- 1Department of Physiotherapy, Bayero University Kano, Kano, Nigeria
- 2Department of Physiotherapy and Rehabilitation Sciences, University of Antwerp, Antwerp, Belgium
The present global pandemic of COVID-19 has brought the whole world to a standstill, causing morbidity, death, and changes in personal roles. The more common causes of morbidity and death in these patients include pneumonia and respiratory failure, which cause the patients to require artificial ventilation and other techniques that can improve respiratory function. One of these techniques is chest physiotherapy, and this has been shown to improve gas exchange, reverse pathological progression, and reduce or avoid the need for artificial ventilation when it is provided very early in other respiratory conditions. For patients with COVID-19, there is limited evidence on its effect, especially in the acute stage and in patients on ventilators. In contrast, in patients after discharge, chest physiotherapy in the form of respiratory muscle training, cough exercise, diaphragmatic training, stretching exercise, and home exercise have resulted in improved FEV1 (L), FVC (L), FEV1/FVC%, diffusing lung capacity for carbon monoxide (DLCO%), endurance, and quality of life, and a reduction in anxiety and depression symptoms. However, there are still controversies on whether chest physiotherapy can disperse aerosols and accelerate the rate of spread of the infection, especially since COVID-19 is highly contagious. While some authors believe it is possible, others believe the aerosol generated by chest physiotherapy is not within respirable range. Therefore, measures such as the use of surgical masks, tele-rehabilitation, and self-management tools can be used to limit cross-infection.
Introduction
Coronavirus 2019 (COVID-19), more recently known as SARS-COV-2, is a coronavirus that belongs to the β-corona cluster that is spread to a large extent via droplets (1). When one contracts the infection, the virus gets into the lungs and is received by angiotensin-converting enzyme 2 (ACE2), which is expressed in normal humans in types I and II alveolar cells (2). When the virus binds with ACE2, it damages the alveolar cells (1). The alveolar cells function under normal circumstances to synthesize and secrete surfactant, carry out xenobiotic metabolism, help with transepithelial movement of water, and regenerate alveolar epithelium following lung injury (3). These aforementioned functions help with normal lung functions. Therefore, damage to the alveolar cells may result in respiratory problems, other systemic manifestations, and eventually death (1, 4). Consequently, clinical manifestations of COVID-19 disease include fever, cough, myalgia or fatigue, pneuomia, and complicated dyspnea (4).
In addition, when the respiratory symptoms are severe, they may progress to respiratory failure (acute respiratory distress syndrome), which could lead to death unless it is managed promptly using invasive ventilation (4–6). However, for those with mild to moderate symptoms, non-invasive techniques such as chest physiotherapy can be used (6). The aim of this article is to critically review the nature of respiratory problems in patients with COVID-19 and the safety and efficacy of the use of chest physiotherapy for these patients. Therefore, for the purpose of this review, PubMed and Google Scholar were searched using COVID-19, chest physiotherapy, and pulmonary rehabilitation as keywords.
The Nature of Acute Respiratory Distress Syndrome in Patients With COVID-19
Acute respiratory distress syndrome (ARDS) in COVID-19 usually begins a bit later than in other ARDS. The onset is usually between 8 and 12 days after infection (7–9). It is usually characterized by a dry cough, which is said to be due to respiratory epithelial cells being affected more than the endothelial cells (10). Consequently, the patients usually present with mild symptoms of cough and dyspnea with no exudation that are inconsistent with laboratory and imaging findings including the presence of ground-glass opacities and basilar opacities and lymphocytopenia (8, 10–15). In contrast, some patients, especially those with comorbidities such as neuromuscular disorders and chronic obstructive pulmonary disorders, may at the same time or later develop exudative consolidation and mucous hyper-secretion along with difficulty in clearing the secretions (15). However, even in those presenting with mild symptoms, the dyspnea may progress quite rapidly and cause the patients to require ventilation (12, 16). Therefore, it is important to be on the alert and ready to use a ventilator for the patients if available. If ventilators are not available, other non-invasive techniques such chest physiotherapy can be used on a case-by-case basis (6, 17).
