- 1Department of Microbiology and Immunology, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States
- 2The Wilmot Cancer Center, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States
Educating the next generation of physicians is a key means of communicating and disseminating impactful immunologic scientific knowledge, and its practical application to human disease. We present our perspective, using as our model a first-year medical school course entitled Host Defense. As the name suggests, immunology is the overarching principle that links the multiple subjects in the course. We address a range of immunologically relevant topics, including innate and adaptive immunity, vaccines, inflammation, allergy, tumor immunotherapy, transplantation, and autoimmunity. These topics are integrated with the fields of infectious diseases, pathology, clinical laboratory testing, and public health, to illustrate how the basic science discoveries in immunology are relevant to clinical practice. The course objectives are not only to deliver “first principles” and molecular mechanisms, but also to connect these principles with the clinical world of diagnosis and therapy. We detail the different methodologies used to achieve these objectives and to reach today's medical students. This provides a framework for course structure and execution designed to engage both the novice and the more “immunologically experienced” learner. The framework includes classical didactic components and personalized instructor access, aligned with current approaches to self-directed learning and using digital media. We also address some of the challenges of assembling a course like Host Defense in the context of an academic medical center with multiple scientific, educational, and clinical missions. This perspective is not meant be proscriptive, but rather to outline our experiences on the strategies tried, while describing their advantages and drawbacks in teaching immunology.
Introduction
Connecting the concepts of immunology to the clinic is a challenge for medical students (1, 2). To quote a clinician/educator at our institution, “Of all the science topics covered in medical school, immunology was one of the hardest to wrap my head around.” Achieving this goal is not trivial for either learner or instructor. The learner can be daunted by the ever expanding “alphabet soup” constituting the language of immunology; cytokines, chemokines, effector molecules, cell types, cell surface receptors. The instructor cannot elucidate immunology's basic concepts without extensive use of terminology. Furthermore, effective teaching of immunological concepts requires integration of basic knowledge from multiple disciplines in the context of clinical observations and laboratory findings (3, 4).
We describe strategies for teaching immunology to first year medical students. In a course entitled Host Defense, we integrate immunological topics with the fields of infectious diseases, pathology and laboratory testing to explore the impact of the immune response on human health. The course is designed to deliver “first principles,” and to connect these principles with the clinical world of diagnosis and therapy. Herein, we address the following questions:
• What are the main challenges of course organization?
• How can we integrate digital media into education?
• How does one connect basic science to the clinical world in a way that is both educational and meaningful?
• What are some emerging trends in immunology education?
In this Perspective, we describe strategies that worked well for us, and some that did not. We also provide specific examples in the hope that others might adapt these strategies in their unique medical education and immunology teaching settings.
Logistics
Logistics, “the detailed coordination of a complex operation involving many people, facilities, or supplies” is an underappreciated, yet crucial, part of any course. The importance of logistics has long been appreciated by the military.
“Amateurs talk about tactics, but professionals study logistics.” –Gen Robert H. Barrow, USMC, as well as others.
“My logisticians are a humorless lot … they know if my campaign fails, they are the first ones I will slay.” –Alexander the Great.
Running a course that involves multiple lecturers, spans several disciplines and includes activities outside of lecture, presents a logistical challenge. Importantly, from the faculty standpoint, the quote from Alexander is relevant—if there are problems with delivery of the material, or performance of medical students on standardized tests such as USMLE Step 1, it is the director of the course who pays the price! Thus, the logistics of the course matters; determining the number of hours of didactic instruction, organizing specific topics to optimize the flow of ideas, scheduling, and recruiting lecturers as well as facilitators for Problem Based Learning (PBL) groups are just some of the hurdles.
