- 1Department of Intensive Care, Amsterdam University Medical Centers, Vrije Universiteit Amsterdam, Amsterdam, Netherlands
- 2Department of Anesthesiology, Amsterdam University Medical Centers, Vrije Universiteit Amsterdam, Amsterdam, Netherlands
- 3Department of Anesthesiology, Noordwest Ziekenhuisgroep, Alkmaar, Netherlands
- 4Department of Pulmonary Diseases, Amsterdam University Medical Centers, Vrije Universiteit Amsterdam, Amsterdam, Netherlands
- 5Department of Epidemiology and Biostatistics, Amsterdam University Medical Centers, Vrije Universiteit Amsterdam, Amsterdam, Netherlands
- 6Research VUmc Intensive Care (REVIVE), Amsterdam University Medical Centers, Vrije Universiteit, Amsterdam, Netherlands
Background: Atelectasis frequently develops in critically ill patients and may result in impaired gas exchange among other complications. The long-term effects of bronchoscopy on gas exchange and the effects on respiratory mechanics are largely unknown.
Objective: To evaluate the effect of bronchoscopy on gas exchange and respiratory mechanics in intensive care unit (ICU) patients with atelectasis.
Methods: A retrospective, single-center cohort study of patients with clinical indication for bronchoscopy because of atelectasis diagnosed on chest X-ray (CXR).
Results: In total, 101 bronchoscopies were performed in 88 ICU patients. Bronchoscopy improved oxygenation (defined as an increase of PaO2/FiO2 ratio > 20 mmHg) and ventilation (defined as a decrease of > 2 mmHg in partial pressure of CO2 in arterial blood) in 76 and 59% of procedures, respectively, for at least 24 h. Patients with a low baseline value of PaO2/FiO2 ratio and a high baseline value of PaCO2 were most likely to benefit from bronchoscopy. In addition, in intubated and pressure control ventilated patients, respiratory mechanics improved after bronchoscopy for up to 24 h. Mild complications, and in particular desaturation between 80 and 90%, were reported in 13% of the patients.
Conclusions: In selected critically ill patients with atelectasis, bronchoscopy improves oxygenation, ventilation, and respiratory mechanics for at least 24 h.
Background
In critically ill patients, mechanical ventilation might cause ventilator-induced lung injury and hospital-acquired pneumonia, both conditions promote atelectasis and stagnant secretions that may worsen oxygenation and delay weaning from ventilator (1, 2).
Atelectasis may result from numerous causes, for example, from congestion of mucus in the central airways, from increased sputum production, from decreased mucociliary clearance, from decreased cough effectiveness, from increased sputum viscosity, or by a combination of these factors. Treatment of atelectasis in intensive care unit (ICU) patients has been focused on blind airway suctioning, bronchoscopy with or without adjuncts such as nebulization of N-acetylcysteine, and chest physiotherapy. Bronchoscopy is regarded as an attractive method for endobronchial mucus clearing, which possibly results in a more effective airway clearance as it is performed under direct visualization of the airways.
However, the current literature on the effectiveness of bronchoscopy in the treatment of atelectasis is limited. A systematic review concluded that bronchoscopy could be effective in the treatment of atelectasis. The success rates (defined as radiographic improvement on chest X-ray [CXR] or an improved PaO2/PAO2 ratio) in the ICU patient population had, however, a remarkably wide range of 19–89% (3). Moreover, the effect of bronchoscopy on lung mechanics is largely unknown, which may be of importance in reducing the work of breathing. Furthermore, the superiority of bronchoscopy over blind airway suctioning on clinical relevant endpoints, such as gas exchange, has also not been established (4).
The lack of consistency in the study design in previous case studies (3–11), such as small groups, large variation in the study population, wide range of success, and studies not looking specifically at atelectasis, represents important limitations in the current scientific evidence about bronchoscopy in ICU patients. As such, additional studies are needed to explore further the role of bronchoscopy in atelectasis in this group of patients.
We have hypothesized that bronchoscopy for atelectasis in the ICU improves gas exchange and respiratory mechanics, as assessed by an increase in PaO2/FiO2 of more than 20 mmHg or by a decrease in PaCO2 of more than 2 mm Hg, combined with an increase in dynamic lung compliance, for up to 24 h after intervention. Furthermore, we have aimed to determine the safety of bronchoscopy and predictors for clinical improvement.
Material and Methods
Design: A retrospective, single-center cohort study.
Setting: The ICU of an academic hospital in Amsterdam from January 2011 till July 2015.
Patients: Adult patients (>18 years old) who underwent a bronchoscopy because of atelectasis on CXR and in which the standard therapy failed. Standard care consisted of blind suctioning of the airways, airway nebulization (with bronchodilators and/or N-acetylcysteine), and chest physiotherapy. We excluded 28 patients whose exact time of bronchoscopy was lacking from the electronic medical record.
