
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Immunol. , 15 October 2020
Sec. Autoimmune and Autoinflammatory Disorders
Volume 11 - 2020 | https://doi.org/10.3389/fimmu.2020.584241
 Maria Orietta Borghi1,2
Maria Orietta Borghi1,2 Asmaa Beltagy1,3
Asmaa Beltagy1,3 Emirena Garrafa4,5
Emirena Garrafa4,5 Daniele Curreli1
Daniele Curreli1 Germana Cecchini6
Germana Cecchini6 Caterina Bodio1
Caterina Bodio1 Claudia Grossi1
Claudia Grossi1 Simonetta Blengino7
Simonetta Blengino7 Angela Tincani8
Angela Tincani8 Franco Franceschini8
Franco Franceschini8 Laura Andreoli8
Laura Andreoli8 Maria Grazia Lazzaroni8
Maria Grazia Lazzaroni8 Silvia Piantoni8
Silvia Piantoni8 Stefania Masneri8
Stefania Masneri8 Francesca Crisafulli8
Francesca Crisafulli8 Duilio Brugnoni5
Duilio Brugnoni5 Maria Lorenza Muiesan9
Maria Lorenza Muiesan9 Massimo Salvetti9
Massimo Salvetti9 Gianfranco Parati7
Gianfranco Parati7 Erminio Torresani6
Erminio Torresani6 Michael Mahler10
Michael Mahler10 Francesca Heilbron7
Francesca Heilbron7 Francesca Pregnolato1
Francesca Pregnolato1 Martino Pengo7
Martino Pengo7 Francesco Tedesco1
Francesco Tedesco1 Nicola Pozzi11*
Nicola Pozzi11* Pier Luigi Meroni1*
Pier Luigi Meroni1*Background: Critically ill patients with coronavirus disease 2019 (COVID-19) have a profound hypercoagulable state and often develop coagulopathy which leads to organ failure and death. Because of a prolonged activated partial-thromboplastin time (aPTT), a relationship with anti-phospholipid antibodies (aPLs) has been proposed, but results are controversial. Functional assays for aPL (i.e., lupus anticoagulant) can be influenced by concomitant anticoagulation and/or high levels of C reactive protein. The presence of anti-cardiolipin (aCL), anti-beta2-glycoprotein I (anti-β2GPI), and anti-phosphatidylserine/prothrombin (aPS/PT) antibodies was not investigated systematically. Epitope specificity of anti-β2GPI antibodies was not reported.
Objective: To evaluate the prevalence and the clinical association of aPL in a large cohort of COVID-19 patients, and to characterize the epitope specificity of anti-β2GPI antibodies.
Methods: ELISA and chemiluminescence assays were used to test 122 sera of patients suffering from severe COVID-19. Of them, 16 displayed major thrombotic events.
Results: Anti-β2GPI IgG/IgA/IgM was the most frequent in 15.6/6.6/9.0% of patients, while aCL IgG/IgM was detected in 5.7/6.6% by ELISA. Comparable values were found by chemiluminescence. aPS/PT IgG/IgM were detectable in 2.5 and 9.8% by ELISA. No association between thrombosis and aPL was found. Reactivity against domain 1 and 4-5 of β2GPI was limited to 3/58 (5.2%) tested sera for each domain and did not correlate with aCL/anti-β2GPI nor with thrombosis.
Conclusions: aPL show a low prevalence in COVID-19 patients and are not associated with major thrombotic events. aPL in COVID-19 patients are mainly directed against β2GPI but display an epitope specificity different from antibodies in antiphospholipid syndrome.
Critically ill patients with coronavirus disease 2019 (COVID-19) have a profound hypercoagulable state and often develop thrombosis in veins, arteries and in the microcirculation (1, 2). A recent analysis showed several coagulation abnormalities in these patients, including prominent elevation of fibrin/fibrinogen degradation products (i.e., D-dimer) and a prolonged activated partial-thromboplastin time (aPTT). While high levels of D-dimer are consistent with sustained activation of the clotting and fibrinolytic cascades, the combination of prolonged aPTT and both arterial and venous thrombosis was, however, surprising, and it is reminiscent of a clinical scenario known as antiphospholipid syndrome (APS) (3).
Looking at the causes of aPTT prolongation, recent studies have shown that lupus anticoagulant (LA) can be detected in a significant percentage of COVID-19 samples (4–6). Since LA is often caused by anti-phospholipid antibody (aPL), these findings support the idea that aPL may play a role in COVID-19 (7). However, it is important to point out that LA is a very sensitive assay and its outcome can be influenced by several factors, most notably heparin administration (8) and a profound inflammatory state characterized by high levels of C reactive protein (CRP) (9, 10). Both of them are present in COVID-19 patients (11).
Another method to detect aPL that is in principle insensitive to anticoagulation and other confounding agents relies on the detection and quantification of autoantibodies using solid-phase assays (3). Using this method, the presence of aPL was recently reported in a handful of case reports and small cohorts of patients (4, 6, 7, 12, 13). While encouraging, this data is limited and its interpretation remains controversial, with some investigators proposing an important role of aPL in COVID-19 patients (7) while others suggesting a very poor correlation between aPL and thrombotic events (14). There is no information on the antigen specificity of COVID-19 aPL in comparison with APS antibodies. Such information and a larger study, possibly multicenter, may be instrumental to clarify the real clinical value of these autoantibodies.