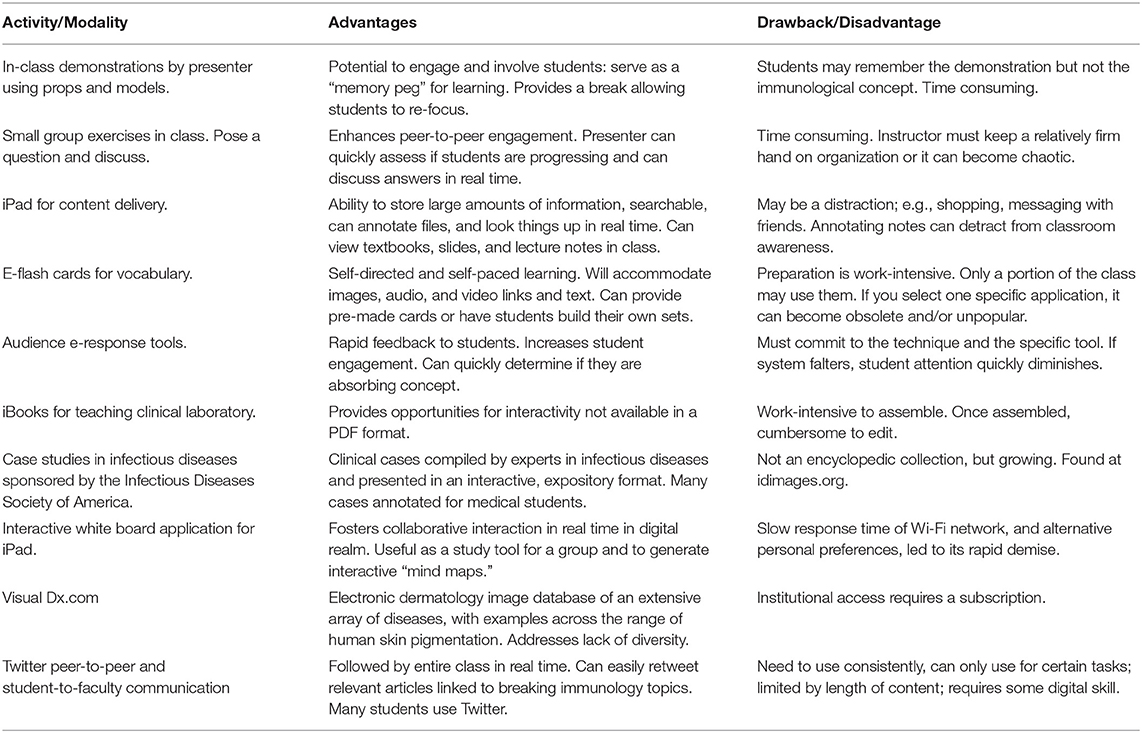
We must now also grapple with the challenge of integrating the digital world into a course in ways that engage students, provides current, accurate information, and enhances learning. Table 1 summarizes the advantages and disadvantages of e-resources we utilized in Host Defense. To bridge the traditional and digital worlds, we advocate a hybrid strategy where selected content can be delivered using a self-study, electronic format (5), so that in-person lecture can be used to integrate key concepts in the context of health and disease (6). A full description of our course structure, learning objectives and lecture materials is provided in Table S1. The next several sections describe our experiences, and challenges we faced in organizing the course and its content.
Transition to Digital Content
Many features of digital content delivery appeal to today's students. Links embedded in a document, and the ability to look up unfamiliar terms or find digital images instantly, enrich the learning experience (7). These advantages led many medical schools, including our own in 2012, to use electronic tablets (in our case, iPads) to deliver didactic content. Using electronic content freed us from printing a 650-page syllabus weeks in advance, allowing editing of the content closer to lecture. Over time, we moved from syllabus replacement to using the iPad to deliver new material linked to lecture content. With the invaluable help of our institution's instructional design expert, we introduced on-line modules to explore diagnostic laboratory microbiology (8, 9). Modules on bacteriology and virology were contained in five iBooks linked to clinical cases (www.idimages.org), each followed by a computer-based self-assessment of knowledge related to the diagnostic tests (Table 1).