Effects and Safety of Chest Physiotherapy in Patients With Other Respiratory Conditions and COVID-19
Chest physiotherapy has been used in many different respiratory conditions. It has been said to improve gas exchange, reverse pathological progression, and reduce or avoid the need for artificial ventilation when it is provided very early (18, 19). However, for patients with COVID-19, evidence is still lacking on its effects, especially during the acute stage, aside from some position papers or recommendations based on anecdotal evidence (15, 17, 20). This is because the features of respiratory problems in patients with COVID-19 significantly differ from those in other respiratory conditions. For instance, during the acute stage, patients with COVID-19 do not usually have exudation (10, 15). In addition, dyspnea in patients with COVID-19 may rapidly progress to acute respiratory failure (4, 5). Consequently, timely use of mechanical ventilation in such situations is strongly recommended (15, 17, 20).
COVID-19 is highly infectious and spreads rapidly, and there have been concerns about the use of chest physiotherapy in infectious diseases. This is because it has been argued that chest physiotherapy may cause aerosolization (21). This may increase the rate at which COVID-19 spreads. However, later findings in similar conditions disproved this view. According to Simonds and colleagues, an evaluation of droplet dispersion in Influenza pandemic and other airborne infections showed that chest physiotherapy significantly and predominantly produced droplets of >10 μm (22). Droplets of this size are not respirable, as only droplets within inspirable range (about 5 μm) can play a significant role in the transmission of infections (23). Similarly, a review of aerosol transmission of Influenza A virus cast doubt on whether it is even possible for droplets from chest physiotherapy to transmit infections (24). In addition, in SARS, a disease that shared similar pathophysiology with COVID-19 (7, 25), chest physiotherapy was later recommended (26). Furthermore, overall, the management of COVID-19 is as yet symptomatic, as scientists are still trying to understand its pathophysiology and the viral behavior (1, 27). Therefore, since the disease can kill within days to a month of onset, especially in the elderly and those with weak immunity (9, 28), we can make our patients sneeze or cough out sputum into disposable plastic bags during and after chest physiotherapy to prevent or reduce the chance of aerosolization. A similar measure was recommended previously (20).
Similarly, we can disinfect the surrounding environment, while at the same time, the therapists and other health workers wear protective gear to protect themselves from infection. In this way, we can save the lives of tens of thousands of people who might be infected with COVID-19. However, if surgical masks are available, the patients can wear them during the procedure to prevent the spread of the infection (17). Use of surgical masks and oxygen masks on the face of the patients has been found to deflect aerosols during chest compression in a simulation and cadaver model (29). In addition, other means such as the use self-management techniques such as the provision of self-management pamphlets and educational videos or consultations online, such as via Skype video communications, to help patients manage themselves 24 h a day can be explored (20). This will help reduce the chances of cross-infection.
For patients with COVID-19, the aim of chest physiotherapy is to alleviate dyspnea and relieve anxiety and depression in the short term (6, 20); in the long term, it is to improve physical functions, which will in turn improve quality of life and aid return to society (6, 20). Consequently, the chest physiotherapy interventions recommended and/or used for patients with COVID-19 include airway clearance techniques (active cycle of breathing technique, forced expiratory technique, percussion and vibrations, positive expiratory pressure (PEP) therapy (including bubble PEP), positioning and gravity-assisted postural drainage, intra- or extrapulmonary high-frequency oscillation devices, autogenic drainage), secretion clearance removal (huff and cough, suctioning, assisted or stimulated cough maneuvers, cough assist machine), and mobilization and exercise prescription, which may trigger a cough and/or sputum expectoration (15, 30). However, it has been recommended that rehabilitation should be provided on a case-by-case basis since patients differ in their clinical characteristics (15, 17, 20).
Chest Physiotherapy During the Acute Period
During this stage, most patients have no exudation, and as such, chest physiotherapy may not be recommended (15). In addition, procedures such as diaphragmatic breathing, pursed-lip breathing, and bronchial hygiene/ lung re-expansion techniques are contraindicated during this stage (17). The priority here is the use of a mechanical ventilator, especially in those with severe symptoms (6, 17). For those with exudation and mild to moderate symptoms, it has been argued that chest physiotherapy can be used to relieve dyspnoea and depression and anxiety on a case-by-case basis (6, 15). However, to date, there are no studies reporting on the use of chest physiotherapy during the acute stage aside from a recommendation based on anecdotal evidence (17).