A total of 122 patients were enrolled from two COVID-19 referral centers in Lombardia. All patients tested positive to SARS-CoV-2, and classified as severe or critical COVID-19 (11). The mean age was 68.5 (± SD 16.4) years; 77 were men and 45 women. No diagnosis of previous autoimmune diseases was made; six patients had a thrombotic event (three arterial and three venous) in the past clinical history. The presence of antinuclear antibodies (ANAs) was investigated in 58 patients at Istituto Auxologico Italiano by HEp2-IIF and solid phase CTD screening following the guidelines described in Agmon-Levin et al. (15). Of the 58 samples, none was positive for ANA.
Eighty-seven patients suffering from APS were also tested for anti-cardiolipin (aCL) and anti-β2GPI IgG/IgM (16).The study was approved by the Ethics Committees (Istituto Auxologico Italiano 3-04-2020 - Milan and ASST Spedali Civili NP4187 - Brescia).
aCL and anti-β2GPI IgG/IgA/IgM were detected by chemiluminescence immunoassay (CIA; Quanta Flash, Inova, San Diego, CA, US) and a home-made ELISA as described (16, 17). Anti-β2GPI domain 1 IgG (anti-D1) were detected by CIA (16, 17), IgG anti-D4-5 by a home-made ELISA, as described (16, 17). Detailed methods are reported in the Supplementary Material. Anti-phosphatidylserine/prothrombin (aPS/PT) IgG/IgM were detected by a commercial ELISA as reported (18). Blood samples were collected in the first week after hospital admission.
Data were analyzed using R v3.4.0. Descriptive statistics was used to summarize data. Associations and differences between categorical or continuous variables were tested by Fisher’s exact test and non-parametric Mann-Whitney test, respectively. A p-value < 0.05 was considered statistically significant.
Table 1 reports the median with minimum and maximum values for different coagulation and inflammation parameters in 122 severe or critical COVID-19 patients. In particular, prolonged aPTT (>30 s) was found in 57.6% while PT INR values were above the cut-off in 24.8% of the cases. Most of the patients (120/122) were on anticoagulation with low molecular weight heparin (70% on therapeutic and the remaining on prophylactic dosage). Despite anticoagulation, we observed sixteen thrombotic events (13.1%, 8 in veins and 8 in arteries). These statistics are in agreement with previous reports (2, 19–24) and document a systemic inflammation and a coagulopathy in our patients.
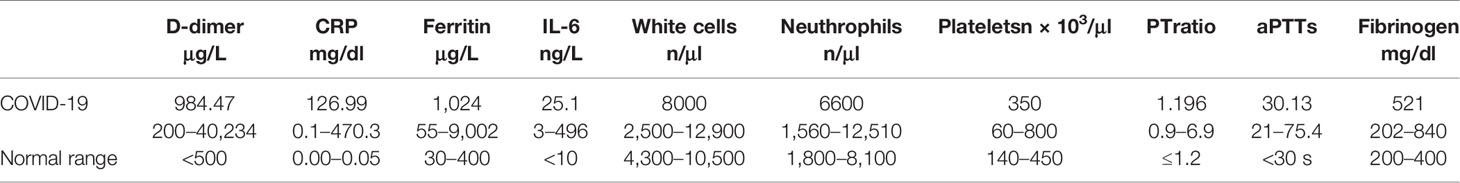
Table 1 Coagulation and inflammation parameters expressed as median with minimum and maximum in severe or critical COVID-19 patients.
In the APS field, testing for LA is not recommended when patients are on heparin, since the presence of heparin, even if neutralized, may lead to false-positive results (8). Likewise, high levels CRP, such as those found in our cohort of patients, have been shown to prolong aPTT independently from the presence of aPL (9, 10). On these bases, the presence of aPL was researched using solid-phase assays, and not LA. First, we investigated the presence of aCL and anti-β2GPI, two APS classification criteria (3). Testing was independently performed in Milan and Brescia, using harmonized methodologies (25). The prevalence of COVID-19 patients positive for aCL and anti-β2GPI IgG/IgA/IgM detected by ELISA and CIA is summarized in Table 2. The ELISA raw data are shown in Figure 1. We found IgG/IgM aCL in 5.7/6.6% of patients, whereas anti-β2GPI IgG/IgA/IgM were found in 15.6/6.6/9.0% of patients. Similar values were obtained for aCL antibodies using CIA (Table 2), whereas a slightly lower sensitivity was obtained for anti-β2GPI antibodies (26). The positivity for aCL and anti-β2GPI antibodies was at medium/low titer in contrast with the medium/high titers found in the control group of primary APS (Figure 1). There is no association between aPL positivity and thrombotic events.
