies compared the LCIG with oral medical treatment (12, 14, 17, 18, 21, 23), while one study compared the LCIG with subthalamic nucleus deep brain stimulation. Three of the studies were performed in Sweden (14, 17, 24), two in USA (12, 21), one in Germany (18), one in Spain (27), and one in both USA and Italy (23). All patients were suffered from advanced PD and were treated with LCIG. Interestingly, there were a lot more male patients than female patients in most included studies. The treatment duration was varied from 3 weeks to 5 years. Besides the efficacy and safety of LCIG, some included studies also reported the pharmacokinetics changes. Most included studies showed that LCIG was a safe therapeutic option for PD patients.
Study Quality
In general, a randomized controlled trial (RCT) has higher quality compared with an observational study. Study quality of RCTs was evaluated by using an assessment scale proposed by the Cochrane Back Review Group, and the results of risk of bias were presented in Table 1. Two RCTs were classified as high quality (12, 21), and the other two RCTs were classified as moderate quality (14, 17). The qualified trials scored ranging from 7 to 10. For the other four cohort studies evaluated by Newcastle-Ottawa Quality Assessment Form, two studies (23, 27) scored 7 points and one study (24) scored 6 points, which could be regarded as at moderate-quality. While one study only (18) scored 5 points, and could be regarded as at low-quality. Thus, most included studies were deemed to be of the moderate or high quality, except one (18). Most RCTs lost points because of the lack of blinding and adequate random sequence generation. While most cohort studies lost points because of a statement of the outcome of interest at the beginning and non-blind outcome assessment.
On-Time and Off-Time
Two studies reported on-time with/without troublesome dyskinesia (12, 21), involving 133 PD patients following LCIG. While three studies reported the off-time (12, 21, 23), involving 173 PD patients following LCIG. As shown in Figure 2, no notable heterogeneity was found in on-time with/without troublesome dyskinesia (I2 = 0%, p = 0.73; I2 = 0%, p = 0.34), while a notable heterogeneity was found in off-time (I2 = 90%, p < 0.0001). There was no significant difference in on-time with troublesome dyskinesia (SMD, −0.06; 95% CI, −0.40 to 0.28; p = 0.71) between control and LCIG group (Figure 2A). However, Significant differences were found in on-time without troublesome dyskinesia (SMD, 0.55; 95% CI, 0.20 to 0.90; p = 0.002; Figure 2B) and off-time (SMD, −1.19; 95% CI, −2.25 to −0.12; p = 0.003; Figure 2C), which suggested the positive effects of LCIG.
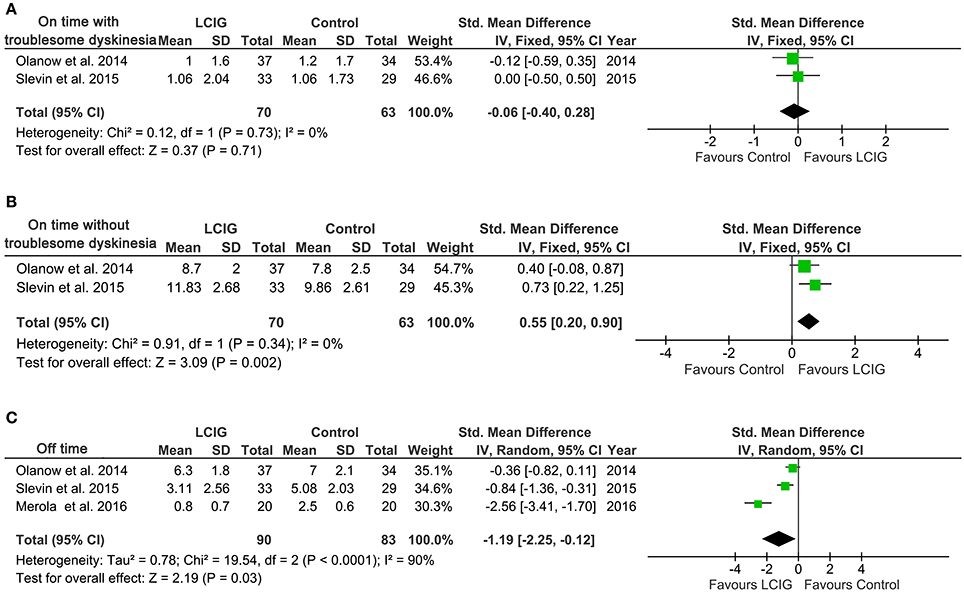
Figure 2. Forest plots of pooled on-time and off-time in PD patients. Plot A (A), on-time with troublesome dyskinesia, h per day; plot B (B), on-time without troublesome dyskinesia, h per day; plot C (C), off-time, h per day. PD, Parkinson's disease; LCIG, levodopa-carbidopa intestinal gel.