Chest Physiotherapy During Mechanical Ventilation
Under mechanical ventilation, patients may lose spontaneous breathing (31). This can predispose the patients to developing lung collapse and ventilator-associated pneumonia. In such circumstances, chest physiotherapy can be used to reduce the length of stay in both a mechanical ventilator and ICU and prevent ventilator-associated pneumonia (32, 33). In addition, high-frequency chest wall oscillation for intubated patients resulted in increased dry sputum weight and PaO2 on day 3, decreased lung collapse on days 2 and 3, and culture positivity on day 3 (33). Similarly, in a patient who received 11 sessions of physical therapy consisting of upright body positioning, mobilization and exercise, and the active cycle of breathing exercise technique every 2 h for 12 h over his 48-h stay in the ICU (six sessions on day one and five sessions on day two), arterial oxygen level improved markedly, with radiographic resolution of infiltration (18). Therefore, since chest physiotherapy reverses pathological progression, prevents atelectasis, improves impaired gas exchange, and decreases culture positivity, which are also some of the pathological hallmarks of COVID-19, it can be utilized in patients with this disease.
Accordingly, the techniques recommended in patients who are on a ventilator include airway clearance techniques, lung maneuver recruitment, endotracheal suctioning, and change in posture (17, 20). The airway clearance techniques recommended include positioning, active cycle of breathing, manual and/or ventilator hyperinflation, percussion and vibration, positive expiratory pressure (PEP), and mechanical insuflation-ensufflation (15, 17). However, there are no details on how to perform these techniques aside from positioning therapy, and there have been no studies yet in patients with COVID-19 reporting on the efficacy of the techniques. See Table 1 for details of the positioning therapy technique. In addition, lung maneuver recruitment needs to be used with caution since it may have severe adverse effects (34). Furthermore, chest physiotherapy during this period is indicated or contraindicated based on the status of the respiratory, cardiovascular, and neurological functions of the patients. See Table 2 for details of the indications and the contraindications.
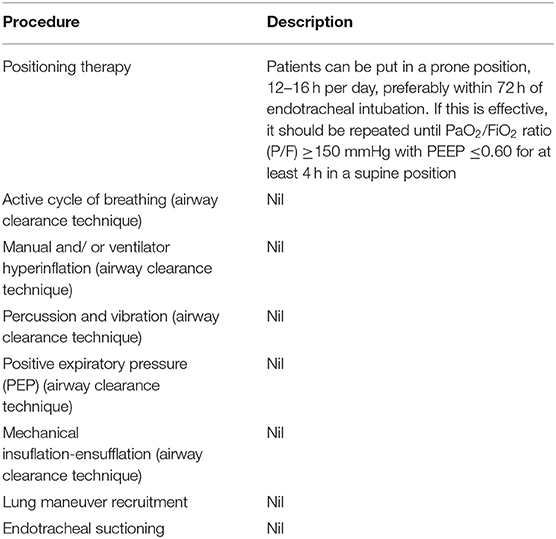
Table 1. Description of the chest physiotherapy (positioning therapy) used in patients with COVID-19 during mechanical ventilation [adopted from (17)].
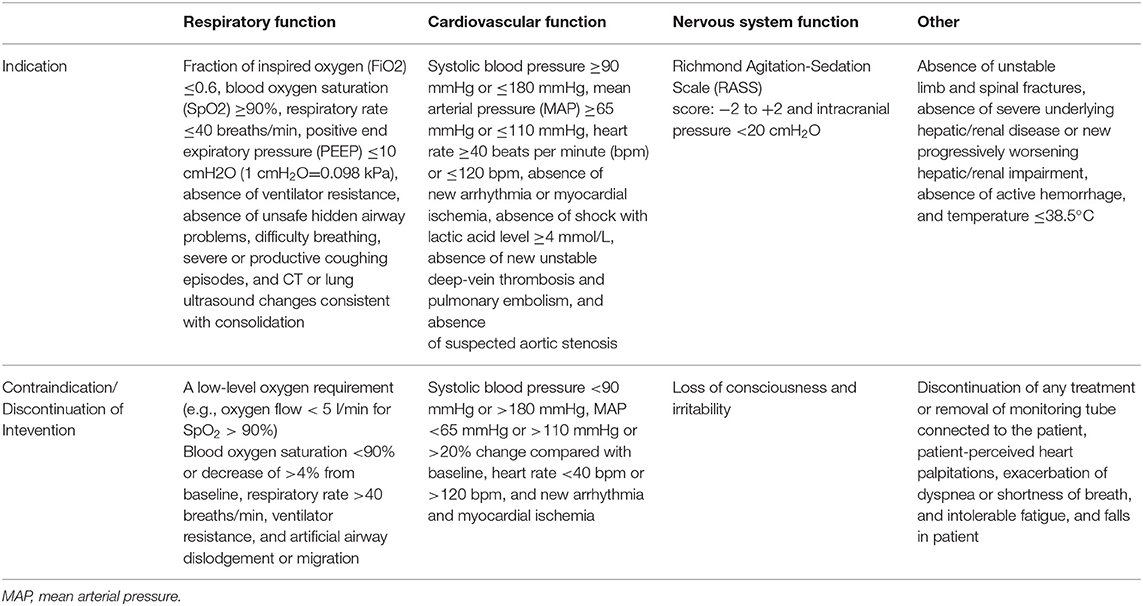
Table 2. Indications and contraindications of chest physiotherapy in patients in mechanical ventilations [adopted from (15, 17, 20)].