Procedure: Shortly before and during the bronchoscopy, the fractional inspired oxygen was raised to 100%. Mechanical ventilation was continued throughout the procedure in a volume controlled mode with an increased upper limit of maximum airway pressure. Sedation was provided as required and titrated by the intensive care physician. All bronchoscopies were performed by or under the direct supervision of a pulmonologist.
Data and Characteristics
Demographic information, patient characteristics, data on admission, and ventilation were collected for all patients from the electronic medical record system PDMS (Metavision®, IMD-soft, Tel-Aviv, Israel). The outcome variables were abstracted immediately before and 1, 12, and 24 h after the bronchoscopy.
Response to bronchoscopy was deemed as clinically relevant based on the improvement of oxygenation, as defined by an increase in the ratio of arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FiO2 ratio) > 20 mmHg (12, 13), and an improvement of ventilation, defined as a decrease of > 2 mmHg in partial pressure of CO2 in arterial blood (PaCO2) (14). Pdriving was calculated as Peak pressure (Ppeak) − positive end expiratory pressure (PEEP), where Ppeak was used as a surrogate for plateau pressure, which was not available. Dynamic compliance was calculated as tidal volume divided by Ppeak. We defined pneumonia as the combination of positive microbiological culture, purulent sputum, and an infiltration on CXR.
The findings obtained during bronchoscopy were retrieved from bronchoscopy reports. Data on the location of atelectasis and pulmonary infiltrate were retrieved from CXR reports when available. The CXRs were evaluated by a staff radiologist. Radiographic improvement was defined as a resolution of atelectasis and/or increased aeration on CXR.
Statistical Analysis
At the start of the study protocol, we estimated that the study would be able to detect a clinically relevant improvement of oxygenation (PaO2/FiO2 ratio > 20 mmHg) after bronchoscopy (with α level of two-tailed test as 0.05) at a power of 80% if the total sample size was at least 98 cases.
Baseline patient characteristics were recorded and tabulated. Categorical variables were summarized using frequencies and percentages. Normally distributed continuous variables were summarized by mean ± standard deviation (± SD) and non-normally distributed variables by median and interquartile range (IQR).
To examine the longitudinal changes in continuous outcome variables after bronchoscopy, mixed linear models were used with time as the independent (categorical) variable. In case of a significant overall effect of time, post-hoc tests were used to compare means at each of the follow-up times separately with baseline measurement. Residuals were checked for normality. In case the normality assumption was violated, the nonparametric Friedman test followed by a post-hoc testing using Wilcoxon signed-rank testing was used.
Chi-square tests and univariate and multivariate logistic regression analyses were used to identify the predicting factors for clinical improvement after bronchoscopy, with additional ROC curve analysis to determine optimal cutoff points. Covariates included in the multivariable model were those associated with clinical improvement in univariate analyses at a significance level of P < 0.1, and a backward elimination method was used. P < 0.05 was considered as statistically significant. For post-hoc comparisons, a Bonferroni correction was used to account for the three separate comparisons of the follow-up measurements with the baseline. All p-values reported for the post-hoc tests have been corrected for multiple testing and should also be compared to the 0.05 significance level. All statistical analyses were performed using the IBM SPSS 20 statistical software package (SPSS Inc.®, Chicago USA).
Results
Patient Characteristics
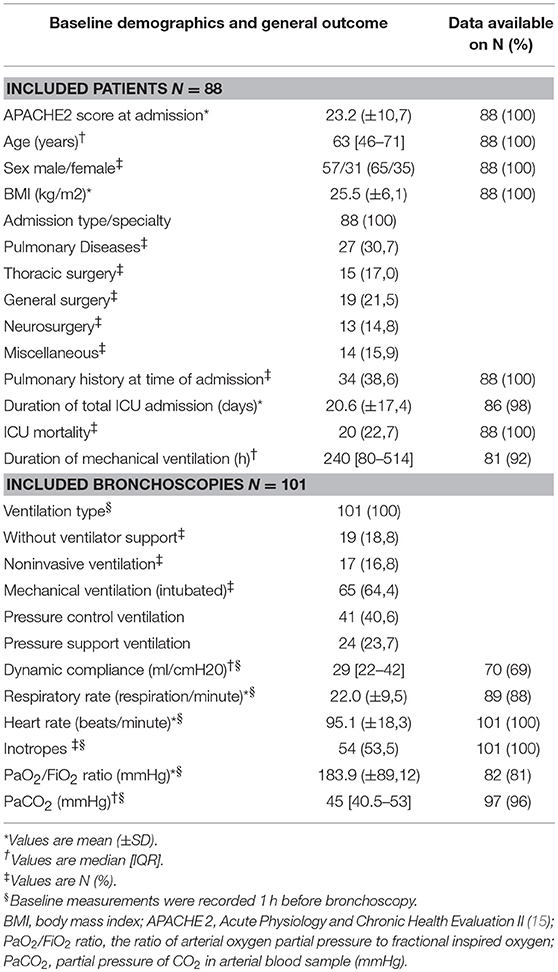
The characteristics of all patients are presented in Table 1. Between January 2011 and July 2015, 129 bronchoscopies were performed for the indication of atelectasis in 116 patients. Of these, 28 patients were excluded due to unsure and/or inadequate recording of bronchoscopy timing, making the total study population amount to 101 bronchoscopies in 88 patients. These 88 patients comprised of 7% of the total ICU population who required > 72 h of mechanical ventilation in the study period. At the time of bronchoscopy, most patients were mechanically ventilated (64%), 17% of the patients were ventilated noninvasively, and only 19% of the patients were without respiratory support.