UPDRS
For UPDRS, five studies with 204 PD patients reported UPDRS total score (14, 17, 21, 23, 24) and other five studies with 259 PD patients reported UPDRS part II and part III (12, 17, 21, 23, 24). A notable heterogeneity was found in UPDRS total score (I2 = 68%, p = 0.01) and UPDRS part II (I2 = 74%, p = 0.004), while no significant heterogeneity was found in UPDRS part III (I2 = 30%, p = 0.22). Therefore, a random-effects model was used for UPDRS total score and UPDRS part ?, while a fixed-effects model was used for UPDRS part II. The pooled results showed that LCIG did not significantly improve UPDRS total score and UPDRS part II and part III (all p > 0.05; Figure 3).
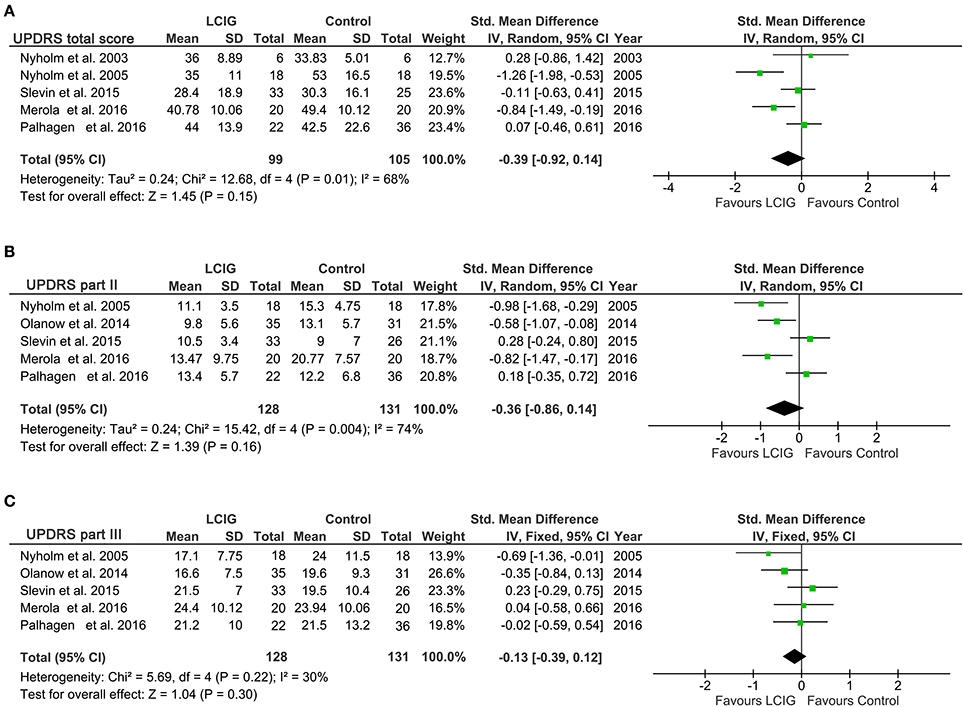
Figure 3. Forest plots of pooled UPDRS scores in PD patients. Plot A (A), UPDRS total scores; plot B (B), UPDRS part II; plot C (C), UPDRS part III. PD, Parkinson's disease; LCIG, levodopa-carbidopa intestinal gel.
PDQ-39
We analyzed PDQ-39 from three studies with 182 patients. The comparisons of PDQ-39 presented a significant heterogeneity among the studies, as was evident from I2 = 59%, p = 0.09 (Figure 4A). Thus, a random-effects model was adopted in this comparisons. Pooling trials that reported PDQ-39 got an SMD of −0.18 and 95% CI of −0.64 to 0.28, which was not a significant effect in favor of LCIG (p = 0.45).
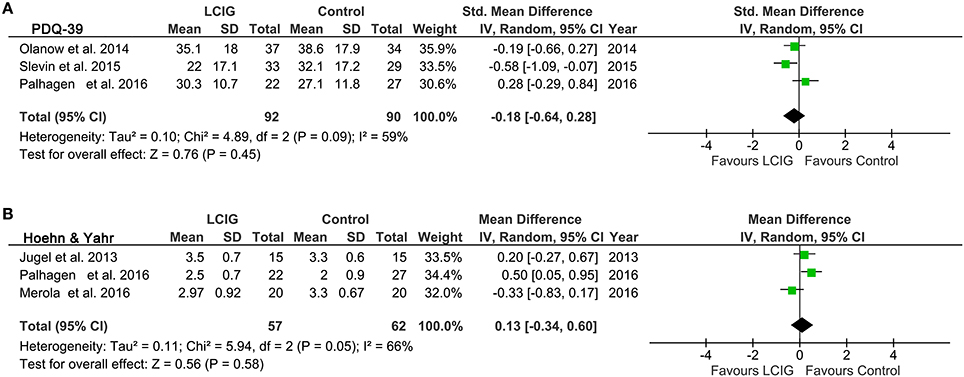
Figure 4. Forest plots of pooled PDQ-39 and Hoehn & Yahr scores in PD patients. Plot A (A), PDQ-39 scores; plot B (B), Hoehn & Yahr scores. PD, Parkinson's disease; LCIG, levodopa-carbidopa intestinal gel; PDQ-39, Unified Parkinson's Disease Rating Scale.