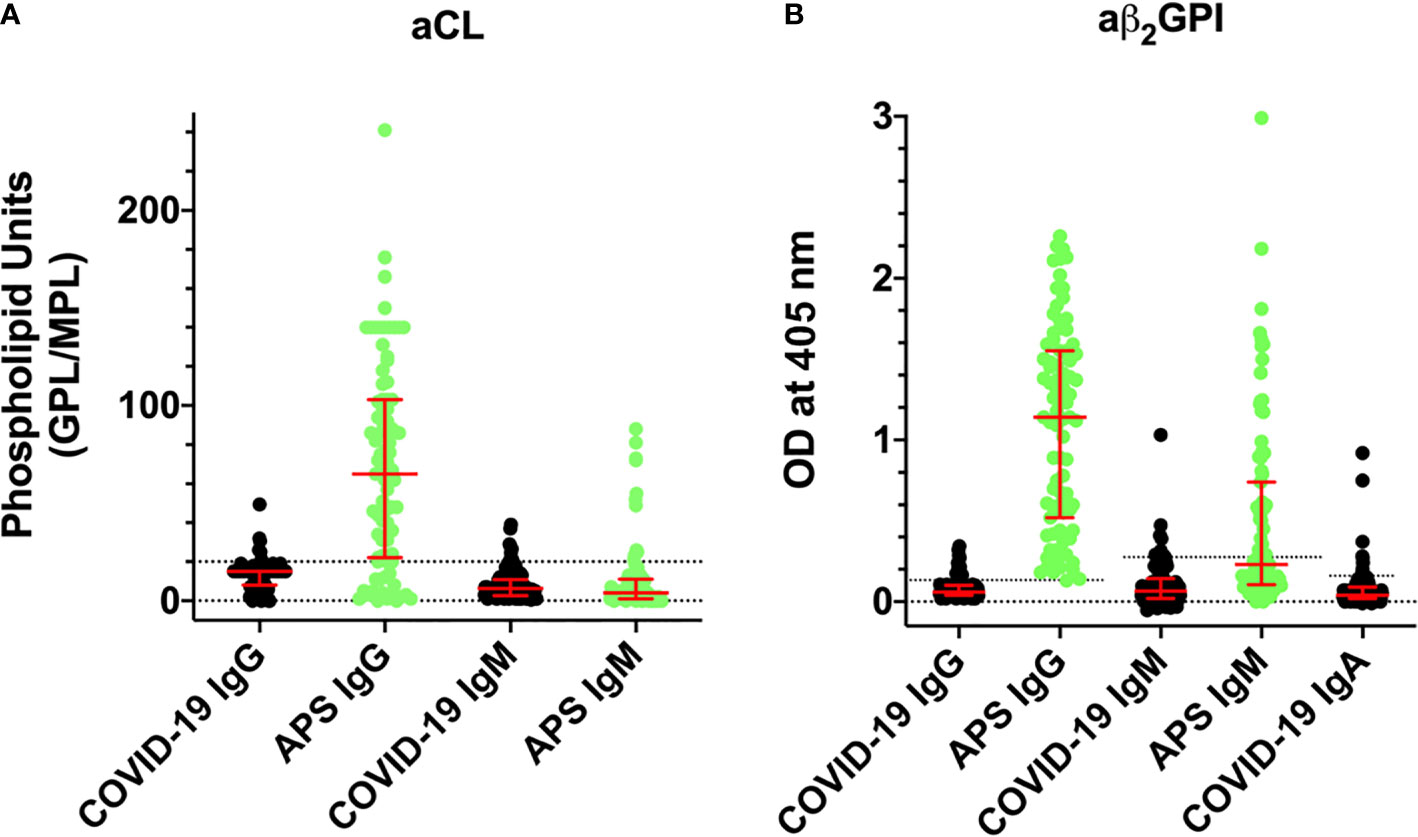
Figure 1 Titers of aCL and aβ2GPI antibodies detected by ELISA in COVID-19 patients (black, n = 122) and comparison with APS patients (green, n = 86). Values are expressed as median levels [first and third quartile]. (A) aCL. From the left to the right: COVID-19 IgG: 15 [8–15]; APS IgG: 65 [22–103]; COVID-19 IgM: 6.2 [2.6–10.8]; and APS IgM: 4.0 [1–11]. (B) aβ2GPI. From the left to the right: COVID-19 IgG: 0.06 [0.04–0.10]; APS IgG: 1.14 [0.52–1.55]; COVID-19 IgM: 0.065 [0.02–0.142]; APS IgM: 0.23 [0.105–0.741]; and COVID-19 IgA: 0.04 [0.02–0.09]. Cutoff values are aCL IgG/IgM 20 phospholipid units (GPL/MPL); aβ2GPI IgG/IgM/IgA ELISA 0.13, 0.27, and 0.16 optical units (OD), respectively.
Fifty-eight sera were also tested with D1 and D4-5-coated plates in order to characterize their epitope specificity. Figure 2B shows that three out of 58 samples reacted with D1, while in Figure 2C, three samples tested positive for D4-5. None of the sera was positive for both domains and all displayed a weak reactivity with no association with thrombosis.