Bronchoscopy, Radiology and Side Effects
The indication, main findings, and interventions during bronchoscopy are presented in Table 2. Atelectasis of one lobe (59%) was the main indication for bronchoscopy.
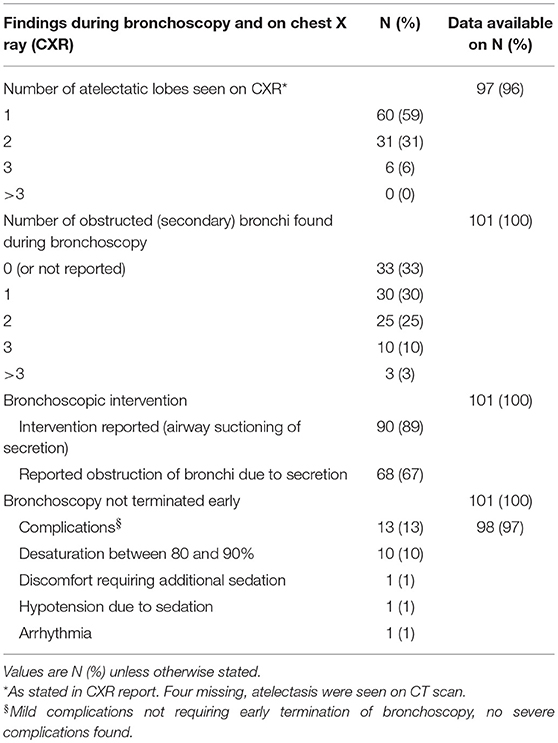
Table 2. Indication, main findings, interventions during bronchoscopy, and associated outcome and side effects.
In 89% of the cases, airway suctioning during bronchoscopy was reported. Obstruction due to this secretion was reported in 67% of the cases. Mostly, obstruction of one bronchus was seen (30%).
Subsequent CXR was performed in 45 subjects and improvement was recorded in 96% of the subjects.
Except for mild complications, occurring in 13% of the subjects, no adverse events were stated. Desaturation, with saturations between 80 and 90%, was encountered the most. None of the bronchoscopies were terminated early (Table 2).
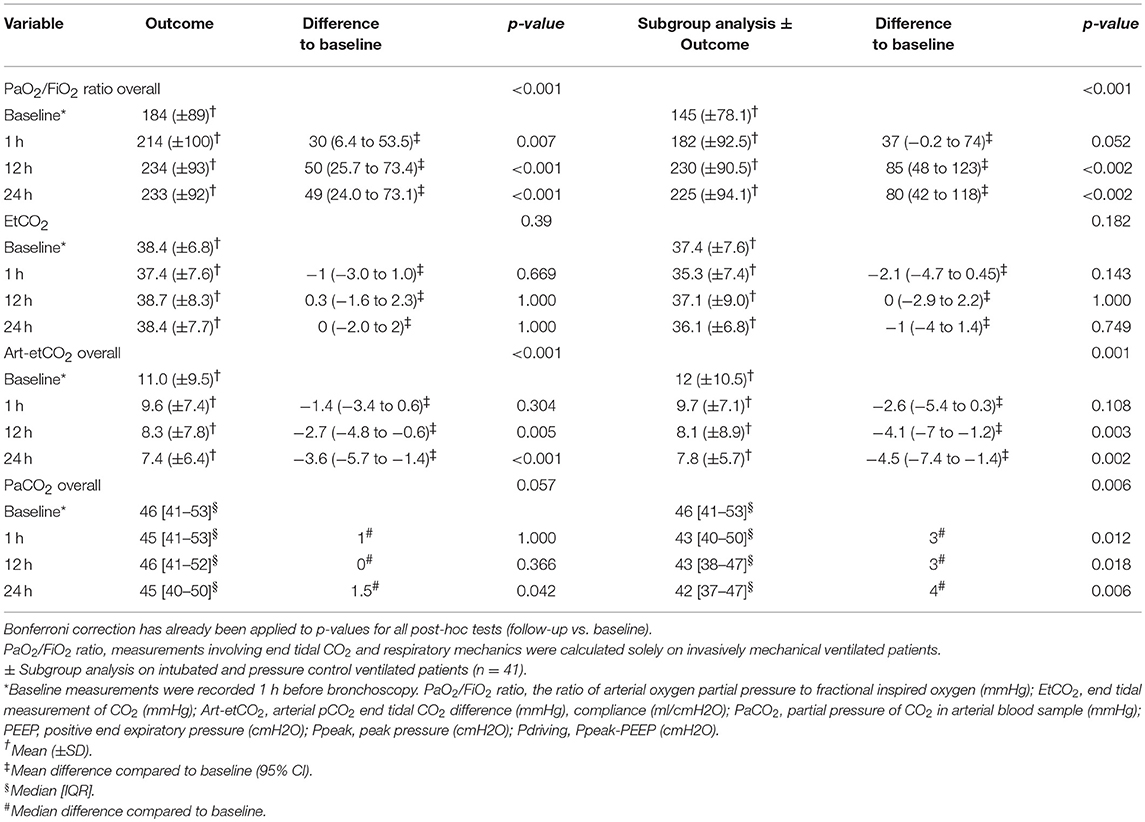
Gas Exchange
Results of bronchoscopy on gas exchange are shown in Table 3. The PaO2/FiO2 ratio and measurements involving end tidal CO2 were calculated solely on invasively mechanical ventilated patients and respiratory mechanics solely on intubated and pressure control ventilated patients.