Hoehn & Yahr
Three studies with 119 patients reported the outcome of Hoehn & Yahr. The heterogeneity is significant, as was evident from I2 = 66%, p = 0.05 (Figure 4B). Pooled results using a random-effects model showed that Hoehn & Yahr got an SMD of 0.13 and 95% CI of −0.34 to 0.60, which was also not a significant effect in favor of LCIG (p = 0.58).
Tolerability
Treatment withdrawal (12, 17, 21, 24) were discussed in four studies for any reason. Among them, three trials discussed the treatment withdrawal for adverse effects (AEs) (12, 21, 24). No significant heterogeneity was observed, and thus, a fixed effect model was adopted when analyzed the treatment withdrawal. No significant difference was found between LCIG and control groups in regard to dropouts (OR, 0.54; 95% CI, 0.24 to 1.20; p = 0.13; Figure 5A; OR, 0.83; 95% CI, 0.30 to 2.29; p = 0.71; Figure 5B).
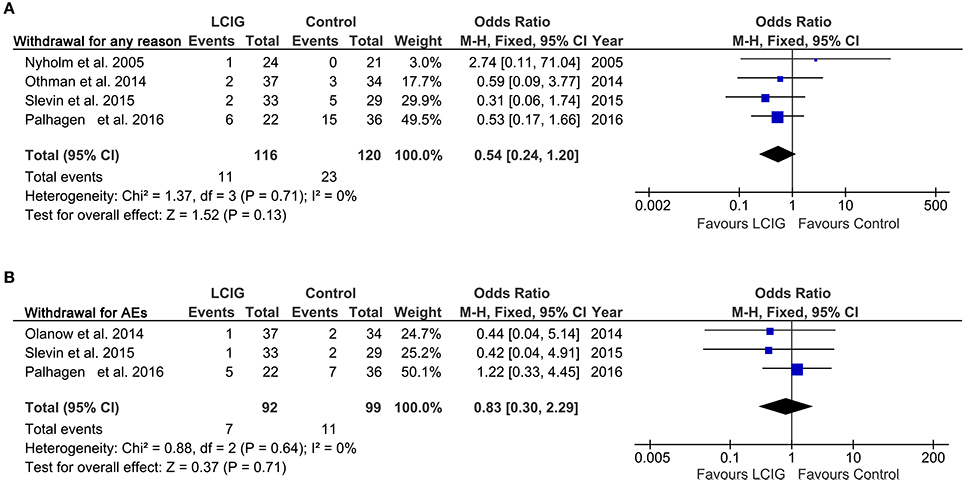
Figure 5. Forest plots of pooled withdrawal in PD patients. Plot A (A), withdrawal for any reason; plot B (B), withdrawal for AEs. PD, Parkinson's disease; AEs, adverse effects; LCIG, levodopa-carbidopa intestinal gel.
Adverse Effects (AEs)
Various AEs were discussed in most included studies. We performed meta-analysis according to the comparison of at least one AE and serious AE. A notable heterogeneity was found in AE (I2 = 52%, p = 0.06), while no notable heterogeneity was found in serious AE (I2 = 0%, p = 0.76). No meaningful differences were found in the risk of AEs (OR, 1.52; 95% CI, 0.34 to 6.74; p = 0.58; Figure 6A) and severe AEs (OR, 0.58; 95% CI, 0.26 to 1.27; p = 0.178; Figure 6B) between control and LCIG. No deaths were reported in the control or LCIG groups of most included studies. However, four deaths occurred in one study (24) (control, n = 2 and LCIG, n = 2). The relationship to study drug was classified by a local study investigator to be unrelated (n = 2), unlikely related (n = 1) to medications and possibly related (n = 1; cardiac arrest) (24).