Post-Extubation and After Discharge
Post-extubation, many patients may develop respiratory failure again (35). This can be prevented using chest vibration and percussion (36). In patients with COVID-19, there seem to be no reports on the use of chest physiotherapy immediately post-extubation. However, following discharge, rehabilitation involving respiratory muscle training, cough exercise, diaphragmatic training, stretching exercise, and home exercise has been applied (30). These forms of training and exercise, when performed for two sessions per week for 6 weeks, resulted in improved FEV1 (L), FVC (L), FEV1/FVC%, diffusing lung capacity for carbon monoxide (DLCO%), endurance, and quality of life and a reduction in anxiety and depression symptoms. See Tables 3, 4 for the indications and contraindications of chest physiotherapy and descriptions of the techniques used during this stage, respectively.
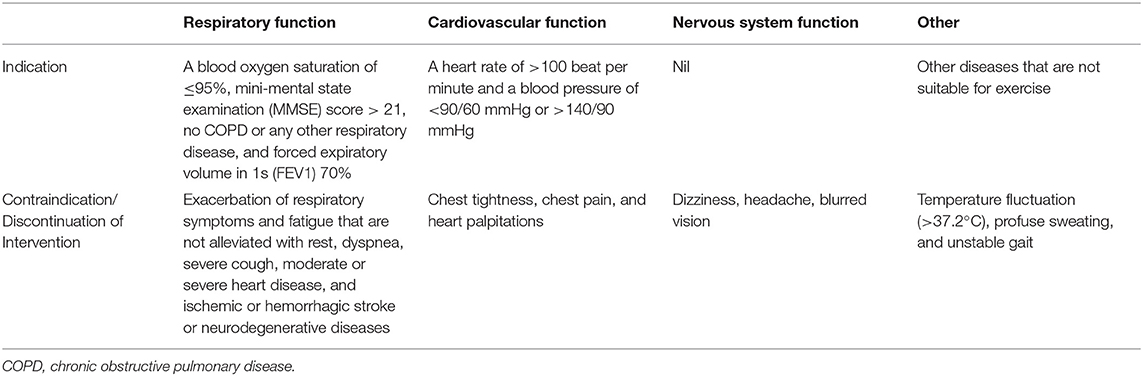
Table 3. Indications and contraindications of chest physiotherapy in patients in after discharge [adopted from (20, 30)].
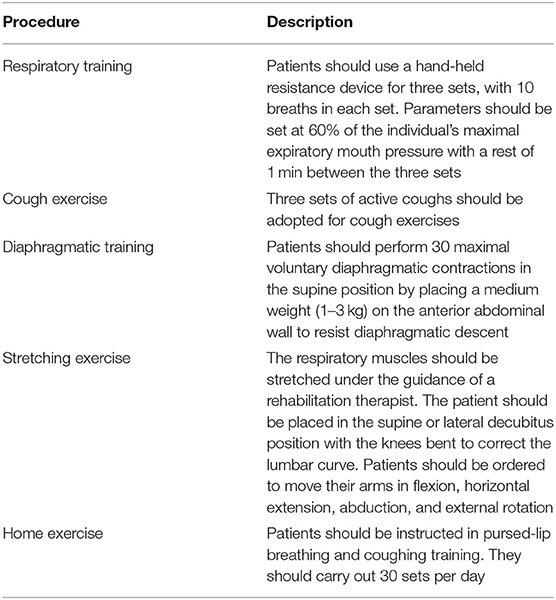
Table 4. Description of the chest physiotherapy used in patients with COVID-19 after discharge [adopted from (30)].
