
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Microbiol. , 12 October 2018
Sec. Fungi and Their Interactions
Volume 9 - 2018 | https://doi.org/10.3389/fmicb.2018.02434
This article is part of the Research Topic Diagnostic Approaches for Aspergillus Infections View all 20 articles
 Afsane Vaezi1
Afsane Vaezi1 Hamed Fakhim2,3
Hamed Fakhim2,3 Zahra Abtahian4
Zahra Abtahian4 Sadegh Khodavaisy5
Sadegh Khodavaisy5 Mohsen Geramishoar5
Mohsen Geramishoar5 Ahad Alizadeh6
Ahad Alizadeh6 Jacques F. Meis7,8
Jacques F. Meis7,8 Hamid Badali1,9*
Hamid Badali1,9*Autosomal recessive deficiency in the caspase recruitment domain containing protein 9 (CARD9) results in susceptibility to fungal infections. In the last decade, infections associated with CARD9 deficiency are more reported due to the advent of genome sequencing. The aim of this study was to evaluate the frequency, geographic distribution and nature of mutations in patients with CARD9 deficiency. We identified 60 patients with 24 mutations and different fungal infections. The presence of the homozygous (HMZ) p.Q295X (c.883C > T) and HMZ p.Q289X (c.865C > T) mutations were associated with an elevated risk of candidiasis (OR: 1.6; 95% CI: 1.18–2.15; p = 0.004) and dermatophytosis (OR: 1.85; 95% CI: 1.47–2.37; p < 0.001), respectively. The geographical distribution differed, showing that the main mutations in African patients were different Asian patients; HMZ p.Q289X (c.865C > T) and HMZ p.Q295X (c.865C > T) accounted for 75% and 37.9% of the African and Asian cases, respectively. The spectrum of CARD9 mutations in Asian patients was higher than in African. Asia is the most populous continent in the world and may have a greater genetic burden resulting in more patients with severe fungal infections. The presence of a high diversity of mutations revealing 24 distinct variations among 60 patients emphasize that the unique genetic alteration in CARD9 gene may be associated with certain geographical areas.
Susceptibility to fungal infections in otherwise healthy individuals with Mendelian disorders are increasingly being recognized (Vinh, 2011) than before the widespread use of genome sequencing. Primary immunodeficiencies consist of various genetic defects that affect the innate and adaptive immune systems. In addition, evaluation of previously healthy, fungus infected patients, suspected of having a primary genetic immunodeficiency may give valuable insights on the role of specific proteins in the immune system for protection from these infections (Wang et al., 2014; Corvilain et al., 2018). Caspase recruitment domain containing protein 9 (CARD9) is a central regulator of innate immunity that is highly expressed in neutrophils, macrophages, dendritic cells, and during cell apoptosis in low-serum conditions (Bertin et al., 2000; Liang et al., 2015). Mutations in several proteins involved in the CARD9 signaling protein have been demonstrated to cause primary immunodeficiencies in humans. These mutations cause a decreased production of cytokines from innate immune cells, leading to deficiencies of TH17 and accordingly predispose patients to severe disseminated infections (Conti and Gaffen, 2015). Severe fungal infections in healthy patients have recently been reported from a few countries, i.e., Algeria, Brazil, France, China, Iran, Morocco and Tunisia (Glocker et al., 2009; Drewniak et al., 2013; Lanternier et al., 2013; Wang et al., 2014; Grumach et al., 2015) and linked to autosomal recessive CARD9 deficiency. The species involved in these infections are Trichophyton violaceum, Trichophyton rubrum, Candida species, Exophiala species, Phialophora verrucosa, Aspergillus fumigatus, Prototheca zopfii, and Mucor irregularis. Some of those etiological agents are plant pathogens, which rarely have been associated with human infection. Highly diverse clinical manifestations from cutaneous to disseminated and progressive infections are observed (Boudghène-Stambouli and Mérad-Boudia, 1991; Boudghène-Stambouli et al., 1992; Pruszkowski et al., 1995). Our aim was to evaluate the global frequency, geographic distribution and nature of mutations in patients with CARD9 deficiency associated with fungal infections.