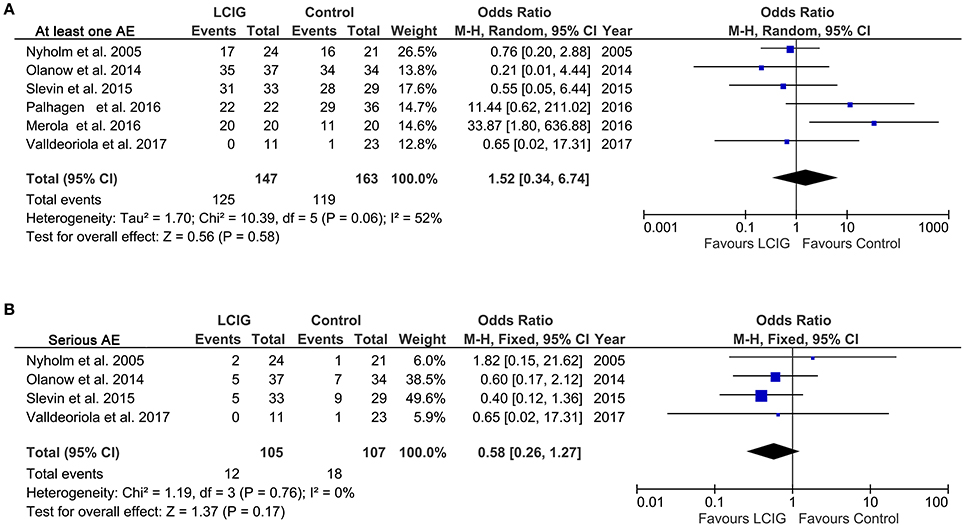
Figure 6. Forest plots of pooled AE in PD patients. Plot A (A), at least one AE; plot B (B), serious AE. PD, Parkinson's disease; LCIG, levodopa-carbidopa intestinal gel; AE, adverse effect.
Publication Bias
Publication bias was estimated by funnel plots. No obvious asymmetry was identified in funnel plots of all outcomes except at least one AE. The funnel plot was quite asymmetrical, suggesting that the publication bias of at least one AE should not be ignored (Figure 7).
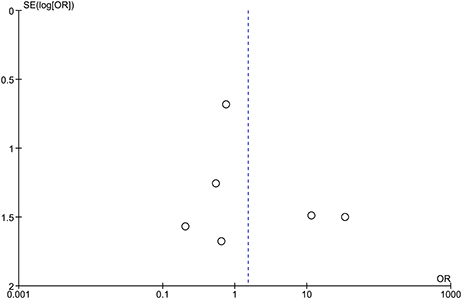
Figure 7. Funnel plot of comparison for at least one AE. The funnel plot appeared asymmetric. Each small circle represents an independent study for the indicated association. AE, adverse effects.
Discussion
The current systematic review and meta-analysis provide evidence that continuous infusion of LCIG provided a clinically significant increase in on-time without troublesome dyskinesia in patients with advanced Parkinson's disease compared with immediate-release oral levodopa. Besides, this benefit was also associated with a significant reduction in off-time. On-time without troublesome dyskinesia in patients treated with LCIG was increased by 0.55 h compared with oral levodopa, and off-time was reduced by 1.19 h. These results were consistent with a recent systematic review (34), which also found that infusion of LCIG reduced off-time, increased on-time without increasing troublesome dyskinesias. There were no differences between groups in UPDRS part II activities of daily life (ADLs) and UPDRS part III motor scores. Similarly, LCIG failed to significantly improve UPDRS, PDQ-39 and Hoehn & Yahr scores. These data suggest that LCIG-treated patients may have approached maximum improvement on several efficacy measures (off-time and on-time without troublesome dyskinesia). The lack of significant further improvement may relate to the notable heterogeneity among these studies and the natural progression of the disease in these patients (24).
This meta-analysis also evaluated the tolerability and safety of LCIG in PD patients. The dropout rates for AEs were 7.6 and 9.1% in LCIG and control group (Figure 5B). Most subjects experienced at least 1 AE (85.0% in LCIG group vs. 73.0% in the control group) (Figure 6A), and most events were mild or moderate in severity. Severe AEs were reported by 11.4% in the LCIG group vs. 16.8% in the control group (Figure 6B). The pooled results showed that there were no clinically meaningful differences in the risk ratio of dropout, AEs and severe AEs between the continuing-LCIG and control patients. Thus, LCIG in Parkinson's disease seems safe and tolerated when compared with control conditions (oral medical treatment or levodopa-carbidopa immediate release). Significantly, Wirdefeldt et al. revealed that the safety issues mainly related to the intestinal infusion system (34). Thus, future studies may further enhance the safety of LCIG by improving the intestinal infusion system.
According to our knowledge, this is the first meta-analysis focusing on the efficacy and safety of LCIG for PD patients. After a comprehensive search, 8 prospective and retrospective studies with 384 PD patients were collected in our meta-analysis. Most included trials were of moderate to high quality. The selection bias was controlled since patients in two groups had a similar baseline condition, and the publication bias was acceptable in most comparisons except AE. However, only two studies used a double-blind design (12, 21), participants bias and rater bias could not be ignored in other studies. Among these included studies, Nyholm et al. also reported the pharmacokinetics changes after intestinal infusion of levodopa, and found that significantly lower variability in plasma levodopa levels can be achieved with the infusion of the stabilized carbidopa/levodopa suspension compared with oral sustained-release tablets (14). Jugel et al. emphasized that handling of LCIG should comprise screening and follow-up exams for polyneuropathy and determine B vitamin as well as folate levels in real time (18).