Clinically relevant improvement of oxygenation was seen in 76% of the subjects and clinically relevant improvement of ventilation in 59% of the subjects. Both oxygenation and ventilation improved in 49% of the subjects.
A statistically significant increase in the PaO2/FiO2 ratio was seen 1, 12, and 24 h after bronchoscopy for all procedures. Arterial-end tidal CO2 difference decreased 12 and 24 h post bronchoscopy. No statistically significant difference was observed for end tidal measurement of CO2 (etCO2). When performing a subgroup analysis on pressure control ventilated patients, these observed differences persisted or became even larger. In case of PaCO2, a statistically significant decrease was found only in the subgroup analysis. No statistically significant changes in oxygenation, ventilation or respiratory mechanics were seen in the cases (representing 11% of the total) in which no intervention was performed during bronchoscopy.
Respiratory Mechanics
Respiratory mechanics were calculated solely on intubated and pressure control ventilated patients. Bronchoscopy improved compliance, Ppeak and Pdriving, while tidal volume remained the same, at 12 h post-bronchoscopy. These results persisted for at least 24 h after bronchoscopy. No statistically significant difference in PEEP was observed at any time after bronchoscopy, so respiratory mechanics improved without adjustment of PEEP (Table 4).
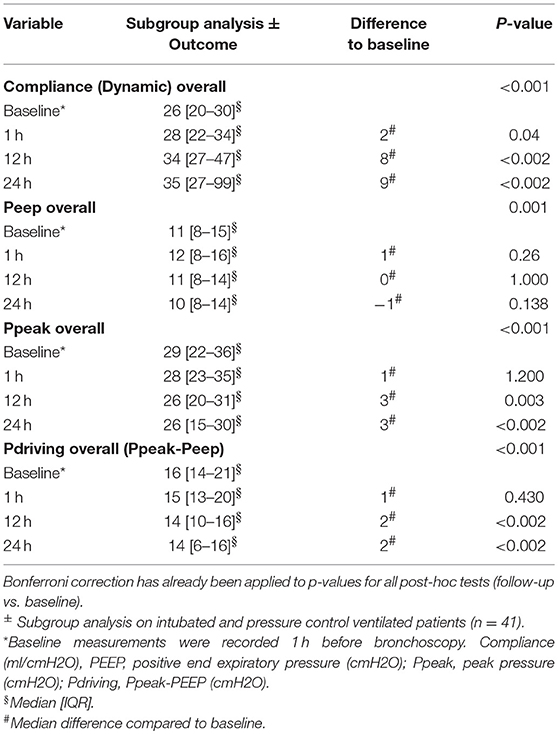
Table 4. Results of bronchoscopy on respiratory mechanics on subgroup intubated, pressure control ventilated patients (n = 41).
All statistically significant changes in gas exchange and respiratory mechanics are shown in Figure 1.