The review process involved study of existing published literature of all reported cases with fungal infection due to CARD9 deficiency. To search the published literature, Medline database through PubMed, Embase through Scopus, ISI Web of Science, Science Direct and Google Scholar were used to explore the published literature of patients with severe fungal infection and CARD9 deficiency using the key words “caspase recruitment domain deficiency,” “CARD9 deficiency,” “autosomal recessive CARD9 deficiency,” “primary immunodeficiency,” “mutations,” “fungal infection” or “invasive fungal diseases,” “candidiasis,” “deep dermatophytosis,” “disseminated phaeohyphomycosis,” and “chronic mucocutaneous candidiasis” in different combinations. A total of 21 relevant articles were found using these key words. The extracted data were analyzed using R software version 3.4.1. The chi-square test was utilized to evaluate associations between nominal variables and the p-value was estimated using the Monte Carlo method. To compare the differential prevalence of CARD9 mutations and determine differences in causative agents of fungal infections, odds ratios (ORs) were used. The significance of all ORs, using a 95% Bayesian credible interval (CI), was calculated using Bayesian logistic regression.
To analyze the role of CARD9 deficiency in fungal infection, we reviewed the literature and identified 60 cases until 2018. The total number of patients with severe fungal infection related to CARD9 deficiency has been summarized in Tables 1A,B (Boudghène-Stambouli and Mérad-Boudia, 1989, 1991, 1998; Pruszkowski et al., 1995; Glocker et al., 2009; Drewniak et al., 2013; Gavino et al., 2014; Wang et al., 2014; Drummond et al., 2015; Grumach et al., 2015; Herbst et al., 2015; Jachiet et al., 2015; Lanternier et al., 2015a,b; Alves de Medeiros et al., 2016; Gavino et al., 2016; Jones et al., 2016; Rieber et al., 2016; Yan et al., 2016; Boudghene-Stambouli et al., 2017; Gavino et al., 2018; Sari et al., 2018; Vaezi et al., 2018; Wang et al., 2018a,b). The age at the time of diagnosis ranged from 4 to 91 years (mean 34.3 ± 17.9 years). Since 1989, a total of 14 countries reported cases of fungal infections associated with CARD9 deficiency (Figure 1). Although most cases originate from Algeria (North Africa) [n = 12 (21.1%)], the majority of cases were from several countries in the Asian continent (n = 29, 48.3%), with Iran reporting the majority (n = 10/29, 34.5%). The main fungal infection associated with CARD9 deficiency was candidiasis (40.3%) followed by deep dermatophytosis (37.3%), phaeohyphomycosis (16.4%) and invasive aspergillosis (3.0%). T. violaceum, T. rubrum, and Trichophyton mentagrophytes were observed as etiological agents of dermatophytosis. Candida infections were caused by C. albicans and non-albicans Candida species in 70.8% and 29.2% of the cases, respectively. P. verrucosa (36.4%) represented the major species of phaeohyphomycosis and were only reported from China. Neurological infection (40.5%) was the predominant clinical presentation in Candida infected patients followed by chronic mucosal and cutaneous candidiasis (29.7%). The outcome was recorded in 45 cases and 11 (24.4%) expired.