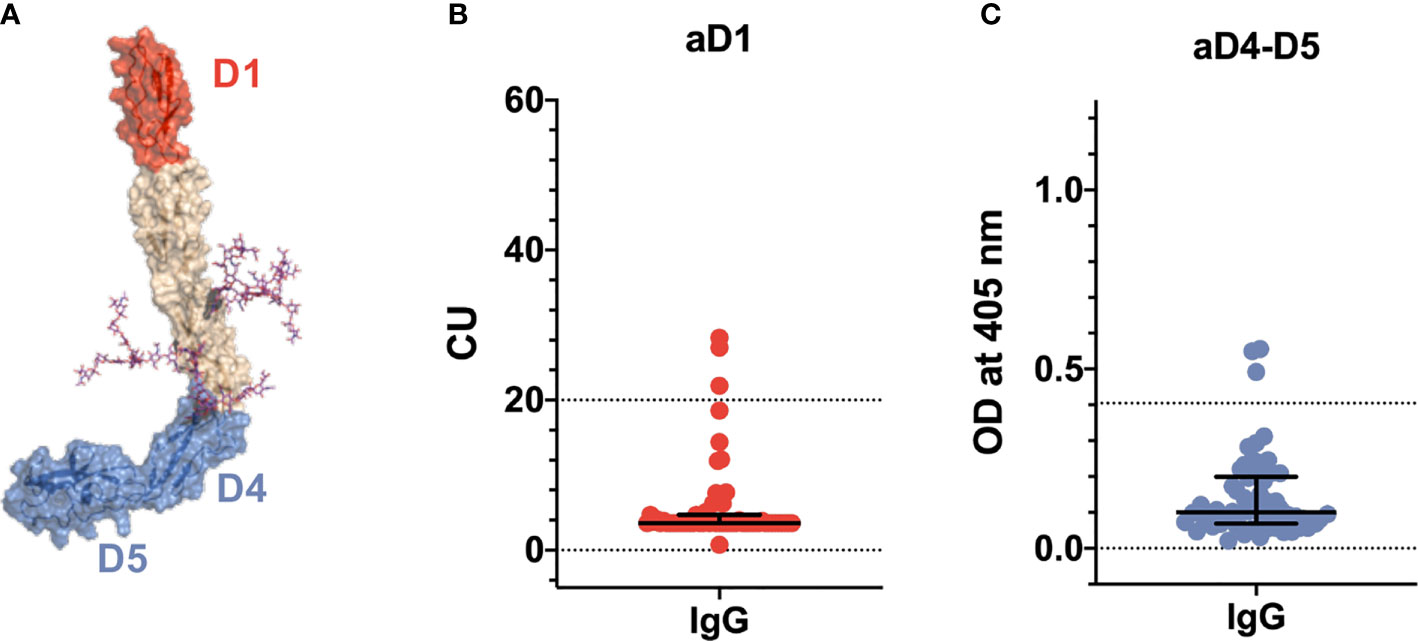
Figure 2 Epitope specificity of anti-β2GPI antibodies in COVID-19 patients. (A) Three-dimensional structure of β2GPI solved at 2.4 Å by X-ray crystallography [PDI ID: 6V06 (27)] displaying the positioning of the fragments used in this study. The N-terminal D1 is shown in red. The C-terminal D4-5 fragment is shown in blue. N-linked glycosylations are shown as magenta stick. Titers of anti-D1 (B) and anti-D4-5 antibodies (C) in 58 COVID-19 patients detected by chemiluminescence and ELISA, respectively. Values are expressed as median levels [first and third quartile]. Anti-D1(aD1): 3.6 [3.6–4.7]. Anti-D4-D5 (aD4-D5): 0.10 [0.068–0.199]. Cutoff values are >20 chemiluminescent units (CU) and >0.405 optical units (OD) for aD1 and aD4-D5, respectively.
Prolonged aPTT (>30 s) was found in 57.6% of the patients. Although aPS/PT are not included in the APS classification laboratory tests, they can be associated with a prolonged aPTT and with the presence of LA (18). Consequently, we looked at the presence of aPS/PT antibodies in our cohort and we found fifteen out of 122 sera positive for aPS/PT (12.3%), mostly of the IgM isotype (12 out 15) and at a low titer (Figure 3). There was no association between prolonged aPTT and the presence of aPS/PT antibodies nor with thrombotic events in our COVID-19 cohort.