We did face challenges in using iPads for content delivery. To quote Marshall McLuhan, “The medium is the message” (10). We found there were unanticipated consequences to introducing new technology that changes the inter-personal dynamics between instructor and learner. During lecture, students focusing on the iPad, and not the lecturer, detracted from the ability of the lecturer to “read” the audience and gauge the effectiveness of their delivery. Unfortunately, this parallels the filing of electronic medical records while interviewing a patient, to the dismay of patients and physicians alike. The interaction between the student and the lecturer is further compromised if the student succumbs to the temptation to use the tablet or laptop for activities unrelated to lecture, e.g., shopping, messaging with friends, etc., as their attention wanders (11).
The Perils and Pitfalls of E-Learning Tools
While the iBooks used to explore diagnostic microbiology were viewed favorably, we cite two experiences where introducing electronic learning tools into Host Defense did not proceed as smoothly as hoped.
Learning vocabulary remains an essential step in immunology and, indeed, all of medicine. Clinicians use this vocabulary daily, and remark that medical vocabulary is the major part of the first 2 years of medical school. Although many students view memorization of terminology pejoratively, there is no more rapid means to shred professional credibility than to mangle the vocabulary. Defaulting to “However you say it …” is no longer acceptable.
In consultation with both students and our instructional design team, we prepared an extensive set of e-flashcards with application Study© for the vocabulary of immunology and infectious diseases to be used in a self-study format. The application was purchased by our institution, provided to each student and formal instruction offered. Along with text, incorporating audio allowed us to add the proper pronunciation for a given term. Despite expending considerable effort to create the e-flashcards, it did not translate into widespread utilization by students. One colleague quipped, “If you build it, they won't come.” Course surveys revealed only ~25% of the class found the e-flashcards “very useful.” In contrast, a professional, visually based program employing “memory pegs” (12) and animation, SketchyMicro©, was considerably more popular, with ~75% finding it “very useful.” Illustrating the gap between students and faculty, we were initially unaware of the degree to which SketchyMicro© was adopted, even though the more popular application was relatively expensive and available only for rent.
In a second instance, we observed students using an interactive computer whiteboard to share content in real time over the Internet and create concept maps (13, 14) as a study tool. With the help of these students and our instructional design expert, we introduced and demonstrated a free, interactive whiteboard iPad application to the entire class during a lecture. We tasked all students to use the application in their respective Problem Based Learning (PBL) group to replace the conventional classroom whiteboard. Our goal was to make it easier to share learning objectives and concept maps of Host Defense PBL cases with the class. Disappointingly, our “top-down” approach quickly crashed, and the students stopped using it after 1–2 sessions. Students stated that the response time of the network was too slow to keep pace with the group's discussion. It was faster to simply write on the board and take a picture on their phone. Furthermore, many students had already been using other platforms, such as Google Docs, and were unwilling to switch. We learned the hard lesson that students often outpace faculty in identifying and adopting new digital applications. Moreover, their popularity can change rapidly through peer-to-peer communication to which faculty are often not privy.
Copyright and Fair Use
The advent of digital content delivery raises the question: How does one use textbooks, particularly in the context of lectures? Does one create all one's own figures (a time consuming and daunting task) or use existing material? In the latter case, there are numerous immunology textbooks, with excellent, professionally designed figures. However, with the steady decline in the purchase of textbooks by students, copyright issues rise to the fore.
Issues surrounding Fair Use of copyrighted material depend upon the precise circumstances when they are used (15–18). Instructors have long used published figures to supplement their lectures, and this has generally been deemed permissible. However, if the course materials are posted on-line, ease of re-distribution can pose copyright problems. If the library buys a site license for a course text, this issue can be mitigated to some extent. However, as we have experienced, if the library buys a site license and later discontinues it, you may need to redo the digital content for your entire course. Posting class materials on portals with access restricted to registered students, such as Blackboard, may serve as an important barrier to potential copyright infringement. Nevertheless, if copyright infringement is alleged, the instructors are usually left to fend for themselves (15). Your institution's library staff is a good resource for Fair Use guidelines to help navigate these issues.