Conclusion
Chest physiotherapy may improve respiratory functions and quality of life in patients with COVID-19, especially after discharge. During the acute stage, evidence is still lacking on its usefulness, aside from some professional recommendations based on anecdotal evidence. However, it should be noted that chest physiotherapy is an individualized treatment based on the patient's particular presentations. Therefore, when patients present with symptoms that can benefit from chest physiotherapy, it may be given while the patients are closely observed for any adverse events. In addition, when administering chest physiotherapy for patients in the acute stage, measures such as the use of surgical masks, if available, should be taken to prevent cross-infection.
Author Contributions
AA contributed solely to the conception, writing, and all sections of this article.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. (2020) 92:1–4. doi: 10.1002/jmv.25722
2. Zhao Y, Zhao Z, Wang Y, Zhou Y, Ma Y, Zuo W. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. bioRxiv. (2020). doi: 10.1101/2020.01.26.919985
3. Castranova V, Rabovsky J, Tucker JH, Miles PR. The alveolar type II epithelial cell: a multifunctional pneumocyte. Toxicol Appl Pharmacol. (1988) 93:472–83. doi: 10.1016/0041-008x(88)90051-8
4. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
5. Ahmed A, Shah RJ, Gul Rahim SEG, Flores M, O'Linn A. Coronavirus Disease 2019 (COVID-19) Complicated by Acute Respiratory Distress syndrome: an internist's perspective. Cureus. (2020) 12:e7482. doi: 10.7759/cureus.7482
6. Yang L-L, Yang T. Pulmonary rehabilitation for patients with coronavirus disease 2019 (COVID-19). Chronic Dis Transl Med. (2020) 6:79–86. doi: 10.1016/j.cdtm.2020.05.002
7. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. doi: 10.1016/S0140-6736(20)30211-7
8. Guan WJ, Zhong NS. Clinical characteristics of COVID- 19 in China. N Engl J Med. (2020) 382:1859–62. doi: 10.1056/NEJMc2005203
9. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. (2020) 305:1054–62. doi: 10.1016/S0140-6736(20)30566-3
10. Li X, Ma X. Acute respiratory failure in COVID-19: is it “typical” ARDS? Critical Care. (2020) 24:198. doi: 10.1186/s13054-020-02911-9
11. Alberti P, Beretta S, Piatti M, Karantzoulis A, Piatti ML, Santoro P, et al. Guillain-Barré syndrome related to COVID-19 infection. Neurol Neuroimmunol Neuroinflamm. (2020) 7:e741. doi: 10.1212/NXI.0000000000000741
12. Virani A, Rabold E, Hanson T, Haag A, Elrufay R, Cheema T, et al. Guillain-Barré Syndrome associated with SARS-CoV-2 infection [published online ahead of print, 2020 Apr 18]. IDCases. (2020) 20:e00771. doi: 10.1016/j.idcr.2020.e00771
13. Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. (2020) 19:383–4. doi: 10.1016/S1474-4422(20)30109-5
14. Padroni M, Mastrangelo V, Asioli GM, Pracucci G, Padroni M, Renieri L, et al. Guillain-Barré syndrome following COVID-19: new infection, old complication? J Neurol. (2020) 267:1877–9. doi: 10.1007/s00415-020-09849-6
15. Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiotherapy. (2020) 66:73–82. doi: 10.1016/j.jphys.2020.03.011
16. Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, Cuzzoni MG, et al. Guillain-Barre syndrome associated with SARS-CoV-2. N Eng J Med. (2020) 382:2574–76. doi: 10.1056/NEJMc2009191
17. Lazzeri M, Lanza A, Bellini R, Bellofiore A, Cecchetto S, Colombo A, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR). Monaldi Arch Chest Dis. (2020) 90:163–7. doi: 10.4081/monaldi.2020.1285
18. Wong WP. Physical therapy for a patient in acute respiratory failure. Phys Ther. (2000) 80:662–70. doi: 10.1093/ptj/80.7.662
19. Wilson LM, Morrison L, Robinson KA. Airway clearance techniques for cystic fibrosis: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. (2019) 1:CD011231. doi: 10.1002/14651858.CD011231.pub2
