- 1Department of Obstetrics and Gynecology, Cantonal Hospital of Lucerne, Lucerne, Switzerland
- 2Department of Radiology, Cantonal Hospital of Lucerne, Lucerne, Switzerland
Introduction: Surgical treatment in oncology is one of the main part concerning the surveillance rate of the patient in case of tumor recurrence. Metastatic suspected lesions are mostly located in the abdomen or pelvis and are diagnosed by PET, MRI, or CT scan. Especially surgery of small lesions in recurrent disease for diagnostic or therapeutic purpose is often challenging.
Material and Methods: We report a case series of 3 patients who were treated in our department due to a metastatic suspected lesion in PET-CT in follow up. For histological confirmation we performed a laparoscopy using a near infrared camera (NIR) for an improved visualization of the metastatic suspected lesion during surgical treatment. Previously the lesion was marked with an amount of Indocyanine Green (ICG) via computer tomography-guided percutaneous injection. The lesion was identified via NIR camera. While changing the camera in NIR mode, it show up as a blue spot due to the fluorescent signal. After correct identification it was removed and send to pathology.
Results: In all 3 cases they confirmed the diagnosis of a metastatic lesion. Complication occur in just one case, where the metastatic lymph node infiltrated the external iliac vein, which led to a high blood loss. In this case a vascular interposition had to be done.
Conclusions: Because of separate wavelengths, which are used for illumination and recording, only the marked area is visible, not the background.Due to correct identification, resection of the lesion was improved and healthy surrounding tissue could have been spared.
Problem
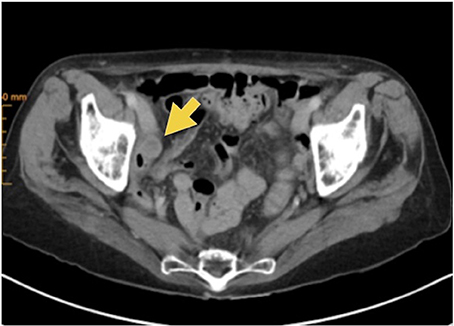
Metastatic suspected lesions are mostly located in the abdomen or pelvis and are diagnosed by PET, MRI or CT scan (Figure 1). Especially surgery of small lesions in recurrent disease for diagnostic or therapeutic purpose is often a challenge, caused by 2 problems. First, detection of the suspected lesion is very difficult due to altered anatomy and adhesions caused by the operation or radiation. Second, intraoperative findings often do not correlate with imaging findings, in particular very small lesions. To detect a suspected lesion correctly while surgical treatment, an injection of a fluorescent dye, like ICG is possible. This attractive method to facilitate the visualization of lymphatic vessels, sentinel nodes, and metastatic lymph nodes has been introduced by Lim and Soter (1).
As a tracer Indocyanine Green is mostly used for SLN mapping in Cervical and Endometrial Cancer and showed increased detection rates compared to the Conventional Dyes (blue dye, 99Tc, or combination of the two tracers) (2, 3). Because of separate wavelengths, which are used for illumination and recording, only the marked area is visible, not the background. Extremely small concentrations are needed to make the marked area visible (4, 5).
Our Solution
In our department we treated three patients due to metastatic suspected lesion in the abdomen/pelvis caused by cervical cancer (2) and carcinosarcoma (1). The first patient was a 35-year old women with a metastatic suspected lesion 2 years after cervical cancer. Initial surgical treatment on FIGO IIA was performed as Total Mesometrial Resection with sentinel lymph node biopsy and was followed by radiation and chemotherapy. The lesion was located on peritoneal site paracolic left. It was resected without difficulties after mobilization of the colon descendens. In this case an expander was inserted to protect the colon in radiotherapy.
The second patient was a 30-year old women with metastatic suspected lesion near external iliac vein 2 years after cervical cancer. Initial surgical treatment on FIGO IB1 was performed as extended cervical conization with sentinel lymph node biopsy, pelvic lymphadenectomy right and paraaortic lymphadenectomy and was followed by radiation and chemotherapy. The lesion was marked on the left side without complication. Due to infiltration of the external iliac vein a severe bleeding was caused by trying to dissect the lesion. Therefore a laparotomy had been performed to stop bleeding. Patientin three, a 74-year old women, had a suspected lesion near external iliac vein 2 years after carcinoasarcoma. Initial operation was performed on FIGO IA by hysterectomy, adnexectomy, pelvic and paraaortic lymphadenectomy and omentectomy. No radiation or chemotherapy has been followed. In this case we performed a prophylactic clamping of the external iliac vein to avoid a mayor complication. The vein was blocked with bulldog-clamps. The operation was performed laparoscopically without any complications. This case is demonstrated in the video.