Making Connections Between Disciplines
Understanding immunological concepts requires the expert integration of multiple disciplines and concepts. Can you teach someone to be an expert in immunology in a medical school class? Obviously, not; becoming an expert takes years of intense effort and dedication. However, it is possible to illustrate how experts think by using examples to make connections between topics students perceive as disparate (19). To illustrate passive immunity, we described the delivery of anti-toxin by the sled dog Balto for the treatment of an outbreak of diphtheria in the Inuit population of Nome, Alaska (20). This was used to segue into serum sickness, Lupus, Rh disease, rattlesnake bite therapy, monoclonal antibodies, and tumor immunotherapy (Figure 1A). We have also used concept mapping (13, 14) to connect the fields of infectious disease, inflammation and adaptive immunity. In a lecture “From Bacterial Capsules to Vaccines,” we start with classic studies from the 1920's on infection caused by Streptococcus pneumoniae to describe how a bacterial structure, polysaccharide capsule, results in evasion of phagocytosis, leading to lung inflammation and consequent pneumonia (Figure 1B). We then transition to the bacterial capsule as an immunogen to explore the concepts of antibodies as opsonins, pneumococcal serotypes, conjugate vaccine design, and immune evasion using the same concept mapping approach.
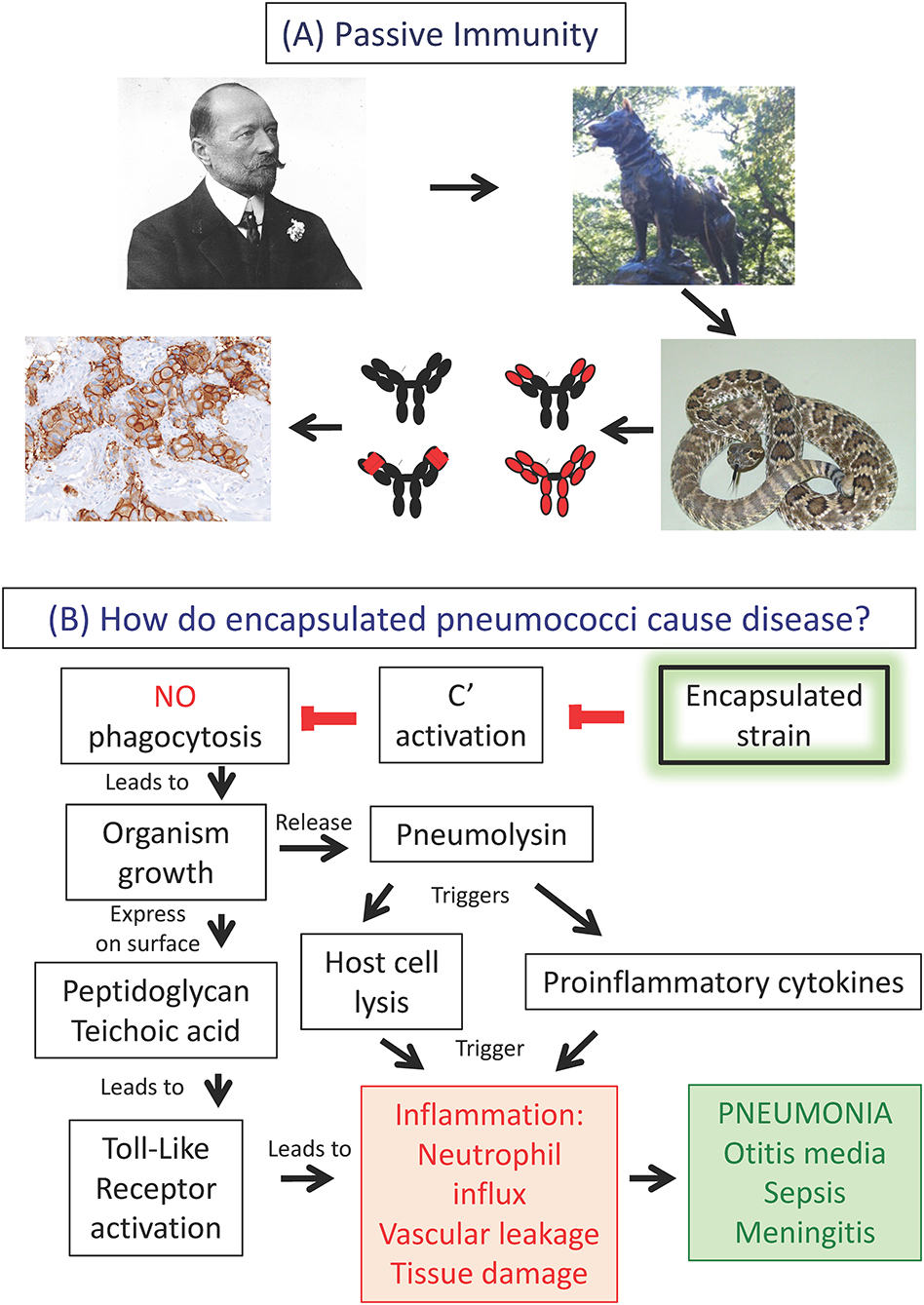
Figure 1. Making connections between disciplines. (A) Antibodies in immunity, disease and therapy. (A) Illustrates one example used in didactic lectures to make connections in immunology. This slide design is used in lecture to create “memory pegs” between material covered in the course and to demonstrate how many of the same basic principles can be applied to several clinically relevant situations. Here we show a picture of the Nobel prize winner von Behring who developed diphtheria antitoxin. This form of passive immunity was memorably applied in the delivery of antitoxin by the sled dog Balto and his owner Gunnar Kaasen for the