Cognitive impairment is one of the most important non-motor symptoms in PD, including PD-associated mild cognitive impairment (PD-MCI) and PD-associated dementia (PD-D). Although Valldeoriola et al. and Merola et al. found that LCIG treatment could not significantly improve the Mini-Mental State Examination (MMSE) scores (23, 27), a lot of studies argued that cognitive changes in the LCIG group could be related to a positive effect of L-dopa on some aspects of cognition, including executive function, language function, learning and recall, etc (27, 35, 36).
To ensure the study quality, the present meta-analysis only included trials with a control group. Actually, according to our search results, more studies focusing on LCIG for PD patients were self pre-and post-control observational studies and lack a control group. Most of them confirm the effectiveness and safety profile of LCIG in patients with advanced PD (11, 37–42), especially in the long-term follow-up (43–46). Zibetti and Kruger et al. also found the positive effects of LCIG infusion on sleep quality and quality of life in patients with advanced PD (47, 48). All included studies in this meta-analysis were performed in the USA and Europe, while Murata et al. added that LCIG was also efficacious and tolerable in Japanese, Taiwanese, and Korean advanced PD patients (42). Interestingly, apart from the efficacy and safety, LCIG is also cost-effective for PD patients (49).
Both deep brain stimulation (DBS) and LCIG are invasive therapies. Merola et al. demonstrated that DBS and LCIG showed comparable efficacy in activities of daily living and OFF time for PD patients (23). Besides, Valldeoriola et al. found that compared with patients receiving DBS, PD patients administrated with LCIG might significantly improve some specific neuropsychological functions such as learning, recognition, delayed recall, and visuospatial function (27). However, DBS might yield greater improvement in dyskinesia and lower long-term rate of complications than LCIG (23). Even so, some patients after DBS could also suffer from intolerable side effects, including dysarthria and stimulation-induced freezing of gait (50). For these patients, additional LCIG therapy may be helpful. In general, LCIG should be preferred to DBS for these older patients with more cognitive deficits (50).
There are several strengths in this meta-analysis. First, this systematic review and meta-analysis was designed and reported closely followed the standard PRISMA guidelines, which were comprehensible and concise for other peer researchers in this field. Second, this study is the first comprehensive meta-analysis to date focusing on the efficacy and safety of LCIG in subjects with PD. Another advantage of this study is that we summarized the outcomes as much as possible. The comprehensive reports of comparisons contribute to finding the shortages in these included studies. Moreover, the results of this meta-analysis have some practical implications for the researchers, clinicians and policymakers in this field. For example, future studies may further improve the LCIG system to ensure safety and maximize efficacy. The results also emboldened the clinicians and policymakers, and give them the confidence to conduct LCIG treatment in PD patients.
As with many systematic reviews and meta-analyses, our study has some limitations. First, the significant heterogeneity (I2 ≥ 50% or p ≤ 0.1) should be noted across these eligible original trials. The heterogeneity may be derived from the different study design (cohort studies and RCTs) or duration (from weeks to years), and cannot be ignored in some comparisons. Second, although most included studies had a moderate or high quality. The limited sample size may lead to false negative or positive conclusions. Moreover, patients of the control group in most studies were treated OMT (oral medical treatment) and LC-IR (levodopa-carbidopa immediate release), but Valldeoriola et al. compared LCIG with STN-DBS (subthalamic nucleus deep brain stimulation) in PD patients. Non-placebo control conditions may also underestimate the effects of LCIG.
Conclusions
In conclusion, the present meta-analysis has provided robust evidence that LCIG improves off-time and on-time without troublesome dyskinesia. There were no significant differences in dropout ratio and AEs between LCIG and control groups, which suggested LCIG was relatively tolerated and safe. Therefore, LCIG may be a promising option for advanced PD patients with motor complications. More double-blind RCTs are needed in this field and future studies should pay more attention to unify its dosage and treatment duration.
Author Contributions
LW contributed to study design, data extraction, quality assessment, analysis and interpretation of data, and drafting the manuscript. JL contributed to data extraction, quality assessment, analysis and interpretation of data, and drafting the manuscript. JC conceiving the study, participating in study design and revising the article. All authors proofed and approved the submitted version of the article.