No ICG was used prior to mark the lymphnodes. Therefore we used ICG to mark the metastatic suspected lesion computer tomography guided in all three cases.
One vial of 25 mg ICG powder was suspended with 5 ml of sterile water to get a maximum of concentration. We tried to insufflate as less as possible due to little capacity of the lymph node. After running a conventional CT with contrast agent first to demonstrate the lesion, 0.2–0.3 ml of ICG was injected into the lesion via 20-Gauge needle computer tomography guided (Figure 2). The patient was directly transferred to the operating room. The operation started 30 min after injection.
We performed a conventional laparoscopy with a NIR camera. In all three cases the suspected lesion show up as a blue spot (Figures 3, 4). The diagnosis of a metastatic lesion was confirmed by pathology in all three patients.
Complication occur in just one case, where the metastatic lymph node infiltrated the external iliac vein, which led to a high blood loss. In this case a vascular interposition had to be done.
Discussion
In our video we are explaining how it is possible to detect small lesions laparoscopically after preoperative computer tomography guided Indocyanine Green injection. In a case series of 3 patients we were able to demonstrate an effective method of correct excision. Especially in the age of modern hybrid operating theaters, which are not yet in routine use in gynecology, a preoperative computer tomography guided injection with a fluorescent dye is a possible method which may lead to shorter operation times and less trauma by correct identification of the suspect lesion. Despite the fact that we do know the limitation of our case series, we truly believe that this cases could pave the way for the establishment of a new operation procedure.
Ethics Statement
All subjects involved in this case series gave written informed consent in accordance with the Decleration of Helsinki.
Author Contributions
AK and AG conception or design of the work and drafting the article. AK, GM, RL, and JF data collection. AK, GM, and AG data analysis and interpretation. AK, RL, JF, GM, and AG critical revision of the article. AK, RL, JF, GM, and AG final approval of the version to be published.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/.2018.00191/full#supplementary-material
References
2. Buda A, Papadia A, Zapardiel I, Vizza E, Ghezzi F, De Ponti E. From Conventional Radiotracer Tc-99(m) with Blue Dye to Indocyanine Green Fluorescence: A Comparison of Methods Towards Optimization of Sentinel Lymph Node Mapping in Early Stage Cervical Cancer for a Laparoscopic Approach. Ann Surg Oncol (2016) 23:2959–65. doi: 10.1245/s10434-016-5227-y.
3. Ruscito I, Gasparri ML, Braicu EI, Bellati F, Raio L, Sehouli J. Sentinel Node Mapping in Cervical and Endometrial Cancer: Indocyanine Green Versus Other Conventional Dyes-A Meta-Analysis. Ann Surg Oncol. (2016) 23:3749–56. doi: 10.1245/s10434-016-5236-x
4. Alander JT, Kaartinen I, Laakso A, Pätilä T, Spillmann T, Tuchin VV, et al. A review of indocyanine green fluorescent imaging in surgery. Int J Biomed Imaging (2012) 2012:940585. doi: 10.1155/2012/940585
Keywords: Indocyanine Green, ICG, mapping metastatic suspected lesions, gynecological metastatic suspected lesions, gynecological oncology
Citation: Kreklau A, Lopez Benitez R, Fornaro J, Meili G and Günthert A (2018) Computer Tomography-Guided Percutaneous Indocyanine Green Injection for Intraoperative Mapping of Metastatic Suspected Lesions. Front. Med. 5:191. doi: 10.3389/fmed.2018.00191
Received: 12 February 2018; Accepted: 08 June 2018;
Published: 10 July 2018.
Edited by:
Patrice Mathevet, Centre Hospitalier Universitaire Vaudois (CHUV), SwitzerlandReviewed by:
Salim Alfred Bassil, Al Arz Hospital, LebanonVincent Balaya, Hôpital Européen Georges-Pompidou, France
Copyright © 2018 Kreklau, Lopez Benitez, Fornaro, Meili and Günthert. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anne Kreklau, YW5uZS5rcmVrbGF1QGx1a3MuY2g=
 Anne Kreklau
Anne Kreklau Ruben Lopez Benitez2
Ruben Lopez Benitez2