20. Zhao H-M, Xie Y-X, Wang C. Recommendations for respiratory rehabilitation in adults with COVID-19. Chin Med J. (2020). doi: 10.1097/CM9.0000000000000848
21. Cooke FJ, Shapiro DS. Global outbreak of severe acute respiratory syndrome (SARS). Int J Infect Dis. (2003) 7: 80–5. doi: 10.1016/S1201-9712(03)90001-4
22. Simonds AK, Hanak A, Chatwin M, Morrell MJ, Hall A, Parker KH, et al. Evaluation of droplet dispersion during non-invasive ventilation, oxygen therapy, nebuliser treatment and chest physiotherapy in clinical practice: implications for management of pandemic influenza and other airborne infections. Health Technol Assess. (2010) 14:131–72. doi: 10.3310/hta14460-02
23. Brankston G, Gitterman L, Hiriji Z, Lemieux C, Gardam M. Transmission of influenza A in human beings. Lancet Infect Dis. (2007) 7:257–65. doi: 10.1016/S1473-3099(07)70268-2
24. Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis. (2006) 12:1657–62. doi: 10.3201/eid1211.060426
25. Hui DS, Azhar IE, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global healt h–the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. (2020) 91:264–66. doi: 10.1016/j.ijid.2020.01.009
26. Mehta SR, Sashindran VK, Kumar K, Gupta A. Severe acute respiratory syndrome: an update. Med J Armed Forces India. (2007) 63:52–5. doi: 10.1016/S0377-1237(07)80110-9
27. Adhikari SP, Meng S, Wu1 Y-J, Mao Y-P, Ye R-X, Wang Q-Z, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. (2020) 9:29. doi: 10.1186/s40249-020-00646-x
28. CDC. 2019 Novel Coronavirus. Wuhan (2020). Available online at: https://www.cdc.gov/coronavirus/2019-nCoV/summary.html. (accessed April 1, 2020).
29. Ott M, Milazzo A, Liebau S, Jaki C, Schilling T, Krohn A, et al. Exploration of strategies to reduce aerosol-spread during chest compressions: a simulation and cadaver model. Resuscitation. (2020) 152:192–8. doi: 10.1016/j.resuscitation.2020.05.012
30. Liu K, Weitong Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Compl Therap Clin Pract. (2020) 39:101166. doi: 10.1016/j.ctcp.2020.101166
31. Castro AA, Calil SR, Freitas SA, Oliveira AB, Porto EF. Chest physiotherapy effectiveness to reduce hospitalization and mechanical ventilation length of stay, pulmonary infection rate and mortality in ICU patients. Respir Med. (2013) 107:68–74. doi: 10.1016/j.rmed.2012.09.016
32. Ntoumenopoulos G, Presneill JJ, McElholum M, Cade JF. Chest physiotherapy for the prevention of ventilator-associated pneumonia. Intensive Care Med. (2002) 28:850–6. doi: 10.1007/s00134-002-1342-2
33. Kuyrukluyildiz U, Binici O, Kupeli I, Erturk N, Gulhan B, Akyol F, et al. What is the best pulmonary physiotherapy method in ICU? Can Respir J. (2016) 2016:4752467. doi: 10.1155/2016/4752467
34. Cavalcanti AB, Suzumura EA, Laranjeira LN, Paisani DM, Damiani LP, Guimarães HP, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. (2017) 318:1335–45. doi: 10.1001/jama.2017.14171
35. Thille AW, Contou D, Fragnoli C, Córdoba-Izquierdo A, Boissier F, Brun-Buisson C. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care. (2013) 17:R269. doi: 10.1186/cc13103
Keywords: physiotherapy, pneumonia, COVID-19, mortality, ventilator, critical care
Citation: Abdullahi A (2020) Safety and Efficacy of Chest Physiotherapy in Patients With COVID-19: A Critical Review. Front. Med. 7:454. doi: 10.3389/fmed.2020.00454
Received: 02 April 2020; Accepted: 08 July 2020;
Published: 21 July 2020.
Edited by:
Ata Murat Kaynar, University of Pittsburgh School of Medicine, United StatesReviewed by:
Evgenia V. Fot, Northern State Medical University, RussiaLongxiang Su, Peking Union Medical College Hospital (CAMS), China
Copyright © 2020 Abdullahi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Auwal Abdullahi, YWFiZHVsbGFoaS5wdGhAYnVrLmVkdS5uZw==
 Auwal Abdullahi
Auwal Abdullahi