treatment of an outbreak of diphtheria in Nome, Alaska. From here one can segue into the role of antibodies in treating snakebites, the structure of antibodies to minimize immune complex disease, the modern use of passive immunization using humanized monoclonal antibodies such as Herceptin® (trastuzumab) for tumor immunotherapy, and other related topics such as Rh disease. Links to additional slides and other educational resources for teaching Immunology can be found at the American Association of Immunologists (AAI) website (https://www.aai.org/Education/Teaching-Resources). (B) Connecting infectious disease, inflammation and adaptive immunity with concept mapping using the bacterium Streptococcus pneumoniae, the pneumococcus, as an example. How do encapsulated pneumococci cause disease? Inhaled encapsulated strains fail to activate complement, thereby evading phagocytosis by alveolar macrophages followed by outgrowth of the organism. Bacterial cell walls, containing peptidoglycan and teichoic acid, activate Toll-like receptors, inducing inflammation. Concomitantly, the bacterium releases the protein pneumolysin, lysing lung cells and inducing proinflammatory cytokines, thereby exacerbating inflammation. Neutrophil influx, vascular leakage and tissue damage manifest as pneumonia, with potential dissemination of infection to extra-pulmonary sites.
Connecting to the Clinic
Medical students recall immunological concepts most effectively when they are placed in a clinical context (6, 21–23). We make clinical correlations by incorporating cutting-edge immunology topics in the news and examining mishaps that occur in medicine, such as transplanting a mismatched kidney. We can review not only the immunology involved, but also encourage discussions on medical ethics. To strengthen the link between basic and clinical immunology (24), we conduct in-class small group exercises to measuring immune responses, with emphasis on the uses of antibodies. Further, we have a series of PBL sessions based on clinical cases emphasizing basic science that, with the help of a facilitator, students work through as a team.