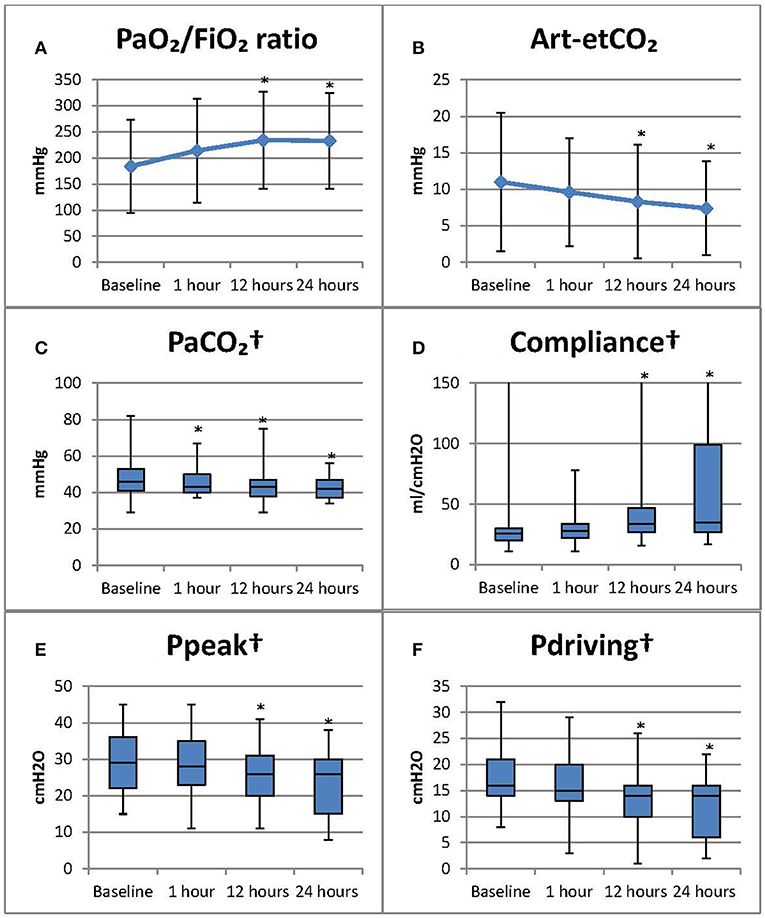
Figure 1. Results of bronchoscopy on gas exchange and respiratory mechanics *Statistically significant change compared to baseline (p < 0.05 Bonferroni correction has already been applied to p-values for all post-hoc tests, follow-up vs. baseline). Baseline measurements were recorded 1 h before bronchoscopy. Subsequent measurements, respectively at 1, 12, and 24 h post bronchoscopy. PaO2/FiO2 ratio, measurements involving end tidal CO2 were calculated solely on invasively mechanical ventilated patients. †Results of subgroup analysis on intubated and pressure control ventilated patients. (A) PaO2/FiO2 ratio: the ratio of arterial oxygen partial pressure to fractional inspired oxygen (mmHg); (B) Art-etCO2: arterial pCO2 end tidal CO2 difference (mmHg); (C) PaCO2: partial pressure of CO2 in arterial blood sample (mmHg); (D) Compliance (ml/cmH2O); (E). Ppeak: peak pressure (cmH2O); (F) Pdriving: Ppeak-PEEP (cmH2O), PEEP: positive end expiratory pressure (cmH2O). PaO2/FiO2 ratio and art-etCO2 presented as median [IQR]; all other parameters as mean (±SD).
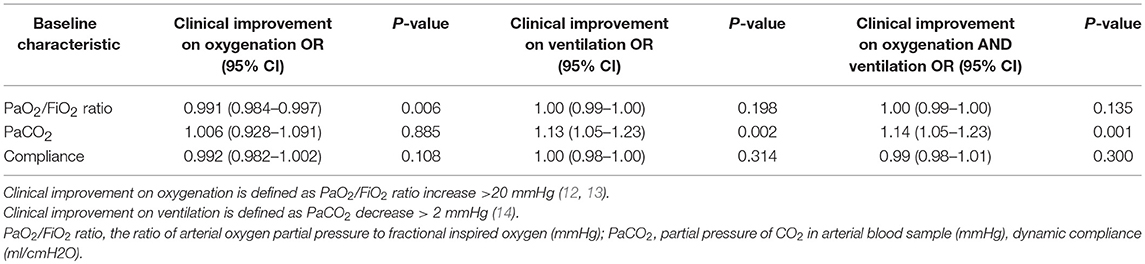
Predictors of Successful Bronchoscopy
To identify individual predictors for clinical improvement after bronchoscopy, univariate logistic regression analyses were performed on several baseline characteristics. Results are presented in Table 5.