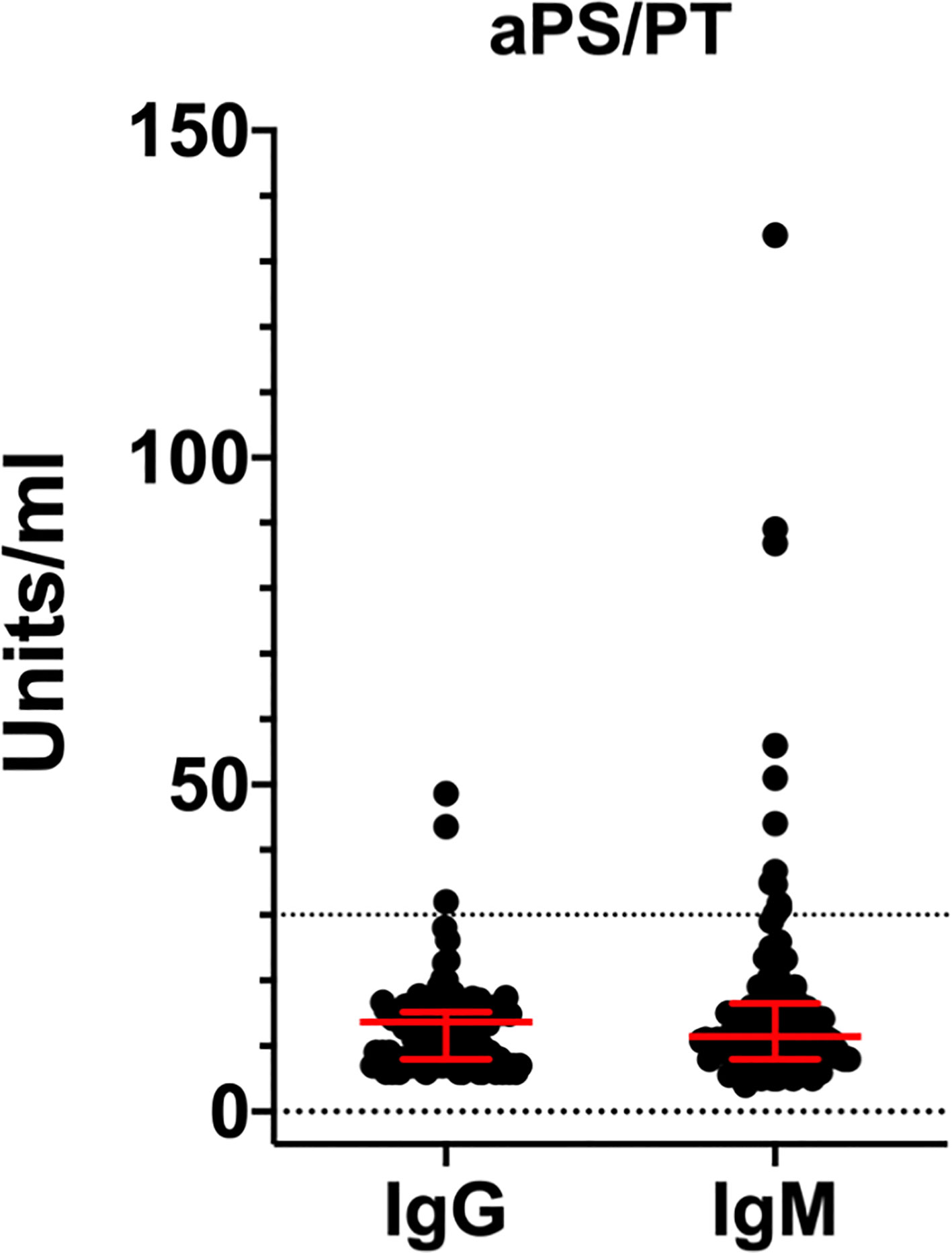
Figure 3 Titers of aPS/PT antibodies detected by ELISA in COVID-19 patients. Values are expressed as median levels [first and third quartile]. aPS/PT IgG:13.6 [8 to 15.2]; aPS/PT IgM:11.4 [8 to 16.5] IgM. Cut-off of the assays was 30 units/ml.
Taken together, our data show a low prevalence of classification criteria aPL in COVID-19 patients. In this regard, our study confirms recent studies obtained with smaller cohorts of patients (4, 14, 24). Importantly, our data also shows that aPL are slightly more reactive towards β2GPI-coated plates as compared to CL-coated ones and that, regardless of the nature of aPL, there is no association between aPL positivity and thrombotic events (p = 1).
A striking difference between the autoantibody profile in COVID-19 patients as compared to the one in APS concerned the titers of aPL. Medium/low aPL titers were consistently found in patients with COVID-19. By contrast, medium/high titers are usually found in APS patients (Figure 1). This difference suggests that aPL found in COVID-19 may be different from aPL found in APS and led us to further investigate the epitope specificity of anti-β2GPI antibodies. We focused on autoantibodies directed against the N-terminal domain 1 (anti-D1) or the C-terminal domains 4-5 (anti-D4-5) of the molecule (17) (Figure 2A). This is because anti-D1 antibodies are associated with an increased risk of thrombosis and pregnancy complications in APS (16, 17, 28). By contrast, anti D4-5 antibodies are associated neither with vascular nor obstetric APS manifestations (16, 29). Furthermore, anti D4-5 antibodies are also reported at high levels in the so called asymptomatic aPL carriers and are frequently found in non-APS (e.g., patients with leprosy, atopic dermatitis, atherosclerosis, and in children born to mothers with systemic autoimmune diseases) (29). We found that three out of 58 samples reacted with D1, and three samples tested positive for D4-5. None of the sera was positive for both domains and all displayed a weak reactivity. Although the number of the investigated sera is relatively small, this finding is quite different from the results found in APS in which almost all the sera positive for the whole β2GPI molecule also reacted with domain D1 at high titer (16, 28). Furthermore, at variance with APS patients, none of the anti-D1 positive patients displayed thrombotic events (28).