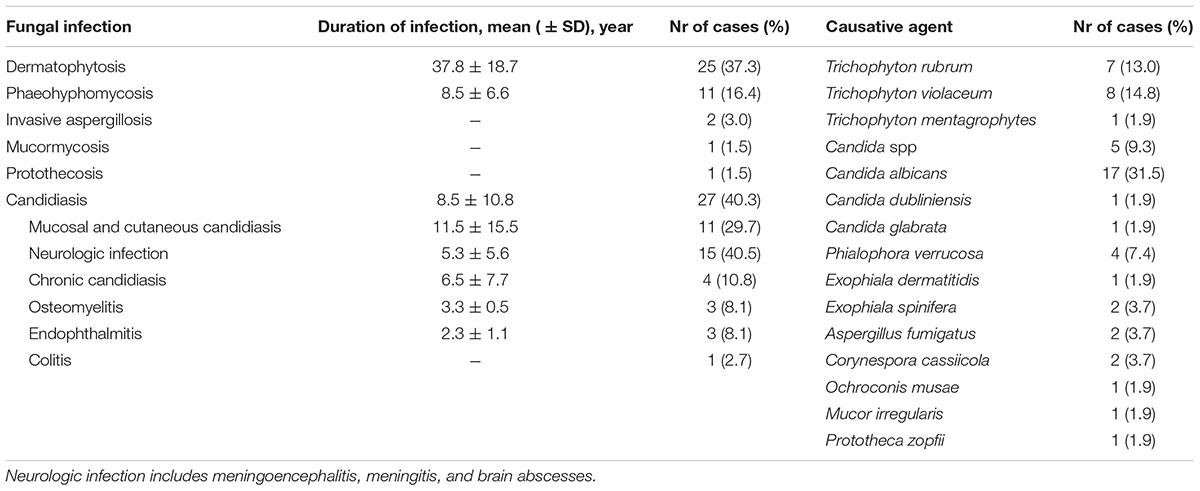
TABLE 1A. Prevalence of fungal infections, duration of infections and causative pathogens in patients with CARD9 deficiency.
Overall, 24 different genetic alterations in CARD9 were described in the 60 patients. Three of those were identified most frequently: homozygous (HMZ) p.Q289X (c.865C > T), HMZ p.Q295X (c.883C > T) and HMZ p.D274fsX60 (c.819-820insG), which accounted for 25.8%, 17.7%, and 8.1% of the patients, respectively. Multiple variations in CARD9 were identified in 8.7% of all cases. The correlation between mutations and fungal infection is shown in Figure 2. The presence of the HMZ p.Q295X (c.883C > T) and HMZ p.Q289X (c.865C > T) mutation was associated with an elevated risk of candidiasis (OR: 1.6; 95% CI: 1.18–2.15; p = 0.004) and dermatophytosis (OR: 1.85; 95% CI: 1.47–2.37; p < 0.001), respectively. Also a strong association was evident between the presence of HMZ p.D274fsX60 (c.819-820insG) and disseminated phaeohyphomycosis; 2.42 (95% CI 1.84–3.2, p < 0.001). This study demonstrated that the HMZ p.Q289X (c.865C > T) mutation had a more than two-fold increased risk of dermatophytosis compared with HMZ p.Q295X (c.883C > T), p < 0.001. Similarly, HMZ p.Q295X (c.883C > T) alteration increased by two times the risk of developing candidiasis [OR: 1.95 (95% CI 1.42-2.69, p < 0⋅001)] versus dermatophytosis (Table 2). T. violaceum infected patients carried a marginally higher frequency of HMZ p.Q289X (c.865C > T) compared to non-T. violaceum dermatophytosis cases (43 vs. 56%).