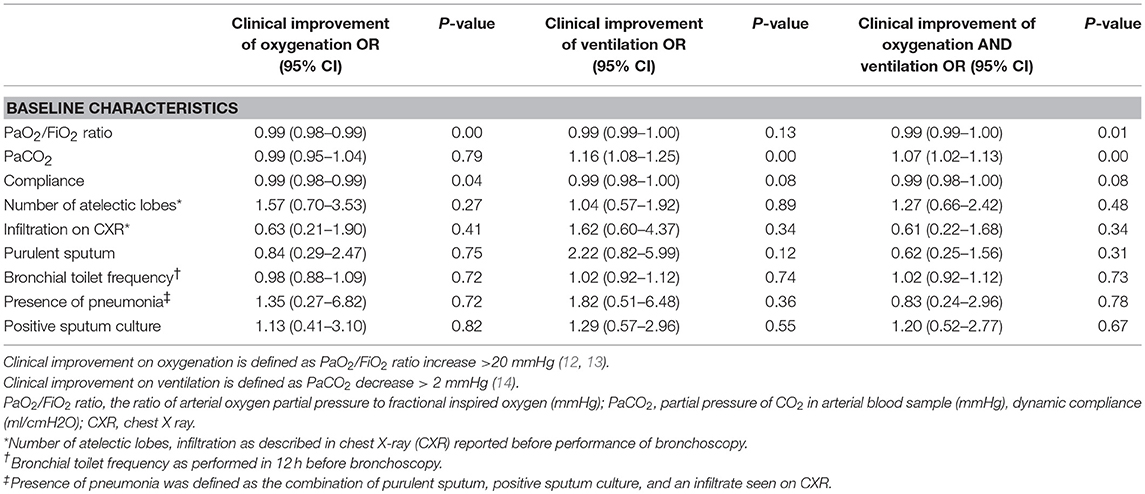
Table 5. Univariable analysis of selected baseline characteristics on clinical improvement of oxygenation.
Of all the variables included, only baseline recordings of a lower PaO2/FiO2 ratio (OR 0.99 95% CI 0.99–1.00 p = 0.01) and higher PaCO2 (OR 1.07 95% CI 1.02,1.13 p < 0.01) were significantly associated with clinical improvement on both oxygenation and ventilation in the univariate analyses. In addition, low compliance (OR 0.99 95% CI 0.98–1.00 p = 0.08) was also included in a multivariate analysis. An association for clinical improvement on oxygenation was found for the baseline recordings of a low PaO2/FiO2 ratio (OR 0.99 95% CI 0.98–0.99 p < 0.01) and low compliance (OR 0.99 95% CI 0.98–1.00 p = 0.04). Additionally, high PaCO2 (OR 1.16 95% CI 1.08–1.25 p < 0.01) and low compliance (OR 0.99 95% CI 0.98–1.00 p = 0.08) were associated with clinical improvement on ventilation.
In the subsequent multivariable analyses, performed on a total of 70 cases due to missing data, only the baseline presence of high levels of PaCO2 remained as a predictive factor for clinical improvement of both oxygenation and ventilation (OR 1.14 95% CI 1.05–1.23 p = 0.001) and ventilation alone (OR 1.13 95% CI 1.05–1.23 p = 0.002). A baseline recording of low PaO2/FiO2 levels was the only remaining parameter that was significantly associated with clinical improvement on oxygenation (OR 0.991 95% CI 0.984–0.997 p = 0.006) (Table 6).
By analyzing PaO2/FiO2 ratio and PaCO2 in a receiver operating characteristic (ROC) curve optimal cutoff points were determined. For PaO2/FiO2 ratio, a baseline value of ≤ 210 mmHg is predictive of clinical improvement on oxygenation after bronchoscopy with a sensitivity of 70% and a specificity of 66%. PaCO2 as predictive of clinical improvement on ventilation alone or on oxygenation and ventilation, a cut-off value of ≥ 44,5 mmHg will render a sensitivity of 72% and specificity of 74% in our patient population.
Discussion
The main results of this study are that bronchoscopy, when performed in the case of atelectasis in critically ill patients, was clinically beneficial in most patients by improving oxygenation (76%), ventilation (59%), or both (49%) for at least 24 h. In addition, in intubated and pressure control ventilated patients, a significant improvement was found in dynamic compliance, Ppeak, and Pdriving, with positive effects lasting for up to 24 h. Patients with a low baseline recording of PaO2/FiO2 and high baseline recording of PaCO2 seemed to benefit the most. Lastly, bronchoscopy was safe in these patients.
While previously published articles have been dominated by the effects of bronchoscopy on re-expansion of the collapsed pulmonary region on CXR (5–10), the clinical course will arguably be dictated more by respiratory mechanics. So, an improvement of long-term gas exchange and respiratory mechanics, as found in this study, will be of more clinical relevance than the aeration on CXR. When reviewing previously published studies that investigated the effects of bronchoscopy, it is noticed that most articles focus on short-term evaluation of gas exchange, finding no statistically significant results, and reported effects on respiratory mechanics are largely missing (4, 6, 16). Today, much emphasis is placed on lung-protective ventilation strategies to reduce ventilator-induced lung injury by maintaining alveolar aeration, preventing overexpansion of the lung, and limiting driving pressure (17). Our study is the first to assess respiratory mechanics after bronchoscopy in this lung protective ventilation perspective. Our results suggest that using bronchoscopy for atelectasis may be an addition to a lung protective strategy when considering the fact that bronchoscopy decreased Ppeak and Pdriving, as required for optimal gas exchange, with results lasting for at least 24 h. This finding merits further studies.