Approximately, 57% of COVID-19 patients have prolonged aPTT. Yet, only a small proportion of COVID-19 patients carry aCL and anti-β2GPI antibodies. This suggests that other factors must be responsible for the prolonged aPTT phenomenon and likely for the LA activity. LA may be affected by the concomitant heparin treatment and the high CRP levels. Although more sensitive and specific diagnostic algorithms have been suggested (30), we followed the ISTH guidelines available at the beginning of the study (31). Since aPS/PT can be associated with a prolonged aPTT and with the presence of LA (18), we tested our cohort for aPS/PT antibodies. We found a small percentage (12.3%) of positive sera, mostly of the IgM isotype (12 out 15) and at a low titer. Again, there was no association between prolonged aPTT and the presence of aPS/PT antibodies nor with thrombotic events in our COVID-19 cohort. This indicates that aPS/PT are not responsible for the prolongation of aPTT nor are predictors of adverse clinical outcomes. Furthermore, in contrast to what we would have expected in APS (32), we found no associations between the presence of aPS/PT, aCL, and anti-β2GPI antibodies. This data is in line with the unusual epitope specificity of anti-β2GPI antibodies documented in Figure 2, supporting the hypothesis that aPL found in COVID-19 patients are different from aPL found in APS patients. Whether COVID-19 aPL are similar to the ones found in other infectious diseases such as HCV, HBV and HIV (33) remains to be determined.
Despite heparin treatment, 13.1% of our patients displayed thrombotic events. Although we cannot exclude that treatment could be protective, the prevalence of vascular events was in line with that reported by other studies as recently reviewed (34).
In conclusion, while the medium/high aPL titers with D1 specificity are associated with vascular events in APS, low antibody titers with reactivity against β2GPI epitope(s) different from D1 or D4,5 can be found in COVID-19. This may explain the lack of association with thrombotic events in COVID-19. In addition, our data do not support the hypothesis that aPL can be the main cause of prolonged aPTT in these patients. Although low titer aPL are not predictive of vascular events in the APS, it is important to keep in mind that COVID-19 patients suffer from an acute form of systemic inflammation with complement activation (35), which may be responsible for endothelial perturbation. In this context, since β2GPI can accumulate on the activated endothelium at high density, even low titers of aPL may become pathogenic thus potentiating or even triggering thrombus formation, especially when anticoagulation is suspended. A comparable condition in which low titers of aPL can cause substantial damage is seen in obstetric APS, where high levels of β2GPI can be found in the placenta (36). Hence, while transitory aPL are likely to be clinically irrelevant in COVID-19 patients as in other infections (33), detection of aPL may be useful for identifying patients potentially at risk of thrombosis after the hospital discharge. Accordingly, anticoagulant prophylaxis or therapies affecting cell signaling involved in inflammatory and coagulation responses could be justified before a confirmatory assay (3, 37).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Istituto Auxologico Italiano 3-04-2020 - Milan and ASST Spedali Civili NP4187 - Brescia. The ethics committee waived the requirement of written informed consent for participation.
MB, MP, AT, FF, FT, NP, and PM designed the study. SB, GP, FH, MP, ML, MLM, and MS collected clinical samples. EG, DC, GC, CB, CG, SP, SM, FC, DB, ET, MM, and LA performed research. MB, AB, FP, FT, NP, and PM analyzed data. MB, FT, NP, and PM wrote the manuscript. All authors contributed to the article and approved the submitted version.
The study was in part supported by IRCCS Istituto Auxologico Italiano - Ricerca Corrente 2019 (PM), a grant from the Italian Ministry of Foreign Affairs and International Cooperation (MAECI) for foreign citizens and Italian citizens living abroad (AB) and a National Institutes of Health Research Grant HL150146 (NP).
MM was employed by Inova Diagnostics, Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank N. Carabellese and G. Martini (Department of Laboratory Diagnostics; ASST Spedali Civili, Brescia, Italy) for their valuable collaboration; all the physicians of the COVID-19 Units of the IRCCS Istituto Auxologico Italiano (Milan) and the ASST Spedali Civili (Brescia). This article has been released as a pre-print at [medRxiv. 2020 Jun 19:2020.06.17.20134114. doi: 10.1101/2020.06.17.20134114. Preprint.], [Borghi M.O., Beltagy A., Garrafa E., Curreli D., Cecchini G., Bodio C., et al.] (38).