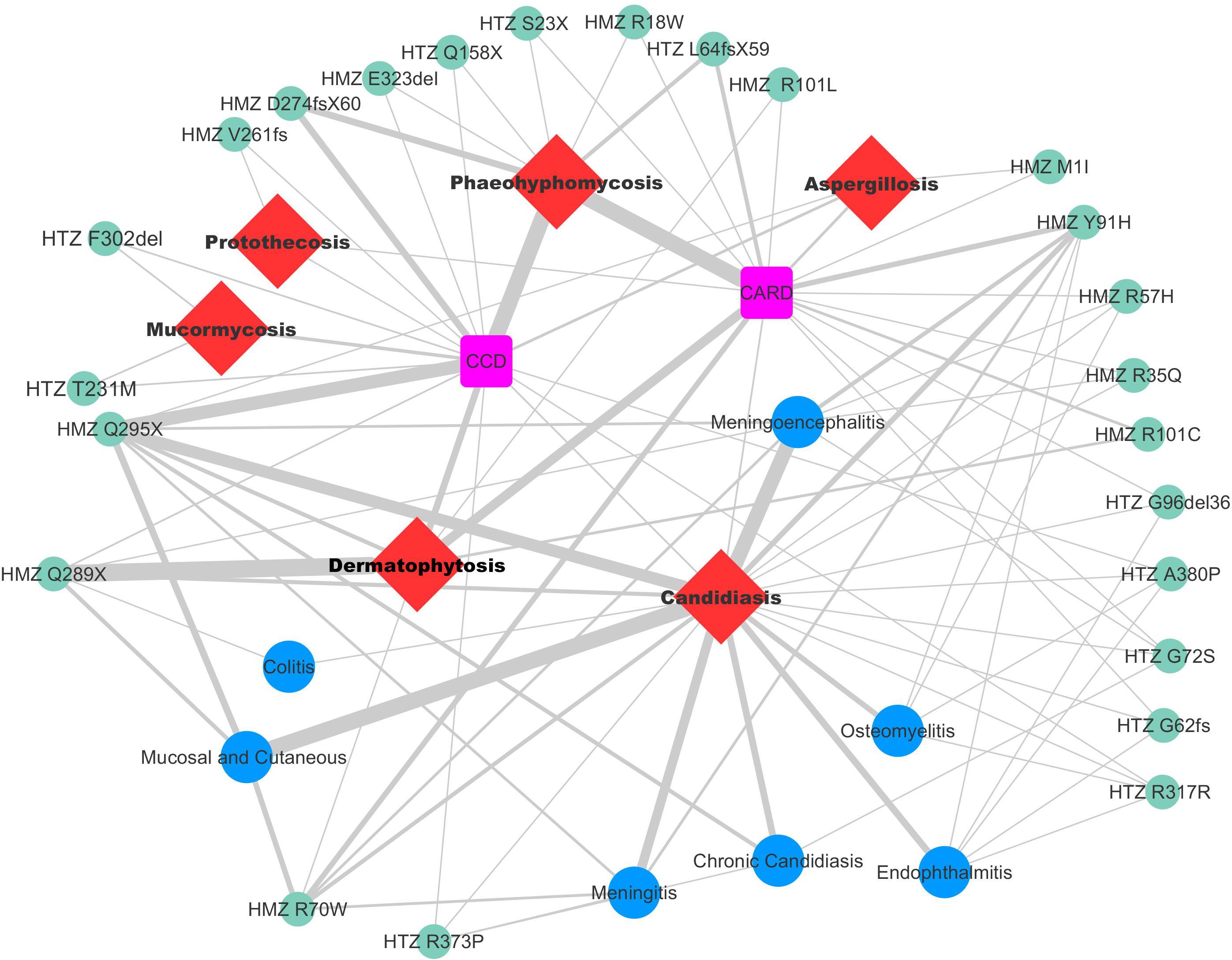
FIGURE 2. Relation between the types of mutations and different clinical forms. Thick, short, and bold line indicates more reported cases with a mutation and clinical form; and less cases shown with thin and lane lines.