Funding
This study was supported by parkinson-related lncRNA differential expression analysis and Jilin Province Neurological Diseases Precision Medicine Science and Technology Innovation Center (No. 20170623006TC).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. de Lau LM, Breteler MM. Epidemiology of Parkinson's disease. Lancet Neurol. (2006) 5:525–35. doi: 10.1016/s1474-4422(06)70471-9
2. Lattanzi S, Grillo E, Brigo F, Silvestrini M. Efficacy and safety of perampanel in Parkinson's disease. A systematic review with meta-analysis. J Neurol. (2018) 265:733–40. doi: 10.1007/s00415-017-8681-y
3. Zhang ZX, Roman GC, Hong Z, Wu CB, Qu QM, Huang JB, et al. Parkinson's disease in China: prevalence in Beijing, Xian, and Shanghai. Lancet (2005) 365:595–7. doi: 10.1016/s0140-6736(05)17909-4
4. Olanow C W., Watts R. L., Koller W. C. (2001). An algorithm (decision tree) for the management of Parkinson's disease: treatment guidelines. Neurology (2001) 56(11 Suppl. 5):S1–88.
5. Lundqvist C. Continuous levodopa for advanced Parkinson's disease. Neuropsychiatr Dis Treat. (2007) 3:335–48.
6. Montane E, Vallano A, Vidal X, Aguilera C, Laporte JR. Reporting randomised clinical trials of analgesics after traumatic or orthopaedic surgery is inadequate: a systematic review. BMC Clin Pharmacol. (2010) 10:2. doi: 10.1186/1472-6904-10-2
7. Shoulson I, Glaubiger GA, Chase TN. On-off response. Clinical and biochemical correlations during oral and intravenous levodopa administration in parkinsonian patients Neurology (1975) 25:1144–8.
8. Olanow CW, Obeso JA, Stocchi F. Drug insight: continuous dopaminergic stimulation in the treatment of Parkinson's disease. Nat Clin Pract Neurol. (2006) 2:382–92. doi: 10.1038/ncpneuro0222
9. Nyholm D, Askmark H, Gomes-Trolin C, Knutson T, Lennernas H, Nystrom C, et al. Optimizing levodopa pharmacokinetics: intestinal infusion versus oral sustained-release tablets. Clin Neuropharmacol. (2003) 26:156–63.
10. Olanow CW, Obeso JA, Stocchi F. Continuous dopamine-receptor treatment of Parkinson's disease: scientific rationale and clinical implications. Lancet Neurol. (2006) 5:677–87. doi: 10.1016/s1474-4422(06)70521-x
11. Fernandez HH, Vanagunas A, Odin P, Espay AJ, Hauser RA, Standaert DG, et al. Levodopa-carbidopa intestinal gel in advanced Parkinson's disease open-label study: interim results. Parkinsonism Relat Disord. (2013) 19:339–45. doi: 10.1016/j.parkreldis.2012.11.020
12. Olanow CW, Kieburtz K, Odin P, Espay AJ, Standaert DG, Fernandez HH, et al. Continuous intrajejunal infusion of levodopa-carbidopa intestinal gel for patients with advanced Parkinson's disease: a randomised, controlled, double-blind, double-dummy study. Lancet Neurol. (2014) 13:141–9. doi: 10.1016/s1474-4422(13)70293-x
13. Loens S, Chorbadzhieva E, Kleimann A, Dressler D, Schrader C. Effects of levodopa/carbidopa intestinal gel versus oral levodopa/carbidopa on B vitamin levels and neuropathy. Brain Behav. (2017) 7:e00698. doi: 10.1002/brb3.698
14. Nyholm D, Askmark H, Gomes-Trolin C, Knutson T, Lennernäs H, Nyström C, et al. Optimizing levodopa pharmacokinetics: Intestinal infusion vs. oral sustained-release tablets. Clin Neuropharmacol.(2003) 26:156–63. doi: 10.1097/00002826-200305000-00010
15. Westin J, Nyholm D, Palhagen S, Willows T, Groth T, Dougherty M, et al. A pharmacokinetic-pharmacodynamic model for duodenal levodopa infusion. Clin Neuropharmacol. (2011) 34:61–5. doi: 10.1097/WNF.0b013e31820b570a
16. Nyholm D, Odin P, Johansson A, Chatamra K, Locke C, Dutta S, et al. Pharmacokinetics of levodopa, carbidopa, and 3-O-methyldopa following 16-hour jejunal infusion of levodopa-carbidopa intestinal gel in advanced Parkinson's disease patients. AAPS J. (2013) 15:316–23. doi: 10.1208/s12248-012-9439-1
17. Nyholm D, Nilsson Remahl AI, Dizdar N, Constantinescu R, Holmberg B, Jansson R, et al. Duodenal levodopa infusion monotherapy vs oral polypharmacy in advanced Parkinson disease. Neurology (2005) 64:216–23. doi: 10.1212/01.wnl.0000149637.70961.4c