We incorporate physicians into the course; as lecturers in their area of expertise to connect basic science to clinical care, but also to communicate how they think about patients (25). We have a clinical immunologist deliver lectures on inflammation, hypersensitivity, asthma, and autoimmunity, and the roles of monoclonal antibodies and other biologics in the therapy of immunologic diseases. We then reinforce and expand these concepts by recruiting a dermatologist to lecture on cutaneous manifestations of adverse drug reactions. We also have two in-class sessions on clinical decision-making in infectious diseases. Clinicians describe their own cases and the decisions they made in terms of diagnosis, therapy and follow-up; emphasizing the evolution of their thinking over time. While clinical vignettes can never fully replicate the experience of a physician connecting with an individual patient for whom they are responsible, they can demonstrate how an expert physician integrates basic science into clinical medicine. The physicians inter-weave all aspects of patient history with basic and clinical science, while communicating their sense of responsibility for the patient's well-being.
The clinical lectures by physicians also serve as an important bridge between the basic science and clinical spheres, and illustrate how basic science information is applied. For example, as shown in Figure 1, we explore the role of the antibody and complement in promoting phagocytosis of encapsulated bacteria. Complement and immune complexes are reintroduced in the context of serum sickness resulting from the passive immunization against diphtheria toxin using horse serum (see Balto, Figure 1), and later in the context of immune complex diseases such as systemic lupus erythematosus (SLE). Complement comes up yet again in a discussion of immunodeficiencies, exemplified by increased susceptibility to infection by the bacterium Neisseria meningitidis, as well as increased frequency of autoimmune diseases. The spaced repetition of the complement system in different contexts is not only an excellent learning tool (26), but also helps to integrate the multidisciplinary field of immunology.
Integrating clinicians into a course poses challenges. First, the lecturer often over-estimates the students' clinical knowledge. Consequently, students often feel overwhelmed by their presentations. It is also hard to schedule clinicians to fit within the flow of the course, as their patient care responsibilities always come first. Finally, the clinicians usually do not have the time to examine the course content in detail. A common expression uttered, which never fails to cause considerable consternation among students (and the directing faculty), is “I don't know if you've had this yet, but…,” giving the unfortunate perception that the course is disorganized and lecturers do not communicate with each other. We coach the lecturers to not use that phrase (not always successfully) by emphasizing where we are in the lecture series and the relative level of audience expertise.
Offering the Best of Both Worlds
We embrace the utility of digital resources and understand their appeal (see Table 1 for details of resources and activities used in Host Defense, along with pros and cons). However, we feel strongly that the most important component of our course is a traditional one; direct interaction with students, in person. Students frequently request that lectures be video recorded; this is problematic from several standpoints. Viewing a video of a good lecture cannot adequately replace the dynamic of attending a good lecture, with the opportunity to view the spectrum of instructor-student interactions, questions, and comments. Video recording of lectures also inevitably leads to a decrease in attendance, resulting in less interaction with instructors and with peers (27).
Effective interaction with a large class requires moving beyond standing at the podium, holding forth for an hour and then exiting the room. We use several approaches to facilitate that interaction, summarized in Table 1. For example, to restore waning student attention during lectures, students are routinely called upon to participate in demonstrations in front of the class that illustrate major teaching points. We also intersperse lectures with small group activities to both make teaching points and help foster teamwork. The instruction team must also find a balance between course objectives and the time students need to master the material. We provide in-class time to perform computer-based exercises to provide personalized instruction, if needed. The course director attends all lectures, and is available to consult with students in the lecture hall when no formal lectures are scheduled, a time we have termed Questions and Answers (Q and A).