The pattern of distribution was differed by geographical region in reported cases with CARD9 mutations. The main mutations in African patients were different from those in Asians; HMZ p.Q289X (c.865C > T) and HMZ p.R101C (c.C301T), accounting for 75% and 10%, respectively, were the common mutations in Africa. The three most common mutations in Asia were HMZ p.Q295X (c.883C > T), HMZ p.D274fsX60 (c.819-820insG), and HMZ p.R70W (c.208C > T), which accounted for 34.5%, 17.2%, and 13.8% of the Asian cases, respectively. Notably, HMZ p.Q289X (c.865C > T) was the most common mutation observed in 75% of the Algerian patients (9 out of 12), while the HMZ p.Q295X (c.883C > T) mutation was reported in 8 out of 10 Iranian patients (80%). This finding is important as it provides a relationship between mutation and specific geographic occurrence in these patients.
CARD9 deficiency is inherited in an autosomal recessive manner. CARD9 plays an important role in the activation of antifungal mechanisms leading to expression of gene products that initiate the inflammatory cascade (Liang et al., 2015; Drummond and Lionakis, 2016). The importance of the CARD9 signaling protein in host defense has been demonstrated in a murine CARD9-/- model with targeted disruptions of innate signaling from the antifungal pattern-recognition receptor, dectin-1, that identifies the β-glucan component of the fungal cell (Taylor et al., 2007). Defective antifungal clearance and latently infected cells could be the result of impaired CARD9 function (Yamamoto et al., 2014; Drummond and Lionakis, 2016). We analyzed the characteristics, distribution, frequency, and relationship between the genotype of the CARD9 gene mutations and fungal infections among the reported cases. Since the first mutation described in 1989 from Algeria (Boudghène-Stambouli and Mérad-Boudia, 1989), several mutations have been reported from Africa. However, only few reports are from Europe and America. Glocker et al. (2009), reported a novel CARD9 mutation, HMZ p.Q289X (c.883C > T), in seven Iranian patients. In this review, the spectrum of CARD9 mutations in Asian patients is higher than in African patients. So far, more than 24 mutations in the CARD9 gene have been reported associated with severe fungal infections. Among these mutations, HMZ p.Q289X (c.865C > T) was the most common, indicating it is a hot spot in Africa. Infections caused by T. violaceum and C. albicans dominate, but frequency differ by region. We found a remarkably low prevalence of dermatophyte infection in Asian CARD9 deficiency patients. However, we demonstrate that Candida species infection is also uncommon in African patients. Our review showed that the two mutations [HMZ p.Q289X (c.865C > T) and HMZ p.Q295X (c.883C > T)] are present in 44.3% of the patients. Dermatophytosis due to the HMZ p.Q289X (c.865C > T) mutation encompass 75% of African cases and 34.5% of Asian patients have candidiasis associated with HMZ p.Q295X (c.883C > T). However, mutations such as HMZ p.R57H (c.170G > A), heterozygous (HTZ) p.A380P (c.1138G > C) and HMZ p.R70W (c.208C > T) are only found in the United States, United Kingdom, and Turkey, respectively, which suggests that mutations may be specific in particular populations or geographic regions. Another possible explanation is the high rate of consanguinity in many closed groups. Although this autosomal recessive disorder which is rare on a world-wide scale, it may not be rare in some countries. The variations in the gene, which are associated with a specific fungal infection, remain unknown. Asia is the most populous continent in the world and may have a greater genetic burden resulting in more patients with severe fungal infections. Although we cannot exclude other causative factors, our data support the notion that some CARD9 mutations, circulating in specific geographic regions, could be the contributing factor for fungal infections. However, because of the small sample size, future screening should be conducted to confirm these conclusions. Studying the impact of genetic variation on severe fungal infection will improve our understanding of pathogenesis and may ultimately aid future interventions. CARD9 deficiency should be considered in patients with unexplained progressive fungal infection, as it may allow early initiation of appropriate antifungal treatment. Regular medical follow-up and identification of patients with CARD9 deficiencies is recommended including family members.
In recent years, interest in primary immunodeficiency disorders and opportunistic infections has grown. The current study reviewed 60 reported cases with CARD9 mutations and severe fungal infections, which may provide more information about the relationship between these mutations, the specific geographic presence and the unique predisposition to a particular fungal disease.