To date, there has been only one study investigating the effects of bronchoscopy on gas exchange and respiratory mechanics for up to 24 h. In Weinstein et al. (11) have shown a significant increase in the ratio of arterial to alveolar oxygen pressures (PaO2/PAO2) at 11 ± 1 h after lavage in 81% of the 43 lavages performed in only 6 patients; 63% of the 43 lavages were associated with a significant increase in effective static compliance at 8 ± 1 h after the lavage.
The long-term improvement of gas exchange might be offset by an initial deterioration after bronchoscopy, as stated by Jolliet and Chevrolet (16). This review of the literature concluded that gas exchange showed initial deterioration as measured by a PaCO2 increase of on average 8.25 mmHg and a PaO2 decrease of between 8.25 and 18.75 mmHg. This is probably being derived from smaller tidal volumes that are delivered while the bronchoscope is in place. When suctioning was applied, this effect became even larger; PaCO2 rose by 30%, while PaO2 decreased by about 40% due to reduced end-expiratory volume and PEEP. The authors stated that normalization takes 15 min in healthy lungs and up to hours in diseased lungs (16). This phenomenon, next to the time necessary for recovery of the ventilation-perfusion mismatch by mitigating hypoxic pulmonary vasoconstriction, can explain that we found no improved gas exchange 1 h after the procedure.
Although the risk of losing lung volume during or after bronchoscopy exists, by either derecruitment, denitrogenation, or negative pressure into the respiratory system, less atelectasis was seen on subsequent CXR (18).
Bronchoscopy can be considered safe in ICU patients, considering the low complication rate found in our study, which is comparable to several previous publications (10, 19, 20). The most recent and largest publication on safety of bronchoscopy in mechanically ventilated ICU patients with sepsis, septic shock, and/or acute lung injury/acute respiratory distress syndrome prospectively collected data on 100 mechanically ventilated patients undergoing bronchoscopy with bronchial lavage. They found an overall complication rate of 10%, with hypoxemia during or immediately after the procedure being the most frequently encountered complication (9%) and with only one bronchoscopy being terminated early (20).
The strengths of our study are in the use of the largest cohort in literature for examining the effects of bronchoscopy for the sole indication of atelectasis and on clinical relevant outcomes, as well as the long term follow-up, for up to 24 h post intervention. Furthermore, this is the first study to investigate predictors for the clinical improvement of gas exchange.
There are a number of limitations to this study, the most important being its observational retrospective design and inherent bias, resulting in an inability to control for confounders. No data is available on pulmonary recruitment before or after the procedure. This decision was left to the clinical judgment of the attending intensive care physician. Also, the true incidence of adverse events may be underestimated in a retrospective study. Furthermore, a suboptimal calculation was used to calculate Pdriving. Missing data at one point of time after intervention is also a limitation in our study. By dismissing the incomplete case series, the inclusion of cases for nonparametric testing ranged between 57 and 85%.
Current evidence on this topic has been dominated by observational studies that investigate the short-term effects of bronchoscopy. Although our results suggest clinical improvement of gas exchange and pulmonary mechanics, future research should confirm our results in a prospective manner, preferably by a randomized controlled study. Subsequently research should focus on patient outcomes such as length of stay and ventilator-free days.
Conclusion
In conclusion, bronchoscopy for atelectasis is beneficial in most ICU patients by improving gas exchange and mechanical properties of the respiratory system, with positive effects lasting for up to 24 h. In addition, bronchoscopy is safe in these patients.
Availability of Research Data
Permission to publish the datasets supporting the conclusions of this article was not granted by our institution. Requests to access the datasets should be directed to the corresponding author (ay5zbWVpanN0ZXJzQHZ1bWMubmw=).
Ethics Approval and Consent to Participate
The research project was reviewed and approved by the medical ethics board at VUmc (reference 2017.084); informed consent was waived and de-identified patient data was used.
Author Contributions
KS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects, and was also responsible for manuscript preparation and revision. RB was involved in study design and data collection and revised the manuscript for important intellectual content. JD, AG, and LH were involved in study design and revised the manuscript for important intellectual content. PvdV was responsible for statistical analysis and manuscript revision. JS and PT supervised the project and were involved in all aspects of the study. All authors read and approved the final version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
ICU, Intensive care Unit; CXR, Chest X- ray; Art-etCO2, arterial pCO2 end tidal CO2 difference; EtCO2, end tidal measurement of CO2; PaCO2, partial pressure of CO2 in arterial blood; PaO2/FiO2 ratio, the ratio of arterial oxygen partial pressure to fractional inspired oxygen; PEEP, positive end expiratory pressure; Pdriving, driving pressure (Ppeak-PEEP); Ppeak, peak pressure.