Like many institutions, we use similar multiple choice questions to those on Step 1 USMLE as one of our assessment mechanisms. However, it is challenging to construct questions that truly assess students' grasp of conceptual knowledge or their ability to synthesize and apply concepts in immunology. To address this issue, we have tried several types of writing exercises that also provide feedback to instructors as to gaps in the student's knowledge. Our current approach, favored by students and instructors alike, is a small-group exercise performed outside of class explaining the underlying immunology involved in an article or video from a popular media source. This reflected the increasing frequency of immunology-based treatments, or clinical scenarios involving immunology, described in commercial or social media, with the expectation that their future patients will want explanations of these new treatments. The group could either choose an article or pick from a list provided. For example, one article titled “HIV used to cure ‘bubble boy' disease” instead described using gene therapy to cure severe combined immunodeficiency disease. Each group was tasked with explaining the immunologic mechanisms of the treatment, its advantages over previous approaches, potential drawbacks, or adverse consequences, cost considerations, and any biomedical errors perceived in the article. Their report was limited to two pages, including a picture or diagram of the immunologic mechanisms involved and a description of the issues just described. All students were expected to read the reports of the other groups. Students valued the opportunity to be creative, work as a team, and to take an active role in directing their learning process.
In all these exercises, logistics, in terms of planning, timing in the lecture and smooth execution, are critical. Faculty time, commitment and direct in-person guidance are essential to maintain their organization and assure communication of the outcomes of the activities to the entire class. Since the initiation of significant course re-modeling in 2012, student surveys demonstrated an increase in the quality of teaching and the quality of the course overall. We used a Likert-like rating scale from 1 to 5 with the following categories: 1. “Needs much improvement,” 2. “Needs some improvement,” 3. “Satisfactory,” 4. “Good” and 5. “Excellent.” Ratings for the course overall improved steadily from slightly below “Satisfactory” in 2011, with an average score of 2.80, to scores consistently in the “Good” to “Excellent” category in 2015 through 2018, with averages ranging from 4.29 to 4.41. Concomitantly, the ratings for overall quality of teaching in 2015–2018 were also in the “Good” to “Excellent” category, with averages ranging from 4.36 to 4.47.
Discussion
We advocate a self-study, electronic format to deliver specific content (5) that affords lecture time to integrate key concepts in the context of health and disease (6). Appreciating that learning may be enhanced by complementing didactic lectures with interactive activities (2, 7, 28, 29), lecture can be supplemented with brief, small group activities during lecture, and in more detailed PBL sessions spanning several days. This hybrid approach is extremely flexible. Recognizing that digital technologies and innovations are constantly being developed, one can blend and experiment with digital advances, while maintaining the best of traditional methods.
The experiences we have described are with medical education in the U.S. We have also utilized the hybrid approach in our basic science courses in microbiology and immunology for undergraduates and graduate students. Moreover, we believe that these lessons will also be valuable to educators outside of the U.S. because many of the challenges faced, particularly on how to incorporate the ever-expanding modes of delivering information, are shared concerns. These educational issues include the balance of traditional methods such as lectures with electronic resources, the increasing adoption and preferences of students for digital modalities, and the role of broad electronic platforms such as internet web sites and social media. These issues are common to educational endeavors wherever one teaches. This shared experience is reflected in studies from outside the U.S. cited herein, including those on student interest in immunology (Australia) (1), use of electronic tablets (United Kingdom) (3) and e-resources (Brazil, Germany, Switzerland) (2, 28, 29) in teaching, and connecting basic science to the clinical world (Canada) (3, 23, 25). Furthermore, it is increasingly recognized that educational strategies must be developed for teaching immunology in the resource-constrained regions of the developing world (30). Open access to internet-based, digital resources (2), such as those listed in Faggioni et al. (31), will facilitate closing the gaps between under-served regions and developed areas of the world. In addition, through their respective Education Committees, the International Union of Immunological Societies (iuisonline.org, in association with immunopaedia.org) and the American Association of Immunologists (aai.org/Education/Teaching-Resources) are committed to providing and disseminating quality digital educational resources, as well as organizing meetings and courses, to fill this need. We hope that the strategies we propose herein will help guide the use of these electronic resources effectively.