AV, HB, and JM conceptualized the study, gathered resources, and wrote, reviewed, and edited the manuscript. AV, HF, ZA, MG, SK, and AA curated the data. AV, HB, and AA performed the formal analysis of the study. HB contributed to funding acquisition, project administration, and data validation. AV and HF investigated the data. AV, HF, ZA, MG, and SK provided methodology for this study. HB and JM supervised the study. AV, HF, ZA, MG, SK, AA, JM, and HB wrote the original draft of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Alves de Medeiros, A. K., Lodewick, E., Bogaert, D. J., Haerynck, F., Van Daele, S., Lambrecht, B., et al. (2016). Chronic and invasive fungal infections in a family with CARD9 deficiency. J. Clin. Immunol. 36, 204–209. doi: 10.1007/s10875-016-0255-8
Bertin, J., Guo, Y., Wang, L., Srinivasula, S. M., Jacobson, M. D., Poyet, J. L., et al. (2000). CARD9 is a novel caspase recruitment domain-containing protein that interacts with BCL10/CLAP and activates N-F-kappa B. J. Biol. Chem. 275, 41082–41086. doi: 10.1074/jbc.C000726200
Boudghene-Stambouli, O., Amrani, N., Boudghéne Stambouli, K., and Bouali, F. (2017). Dermatophytic disease with deficit in CARD9: a new case with a brain impairment. J. Mycol. Med. 27, 250–253. doi: 10.1016/j.mycmed.2017.01.001
Boudghène-Stambouli, O., and Mérad-Boudia, A. (1989). Trichophyton rubrum dermatophytic disease: a new case. Ann. Dermatol. Venereol. 116, 725–727.
Boudghène-Stambouli, O., and Mérad-Boudia, A. (1991). Dermatophytic disease in Algeria: a new case and review of the literature. Ann. Dermatol. Venereol. 118, 17–21.
Boudghène-Stambouli, O., and Mérad-Boudia, A. (1998). Dermatophytic disease: exuberant hyperkeratosis with cutaneous horns. Ann. Dermatol. Venereol. 125, 705–707.
Boudghène-Stambouli, O., Mérad-Boudia, A., and Allal, M. (1992). Cerebral injury in dermatophytic disease. J. Mycol. Med. 2, 106–108.
Conti, H. R., and Gaffen, S. L. (2015). IL-17-mediated immunity to the opportunistic fungal pathogen Candida albicans. J. Immunol. 195, 780–788. doi: 10.4049/jimmunol.1500909
Corvilain, E., Casanova, J. L., and Puel, A. (2018). Inherited CARD9 deficiency: invasive disease caused by Ascomycete fungi in previously healthy children and adults. J. Clin. Immunol. 38, 656–693. doi: 10.1007/s10875-018-0539-2
Drewniak, A., Gazendam, R. P., Tool, A. T., van Houdt, M., Jansen, M. H., van Hamme, J. L., et al. (2013). Invasive fungal infection and impaired neutrophil killing in human CARD9 deficiency. Blood 121, 2385–2392. doi: 10.1182/blood-2012-08-450551
Drummond, R. A., Collar, A. L., Swamydas, M., Rodriguez, C. A., Lim, J. K., Mendez, L. M., et al. (2015). CARD9-dependent neutrophil recruitment protects against fungal invasion of the central nervous system. PLoS Pathog. 11:e1005293. doi: 10.1371/journal.ppat.1005293
Drummond, R. A., and Lionakis, M. S. (2016). Mechanistic insights into the role of C-type lectin receptor/CARD9 signaling in human antifungal immunity. Front. Cell. Infect. Microbiol. 6:39. doi: 10.3389/fcimb.2016.00039