18. Jugel C, Ehlen F, Taskin B, Marzinzik F, Müller T, Klostermann F. Neuropathy in parkinson's disease patients with intestinal levodopa infusion vs. oral drugs. PLoS ONE (2013) 8:e66639. doi: 10.1371/journal.pone.0066639
19. Othman AA, Dutta S. Population pharmacokinetics of levodopa in subjects with advanced Parkinson's disease: levodopa-carbidopa intestinal gel infusion vs. oral tablets. Br J Clin Pharmacol. (2014) 78:94–105. doi: 10.1111/bcp.12324
20. Othman AA, Chatamra K, Mohamed ME, Dutta S, Benesh J, Yanagawa M, et al. Jejunal Infusion of levodopa-carbidopa intestinal gel versus oral administration of levodopa-carbidopa tablets in japanese subjects with advanced Parkinson's disease: pharmacokinetics and pilot efficacy and safety. Clin Pharmacokinet. (2015) 54:975–84. doi: 10.1007/s40262-015-0265-3
21. Slevin JT, Fernandez HH, Zadikoff C, Hall C, Eaton S, Dubow J, et al. Long-term safety and maintenance of efficacy of levodopa-carbidopa intestinal gel: an open-label extension of the double-blind pivotal study in advanced Parkinson's disease patients. J Parkinsons Dis. (2015) 5:165–74. doi: 10.3233/jpd-140456
22. Antonini A, Fung VS, Boyd JT, Slevin JT, Hall C, Chatamra K, et al. Effect of levodopa-carbidopa intestinal gel on dyskinesia in advanced Parkinson's disease patients. Mov Disord. (2016) 31:530–7. doi: 10.1002/mds.26528
23. Merola A, Espay AJ, Romagnolo A, Bernardini A, Rizzi L, Rosso M, et al. Advanced therapies in Parkinson's disease: long-term retrospective study. Parkinsonism Relat Disord. (2016) 29:104–8. doi: 10.1016/j.parkreldis.2016.05.015
24. Palhagen SE, Sydow O, Johansson A, Nyholm D, Holmberg B, Widner H, et al. Levodopa-carbidopa intestinal gel (LCIG) treatment in routine care of patients with advanced Parkinson's disease: an open-label prospective observational study of effectiveness tolerability and healthcare costs. Parkinsonism Relat Disord. (2016) 29:17–23. doi: 10.1016/j.parkreldis.2016.06.002
25. Othman AA, Rosebraugh M, Chatamra K, Locke C, Dutta S. Levodopa-carbidopa intestinal gel pharmacokinetics: lower variability than oral levodopa-carbidopa. J Parkinsons Dis. (2017) 7:275–8. doi: 10.3233/jpd-161042
26. Senek M, Nielsen EI, Nyholm D. Levodopa-entacapone-carbidopa intestinal gel in Parkinson's disease: a randomized crossover study. Mov Disord. (2017) 32:283–6. doi: 10.1002/mds.26855
27. Valldeoriola F, Santacruz P, Rios J, Compta Y, Rumia J, Munoz JE, et al. l-Dopa/carbidopa intestinal gel and subthalamic nucleus stimulation: effects on cognition and behavior. Brain Behav. (2017) 7:e00848. doi: 10.1002/brb3.848
28. Furlan AD, Pennick V, Bombardier C, van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (2009) 34:1929–41. doi: 10.1097/BRS.0b013e3181b1c99f
29. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
30. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
31. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
32. Peng Z, Sun Y, Lv X, Zhang H, Liu C, Dai S. Interleukin-6 levels in women with polycystic ovary syndrome: a systematic review and meta-analysis. PLoS ONE (2016) 11:e0148531. doi: 10.1371/journal.pone.0148531
33. Dayan N, Filion KB, Okano M, Kilmartin C, Reinblatt S, Landry T, et al. Cardiovascular risk following fertility therapy: systematic review and meta-analysis. J Am Coll Cardiol. (2017) 70:1203–13. doi: 10.1016/j.jacc.2017.07.753
34. Wirdefeldt K, Odin P, Nyholm D. Levodopa-carbidopa intestinal gel in patients with parkinson's disease: a systematic review. CNS Drugs (2016) 30:381–404. doi: 10.1007/s40263-016-0336-5
35. Muslimovic D, Post B, Speelman JD, Schmand B. Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology (2005) 65:1239–45. doi: 10.1212/01.wnl.0000180516.69442.95
36. Fera F, Nicoletti G, Cerasa A, Romeo N, Gallo O, Gioia MC, et al. Dopaminergic modulation of cognitive interference after pharmacological washout in Parkinson's disease. Brain Res Bull. (2007) 74:75–83. doi: 10.1016/j.brainresbull.2007.05.009
37. Fernandez HH, Standaert DG, Hauser RA, Lang AE, Fung VS, Klostermann F, et al. Levodopa-carbidopa intestinal gel in advanced Parkinson's disease: final 12-month, open-label results. Mov Disord. (2015) 30:500–9. doi: 10.1002/mds.26123