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2020.584241/full#supplementary-material
1. Carsana L, Sonzogni A, Nasr A, Rossi RS, Pellegrinelli A, Zerbi P, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis (2020) 20:1135–40. doi: 10.1016/S1473-3099(20)30434-5
2. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost (2020) 18:844–7. doi: 10.1111/jth.14768
3. Garcia D, Erkan D. Diagnosis and Management of the Antiphospholipid Syndrome. N Engl J Med (2018) 378:2010–21. doi: 10.1056/NEJMra1705454
4. Harzallah I, Debliquis A, Drénou B. Lupus anticoagulant is frequent in patients with Covid-19. J Thromb Haemost (2020) 18:2064–5. doi: 10.1111/jth.14867
5. Bowles L, Platton S, Yartey N, Dave M, Lee K, Hart DP, et al. Lupus Anticoagulant and Abnormal Coagulation Tests in Patients with Covid-19. N Engl J Med (2020) 383:288–90. NEJMc2013656. doi: 10.1056/NEJMc2013656
6. Pineton de Chambrun M, Frere C, Miyara M, Amoura Z, Martin-Toutain I, Mathian A, et al. High Frequency of Antiphospholipid Antibodies in Critically-ill COVID-19 Patients: a Link with Hypercoagulability? J Int Med (2020) 12. doi: 10.1111/joim.13126
7. Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, et al. Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. N Engl J Med (2020) June, 382:e38. doi: 10.1056/NEJMc2007575
8. Martinuzzo ME, Barrera L.H., D ‘Adamo MA, Otaso JC, Gimenez MI, Oyhamburu J. Frequent False-positive results of lupus anticoagulant tests in plasmas of patients receiving the new oral anticoagulants and enoxaparin. Int J Lab Hematol (2014) 36:144–50. doi: 10.1111/ijlh.12138
9. Schouwers SME, Delanghe JR, Devreese KMJ. Lupus Anticoagulant (LAC) testing in patients with inflammatory status: Does C-reactive protein interfere with LAC test results? Thromb Res (2010) 125:102–4. doi: 10.1016/j.thromres.2009.09.001
10. Ruinemans-Koerts J, Ahmed-Ousenkova YM, Kaasjager HAH, Hendriks-van Wijhe C, Hovens MMC. When to screen for lupus anticoagulant? Influence of testing during acute phase and consequences for clinical practise. Lupus (2015) 24:1233–5. doi: 10.1177/0961203315583540
11. Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest (2020) 130:2620–9. doi: 10.1172/JCI137244
12. Zuo Y, Estes SK, Gandhi AA, Yalavarthi S, Ali RA, Shi H, et al. Prothrombotic antiphospholipid antibodies in COVID-19. medRxiv (2020) 17. doi: 10.1101/2020.06.15.20131607
13. Xiao M, Zhang Y, Zhang S, Qin X, Xia P, Cao W, et al. Brief Report: Anti-phospholipid antibodies in critically ill patients with Coronavirus Disease 2019 (COVID-19). Arthritis Rheumatol (2020). doi: 10.1002/art.41425
14. Galeano-Valle F, Oblitas CM, Ferreiro-Mazón MM, Alonso-Muñoz J, Del Toro-Cervera J, Di Natale M, et al. Antiphospholipid antibodies are not elevated in patients with severe COVID-19 pneumonia and venous thromboembolism. Thromb Res (2020) 192:113–5. doi: 10.1016/j.thromres.2020.05.017
15. Agmon-Levin N, Damoiseaux J, Kallenberg C, Sack U, Witte T, Herold M, et al. International recommendations for the assessment of autoantibodies to cellular antigens referred to as anti-nuclear antibodies. Ann Rheum Dis (2014) 73:17–23. doi: 10.1136/annrheumdis-2013-203863
16. Chighizola CB, Pregnolato F, Andreoli L, Bodio C, Cesana L, Comerio C, et al. Beyond thrombosis: Anti-β2GPI domain 1 antibodies identify late pregnancy morbidity in anti-phospholipid syndrome. J Autoimmun (2018) 90:76–83. doi: 10.1016/j.jaut.2018.02.002
17. Durigutto P, Grossi C, Borghi MO, Macor P, Pregnolato F, Raschi E, et al. New insight into antiphospholipid syndrome: antibodies to β2glycoprotein I-domain 5 fail to induce thrombi in rats. Haematologica (2019) 104:819–26. doi: 10.3324/haematol.2018.198119
18. Tincani A, Morozzi G, Afeltra A, Alessandri C, Allegri F, Bistoni O, et al. Antiprothrombin antibodies: a comparative analysis of homemade and commercial methods. A collaborative study by the Forum Interdisciplinare per la Ricerca nelle Malattie Autoimmuni (FIRMA). Clin Exp Rheumatol (2007) 25:268–74.
19. Nahum J, Morichau-Beauchant T, Daviaud F, Echegut P, Fichet J, Maillet JM, et al. Venous Thrombosis Among Critically Ill Patients With Coronavirus Disease 2019 (COVID-19). JAMA Network Open (2020) 3:e2010478–e. doi: 10.1001/jamanetworkopen.2020.10478
20. Zhang L, Feng X, Zhang D, Jiang C, Mei H, Wang J, et al. Deep Vein Thrombosis in Hospitalized Patients with Coronavirus Disease 2019 (COVID-19) in Wuhan, China: Prevalence, Risk Factors, and Outcome. Circulation (2020) 142:114–28. doi: 10.1161/CIRCULATIONAHA.120.046702
21. Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers D.A.M.P.J., Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res (2020) 191:145–7. doi: 10.1016/j.thromres.2020.04.013
22. Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res (2020) 191:9–14. doi: 10.1016/j.thromres.2020.04.024
23. Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller MCA, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost (2020) 18:1995–2002. doi: 10.1111/jth.14888