Gavino, C., Cotter, A., Lichtenstein, D., Lejtenyi, D., Fortin, C., Legault, C., et al. (2014). CARD9 deficiency and spontaneous central nervous system candidiasis: complete clinical remission with GM-CSF therapy. Clin. Infect. Dis. 59, 81–84. doi: 10.1093/cid/ciu215
Gavino, C., Hamel, N., Zeng, J. B., Legault, C., Guiot, M. C., Chankowsky, J., et al. (2016). Impaired RASGRF1/ERK-mediated GM-CSF response characterizes CARD9 deficiency in French-Canadians. J. Allergy Clin. Immunol. 137, 1178.e7–1188.e7. doi: 10.1016/j.jaci.2015.09.016
Gavino, C., Mellinghoff, S., Cornely, O. A., Landekic, M., Le, C., Langelier, M., et al. (2018). Novel bi-allelic splice mutations in CARD9 causing adult-onset Candida endophthalmitis. Mycoses 61, 61–65. doi: 10.1111/myc.12701
Glocker, E. O., Hennigs, A., Nabavi, M., Schaffer, A. A., Woellner, C., Salzer, U., et al. (2009). A homozygous CARD9 mutation in a family with susceptibility to fungal infections. N. Engl. J. Med. 361, 1727–1735. doi: 10.1056/NEJMoa0810719
Grumach, A. S., de Queiroz-Telles, F., Migaud, M., Lanternier, F., Filho, N. R., Palma, S. M., et al. (2015). A homozygous CARD9 mutation in a Brazilian patient with deep dermatophytosis. J. Clin. Immunol. 35, 486–490. doi: 10.1007/s10875-015-0170-4
Herbst, M., Gazendam, R., Reimnitz, D., Sawalle-Belohradsky, J., Groll, A., Schlegel, P. G., et al. (2015). Chronic Candida albicans meningitis in a 4-year-old girl with a homozygous mutation in the CARD9 gene (Q295X). Pediatr. Infect. Dis. J. 34, 999–1002. doi: 10.1097/INF.0000000000000736
Jachiet, M., Lanternier, F., Rybojad, M., Bagot, M., Ibrahim, L., Casanova, J. L., et al. (2015). Posaconazole treatment of extensive skin and nail dermatophytosis due to autosomal recessive deficiency of CARD9. JAMA Dermatol. 151, 192–194. doi: 10.1001/jamadermatol.2014.2154
Jones, N., Garcez, T., Newman, W., and Denning, D. (2016). Endogenous Candida endophthalmitis and osteomyelitis associated with CARD9 deficiency. BMJ Case Rep. 3:2016. doi: 10.1136/bcr-2015-214117
Lanternier, F., Barbati, E., Meinzer, U., Liu, L., Pedergnana, V., Migaud, M., et al. (2015a). Inherited CARD9 deficiency in 2 unrelated patients with invasive Exophiala infection. J. Infect. Dis. 211, 1241–1250. doi: 10.1093/infdis/jiu412
Lanternier, F., Mahdaviani, S. A., Barbati, E., Chaussade, H., Koumar, Y., Levy, R., et al. (2015b). Inherited CARD9 deficiency in otherwise healthy children and adults with Candida species-induced meningoencephalitis, colitis, or both. J. Allergy Clin. Immunol. 135, 1558.e2–1568.e2. doi: 10.1016/j.jaci.2014.12.1930
Lanternier, F., Pathan, S., Vincent, Q. B., Liu, L., Cypowyj, S., Prando, C., et al. (2013). Deep dermatophytosis and inherited CARD9 deficiency. N. Engl. J. Med. 369, 1704–1714. doi: 10.1056/NEJMoa1208487
Liang, P., Wang, X., Wang, R., Wan, Z., Han, W., and Li, R. (2015). CARD9 deficiencies linked to impaired neutrophil functions against Phialophora verrucosa. Mycopathologia 179, 347–357. doi: 10.1007/s11046-015-9877-2
Pruszkowski, A., Bourgault Villada, I., Cremer, G., Ammar-Khodja, A., Emilie, D., and Revuz, J. (1995). Dermatophytic disease: role of type TC2 CD8 lymphocytes. Ann. Dermatol. Venereol. 122(Suppl. 1), 55.