References
1. Jaffal K, Six S, Zerimech F, Nseir S. Relationship between hyperoxemia and ventilator associated pneumonia. Ann Transl Med. (2017) 5:453. doi: 10.21037/atm.2017.10.15
2. Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. (2013) 369:2126–36. doi: 10.1056/NEJMra1208707
3. Kreider ME, Lipson DA. Bronchoscopy for atelectasis in the ICU: a case report and review of the literature. Chest (2003) 124:344–50. doi: 10.1378/chest.124.1.344
4. Marini JJ, Pierson DJ, Hudson LD. Acute lobar atelectasis: a prospective comparison of fiberoptic bronchoscopy and respiratory therapy. Am Rev Respir Dis. (1979) 119:971–8.
5. Lindholm CE, Ollman B, Snyder J, Millen E, Grenvik A. Flexible fiberoptic bronchoscopy in critical care medicine. Diagnosis, therapy and complications. Crit Care Med. (1974) 2:250–61. doi: 10.1097/00003246-197409000-00004
6. Mahajan VK, Catron PW, Huber GL. The value of fiberoptic bronchoscopy in the management of pulmonary collapse. Chest (1978) 73:817–20. doi: 10.1378/chest.73.6.817
7. Olopade CO, Prakash UB. Bronchoscopy in the critical-care unit. Mayo Clin Proc. (1989) 64:1255–63.
9. Stevens RP, Lillington GA, Parsons GH. Fiberoptic bronchoscopy in the intensive care unit. Heart Lung. (1981) 10:1037–45.
10. Turner JS, Willcox PA, Hayhurst MD, Potgieter PD. Fiberoptic bronchoscopy in the intensive care unit–a prospective study of 147 procedures in 107 patients. Crit Care Med. (1994) 22:259–64. doi: 10.1097/00003246-199402000-00017
11. Weinstein HJ, Bone RC, Ruth WE. Pulmonary lavage in patients treated with mechanical ventilation. Chest (1977) 72:583–7. doi: 10.1378/chest.72.5.583
12. Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. (2001) 345:568–73. doi: 10.1056/NEJMoa010043
13. Lee DL, Chiang HT, Lin SL, Ger LP, Kun MH, Huang YC. Prone-position ventilation induces sustained improvement in oxygenation in patients with acute respiratory distress syndrome who have a large shunt. Crit Care Med. (2002) 30:1446–52. doi: 10.1097/00003246-200207000-00008
14. Charron C, Repesse X, Bouferrache K, Bodson L, Castro S, Page B, et al. PaCO2 and alveolar dead space are more relevant than PaO2/FiO2 ratio in monitoring the respiratory response to prone position in ARDS patients: a physiological study. Crit Care (2011) 15:R175. doi: 10.1186/cc10324
15. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. (1985) 13:818–29. doi: 10.1097/00003246-198510000-00009
16. Jolliet P, Chevrolet JC. Bronchoscopy in the intensive care unit. Intensive Care Med. (1992) 18:160–9. doi: 10.1007/BF01709240
17. Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. (2015) 372:747–55. doi: 10.1056/NEJMsa1410639
18. Lindgren S, Odenstedt H, Erlandsson K, Grivans C, Lundin S, Stenqvist O. Bronchoscopic suctioning may cause lung collapse: a lung model and clinical evaluation. Acta Anaesthesiol Scand. (2008) 52:209–18. doi: 10.1111/j.1399-6576.2007.01499.x
19. Estella A. [Analysis of 208 flexible bronchoscopies performed in an intensive care unit]. Med Intensiva (2012) 36:396–401. doi: 10.1016/j.medine.2012.08.001
Keywords: bronchoscopy, atelectasis, intensive care, critical care, gas exchange, respiratory mechanics
Citation: Smeijsters KMG, Bijkerk RM, Daniels JMA, van de Ven PM, Girbes ARJ, Heunks LMA, Spijkstra JJ and Tuinman PR (2018) Effect of Bronchoscopy on Gas Exchange and Respiratory Mechanics in Critically Ill Patients With Atelectasis: An Observational Cohort Study. Front. Med. 5:301. doi: 10.3389/fmed.2018.00301
Received: 26 June 2018; Accepted: 11 October 2018;
Published: 13 November 2018.
Edited by:
Mikhail Kirov, Northern State Medical University, RussiaReviewed by:
Lars Jakob Bjertnæs, UiT The Arctic University of Norway, NorwayEvgeny Suborov, North-Western State Medical University named after II. Mechnikov, Russia
Copyright © 2018 Smeijsters, Bijkerk, Daniels, van de Ven, Girbes, Heunks, Spijkstra and Tuinman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kim M. G. Smeijsters, ay5zbWVpanN0ZXJzQHZ1bWMubmw=
 Kim M. G. Smeijsters
Kim M. G. Smeijsters Ronald M. Bijkerk
Ronald M. Bijkerk Johannes M. A. Daniels4
Johannes M. A. Daniels4 Jan Jaap Spijkstra
Jan Jaap Spijkstra Pieter R. Tuinman
Pieter R. Tuinman