24. Beyrouti R, Adams ME, Benjamin L, Cohen H, Farmer SF, Goh YY, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry (2020) 91:889–91. jnnp–2020-323586. doi: 10.1136/jnnp-2020-323586
25. Andreoli L, Rizzini S, Allegri F, Meroni P, Tincani A. Are the Current Attempts at Standardization of Antiphospholipid Antibodies Still Useful? Emerging Technologies Signal a Shift in Direction. Semin Thromb Hemost (2008) 34:356–60. doi: 10.1055/s-0028-1085478
26. Lakos G, Bentow C. Mahler M. A Clinical Approach for Defining the Threshold between Low and Medium Anti-Cardiolipin Antibody Levels for QUANTA Flash Assays. Antibodies (Basel Switzerland) (2016) 5:14. doi: 10.3390/antib5020014
27. Ruben EA, Planer W, Chinnaraj M, Chen Z, Zuo X, Pengo V, et al. The J-elongated conformation of beta2-glycoprotein I predominates in solution: Implications for our understanding of antiphospholipid syndrome. J Biol Chem (2020) 295:10794–806, jbc.RA120.013939. doi: 10.1074/jbc.RA120.013939
28. Radin M, Cecchi I, Roccatello D, Meroni PL, Sciascia S. Prevalence and Thrombotic Risk Assessment of Anti-β2 Glycoprotein I Domain I Antibodies: A Systematic Review. Semin Thromb Hemost (2018) 44:466–74. doi: 10.1055/s-0037-1603936
29. Andreoli L, Chighizola CB, Nalli C, Gerosa M, Borghi MO, Pregnolato F, et al. Clinical characterization of antiphospholipid syndrome by detection of IgG antibodies against β2 -glycoprotein i domain 1 and domain 4/5: ratio of anti-domain 1 to anti-domain 4/5 as a useful new biomarker for antiphospholipid syndrome. Arthritis Rheumatol (2015) 67:2196–204. doi: 10.1002/art.39187
30. Dziamski K, Sharmeen S, Banki K, Perl A. Nine-test panel has superior sensitivity to detect antiphospholipid antibody syndrome in patients with or without SLE. Clin Immunol (2020) 214:108388. doi: 10.1016/j.clim.2020.108388
31. Devreese KMJ, Ortel TL, Pengo V, de Laat B. Subcommittee on Lupus Anticoagulant/Antiphospholipid Antibodies. Laboratory criteria for antiphospholipid syndrome: communication from the SSC of the ISTH. J Thromb Haemost (2018) 16:809–13. doi: 10.1111/jth.13976
32. Cattini MG, Bison E, Pontara E, Cheng C, Denas G, Pengo V. Tetra positive thrombotic antiphospholipid syndrome: Major contribution of anti-phosphatidyl-serine/prothrombin antibodies to lupus anticoagulant activity. J Thromb Haemost (2020) 18:1124–32. doi: 10.1111/jth.14765
33. García-Carrasco M, Galarza-Maldonado C, Mendoza-Pinto C, Escarcega RO, Cervera R. Infections and the Antiphospholipid Syndrome. Clin Rev Allergy Immunol (2009) 36:104–8. doi: 10.1007/s12016-008-8103-0
34. Mackman N, Antoniak S, Wolberg AS, Kasthuri R, Key NS. Coagulation Abnormalities and Thrombosis in Patients Infected With SARS-CoV-2 and Other Pandemic Viruses. Arterioscler Thromb Vasc Biol (2020) 40:2033–44. doi: 10.1161/ATVBAHA.120.314514
35. Cugno M, Meroni PL, Gualtierotti R, Griffini S, Grovetti E, Torri A, et al. Complement activation in patients with COVID-19: A novel therapeutic target. J Allergy Clin Immunol (2020) 146:215–17. S0091–6749(20)30650-3. doi: 10.1016/j.jaci.2020.05.006
36. Pregnolato F, Gerosa M, Raimondo MG, Comerio C, Bartoli F, Lonati PA, et al. EUREKA algorithm predicts obstetric risk and response to treatment in women with different subsets of anti-phospholipid antibodies. Rheumatol (Oxford) (2020) 22:keaa203. doi: 10.1093/rheumatology/keaa203
37. Wyman B, Perl A. Metabolic pathways mediate pathogenesis and offer targets for treatment in rheumatic diseases. Curr Opin Rheumatol (2020) 32:184–91. doi: 10.1097/BOR.0000000000000687
Keywords: anti-phospholipid antibodies, β2-glycoprotein I, prothrombin, autoimmunity, COVID-19, thrombosis
Citation: Borghi MO, Beltagy A, Garrafa E, Curreli D, Cecchini G, Bodio C, Grossi C, Blengino S, Tincani A, Franceschini F, Andreoli L, Lazzaroni MG, Piantoni S, Masneri S, Crisafulli F, Brugnoni D, Muiesan ML, Salvetti M, Parati G, Torresani E, Mahler M, Heilbron F, Pregnolato F, Pengo M, Tedesco F, Pozzi N and Meroni PL (2020) Anti-Phospholipid Antibodies in COVID-19 Are Different From Those Detectable in the Anti-Phospholipid Syndrome. Front. Immunol. 11:584241. doi: 10.3389/fimmu.2020.584241
Received: 16 July 2020; Accepted: 25 September 2020;
Published: 15 October 2020.
Edited by:
Rolando Cimaz, University of Milan, ItalyReviewed by:
Andras Perl, Upstate Medical University, United StatesCopyright © 2020 Borghi, Beltagy, Garrafa, Curreli, Cecchini, Bodio, Grossi, Blengino, Tincani, Franceschini, Andreoli, Lazzaroni, Piantoni, Masneri, Crisafulli, Brugnoni, Muiesan, Salvetti, Parati, Torresani, Mahler, Heilbron, Pregnolato, Pengo, Tedesco, Pozzi and Meroni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicola Pozzi, bmljb2xhLnBvenppQGhlYWx0aC5zbHUuZWR1; Pier Luigi Meroni, cGllcmx1aWdpLm1lcm9uaUB1bmltaS5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.