Rieber, N., Gazendam, R. P., Freeman, A. F., Hsu, A. P., Collar, A. L., Sugui, J. A., et al. (2016). Extrapulmonary Aspergillus infection in patients with CARD9 deficiency. JCI Insight 1:e89890. doi: 10.1172/jci.insight.89890
Sari, S., Dalgic, B., Muehlenbachs, A., DeLeon-Carnes, M., Goldsmith, C. S., Ekinci, O., et al. (2018). Prototheca zopfii colitis in inherited CARD9 deficiency. J. Infect. Dis. 218, 485–489. doi: 10.1093/infdis/jiy198
Taylor, P. R., Tsoni, S. V., Willment, J. A., Dennehy, K. M., Rosas, M., Findon, H., et al. (2007). Dectin-1 is required for beta-glucan recognition and control of fungal infection. Nat. Immunol. 8, 31–38. doi: 10.1038/ni1408
Vaezi, A., Mardani, M., Fakhim, H., Hedayat Yaghoobi, M., Abtahian, Z., Nasri, E., et al. (2018). Severe disseminated phaeohyphomycosis in a patient with inherited CARD9 deficiency. Arch. Clin. Infect. Dis. e84006. doi: 10.5812/archcid.84006
Vinh, D. C. (2011). Insights into human antifungal immunity from primary immunodeficiencies. Lancet Infect. Dis. 11, 780–792. doi: 10.1016/S1473-3099(11)70217-1
Wang, X., Wang, A., Wang, X., Li, R., and Yu, J. (2018a). Cutaneous mucormycosis caused by Mucor irregularis in a patient with CARD9 deficiency. Br. J. Dermatol. doi: 10.1111/bjd.17144 [Epub ahead of print].
Wang, X., Zhang, R., Wu, W., Song, Y., Wan, Z., Han, W., et al. (2018b). Impaired specific antifungal immunity in CARD9-deficient patients with phaeohyphomycosis. J. Invest. Dermatol. 138, 607–617. doi: 10.1016/j.jid.2017.10.009
Wang, X., Wang, W., Lin, Z., Wang, X., Li, T., Yu, J., et al. (2014). CARD9 mutations linked to subcutaneous phaeohyphomycosis and TH17 cell deficiencies. J. Allergy Clin. Immunol. 133, 905–908. doi: 10.1016/j.jaci.2013.09.033
Yamamoto, H., Nakamura, Y., Sato, K., Takahashi, Y., Nomura, T., Miyasaka, T., et al. (2014). Defect of CARD9 leads to impaired accumulation of gamma interferon-producing memory phenotype T cells in lungs and increased susceptibility to pulmonary infection with Cryptococcus neoformans. Infect. Immun. 82, 1606–1615. doi: 10.1128/IAI.01089-13
Keywords: severe fungal infections, CARD9 deficiency, mutation, candidiasis, dermatophytosis
Citation: Vaezi A, Fakhim H, Abtahian Z, Khodavaisy S, Geramishoar M Alizadeh A, Meis JF and Badali H (2018) Frequency and Geographic Distribution of CARD9 Mutations in Patients With Severe Fungal Infections. Front. Microbiol. 9:2434. doi: 10.3389/fmicb.2018.02434
Received: 11 July 2018; Accepted: 24 September 2018;
Published: 12 October 2018.
Edited by:
Martin Hoenigl, University of California, San Diego, United StatesReviewed by:
Aleksandra Barac, University of Belgrade, SerbiaCopyright © 2018 Vaezi, Fakhim, Abtahian, Khodavaisy, Geramishoar, Alizadeh, Meis and Badali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hamid Badali, YmFkYWxpaUB5YWhvby5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.