38. Bajenaru O, Ene A, Popescu BO, Szasz JA, Sabau M, Muresan DF, et al. The effect of levodopa-carbidopa intestinal gel infusion long-term therapy on motor complications in advanced Parkinson's disease: a multicenter Romanian experience. J Neural Transm. (2016) 123:407–14. doi: 10.1007/s00702-015-1496-z
39. Bologna M, Latorre A, Di Biasio F, Conte A, Belvisi D, Modugno N, et al. The effect of L-dopa/carbidopa intestinal gel in parkinson disease assessed using neurophysiologic techniques. Clin Neuropharmacol. (2016) 39:302–5. doi: 10.1097/wnf.0000000000000184
40. Lopiano L, Modugno N, Marano P, Sensi M, Meco G, Cannas A, et al. Motor outcomes in patients with advanced Parkinson's disease treated with levodopa/carbidopa intestinal gel in Italy: an interim analysis from the GREENFIELD observational study. Neurol Sci. (2016) 37:1785–92. doi: 10.1007/s10072-016-2664-0
41. Standaert DG, Rodriguez RL, Slevin JT, Lobatz M, Eaton S, Chatamra K, et al. Effect of levodopa-carbidopa intestinal gel on non-motor symptoms in patients with advanced parkinson's disease. Mov Disord Clin Pract. (2017) 4:829–37. doi: 10.1002/mdc3.12526
42. Murata M, Mihara M, Hasegawa K, Jeon B, Tsai CH, Nishikawa N, et al. Safety and efficacy of levodopa-carbidopa intestinal gel: results from an open-label extension study in Japanese, Korean and Taiwanese patients with advanced Parkinson's disease. Ther Adv Neurol Disord. (2018) 11:1756286418759315. doi: 10.1177/1756286418759315
43. Caceres-Redondo MT, Carrillo F, Lama MJ, Huertas-Fernandez I, Vargas-Gonzalez L, Carballo M, et al. Long-term levodopa/carbidopa intestinal gel in advanced Parkinson's disease. J Neurol. (2014) 261:561–9. doi: 10.1007/s00415-013-7235-1
44. Valldeoriola F, Grandas F, Santos-Garcia D, Regidor I, Catalan MJ, Arbelo JM, et al. Long-term effectiveness of levodopa-carbidopa intestinal gel in 177 Spanish patients with advanced Parkinson's disease. Neurodegener Dis Manage. (2016) 6:289–98. doi: 10.2217/nmt-2016-0021
45. De Fabregues O, Dot J, Abu-Suboh M, Hernandez-Vara J, Ferre A, Romero O, et al. Long-term safety and effectiveness of levodopa-carbidopa intestinal gel infusion. Brain Behav. (2017) 7:e00758. doi: 10.1002/brb3.758
46. Fernandez HH, Boyd JT, Fung VSC, Lew MF, Rodriguez RL, Slevin JT, et al. Long-term safety and efficacy of levodopa-carbidopa intestinal gel in advanced Parkinson's disease. Mov Disord. (2018). doi: 10.1002/mds.27338
47. Zibetti M, Rizzone M, Merola A, Angrisano S, Rizzi L, Montanaro E, et al. Sleep improvement with levodopa/carbidopa intestinal gel infusion in Parkinson disease. Acta Neurol Scand. (2013) 127:e28–32. doi: 10.1111/ane.12075
48. Kruger R, Lingor P, Doskas T, Henselmans JML, Danielsen EH, de Fabregues O, et al. An Observational study of the effect of levodopa-carbidopa intestinal gel on activities of daily living and quality of life in advanced parkinson's disease patients. Adv Ther. (2017) 34:1741–52. doi: 10.1007/s12325-017-0571-2
49. Kamusheva MS, Gerasimov N, Petrova GI. Intestinal gel Levodopa + Carbidopa in Parkinson's patients with frequent and prolonged akinesia - an economic evaluation. Int J Pharm Sci Rev Res. (2013) 22:244–6. Available online at: http://globalresearchonline.net/journalcontents/v22-1/44.pdf
Keywords: Parkinson's disease, levodopa-carbidopa intestinal gel, efficacy, safety, meta-analysis
Citation: Wang L, Li J and Chen J (2018) Levodopa-Carbidopa Intestinal Gel in Parkinson's Disease: A Systematic Review and Meta-Analysis. Front. Neurol. 9:620. doi: 10.3389/fneur.2018.00620
Received: 16 May 2018; Accepted: 10 July 2018;
Published: 30 July 2018.
Edited by:
Giuseppe De Michele, Università degli Studi di Napoli Federico II, ItalyReviewed by:
Matteo Bologna, Sapienza Università di Roma, ItalyPedro Ribeiro, Universidade Federal do Rio de Janeiro, Brazil
Copyright © 2018 Wang, Li and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiajun Chen, ampjaGVuX25ldXJvbG9neUAxMjYuY29t
 Libo Wang
Libo Wang Jia Li
Jia Li Jiajun Chen
Jiajun Chen