Looking to the future, we see three emerging technological trends that we anticipate will make major impacts in teaching immunology and related disciplines. They include:
1. A multi-institution collaboration to develop a “shared medical school curricular ecosystem” has been proposed (32, 33) using online videos to deliver core content to preclinical students, thereby affording faculty more class time to facilitate personalized, interactive learning experiences.
2. The increased incorporation of social media (34) including blogging (35) and Twitter (36–38), to facilitate student-student and student-faculty communication.
3. The integrated analysis of the human immune response and systems immunology (39), which require concomitant development of both basic immunological literacy and information literacy skills (40–42) early in medical training.
Whatever the future holds, one can be certain that Immunology will impact nearly every aspect of a physician's practice (24). The sophisticated technological approaches that will become “normal” for today's students as they move into medical practice will be deprived of their potential promise without fostering life-long learning and interest in immunology early in their training. However, we are cognizant of a time-tested quote:
“The only thing constant is change” –Heraclitus.
In that light, we advocate a blend of methods to teach the concepts and applications of immunology, but one that affords the flexibility to adapt to changing times. Immunologists, of course, excel at adapting!
Author Contributions
CH and JF contributed equally to the concept, organization and writing of this manuscript.
Funding
This work was supported in part by the Lawrence E. Young Dean's Teaching Fellowship from the University of Rochester School of Medicine and Dentistry to CH and by a generous gift from Steve and Alison Krausz to JF.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Ronald M. Epstein M.D., Catherine Frelinger M.D., Sandra H. Jee M.D., and Anne Nofziger M.D. for helpful comments and suggestions on the manuscript. The authors want to acknowledge that the image of Her2 immunocytochemistry in Figure 1A was used under the creative commons usage. This file is licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license. The Image was found at https://commons.wikimedia.org/wiki/File:Breast_invasive_scirrhous_carcinoma_histopathology_(2)_HER2_expression.JPG#filehistory. The image of von Behring was cropped from a photograph from the Welcome Collection and used under Creative Commons Attribution (CC BY 4.0) terms and conditions https://creativecommons.org/licenses/by/4.0 Emil von Behring. Photograph. Credit: Wellcome Collection. CC BY. The image was found at https://wellcomecollection.org/works/pcczg3pk.
The image of the snake is found at https://commons.wikimedia.org/wiki/File:Crotalus_scutulatus_02.JPG.
This work has been released into the public domain by its author. This applies worldwide. In some countries, this may not be legally possible; if so: grants anyone the right to use this work for any purpose, without any conditions, unless such conditions are required by law.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2019.02548/full#supplementary-material
References
1. Bansal AS. Medical students' views on the teaching of immunology. Acad Med. (1997) 72:662. doi: 10.1097/00001888-199708000-00006
2. Bercot FF, Fidalgo-Neto AA, Lopes RM, Faggioni T, Alves LA. Virtual immunology: software for teaching basic immunology. Biochem Mol Biol Educ. (2013) 41:377–83. doi: 10.1002/bmb.20733
3. Kulasegaram KM, Martimianakis MA, Mylopoulos M, Whitehead CR, Woods NN. Cognition before curriculum: rethinking the integration of basic science and clinical learning. Acad Med. (2013) 88:1578–85. doi: 10.1097/ACM.0b013e3182a45def
4. Manglik N, Dudrey EF, Baatar D, Piskurich JF. Immune response to bacteria: an integrated learning module to enhance preclinical students' competency in immunology. MedEdPORTAL. (2017) 13:10585. doi: 10.15766/mep_2374-8265.10585
5. Knight JK, Wood WB. Teaching more by lecturing less. Cell Biol Educ. (2005) 4:298–310. doi: 10.1187/05-06-0082
6. Wilkerson L, Stevens CM, Krasne S. No content without context: integrating basic, clinical, and social sciences in a pre-clerkship curriculum. Med Teach. (2009) 31:812–21. doi: 10.1080/01421590903049806
7. Patel S, Burke-Gaffney A. The value of mobile tablet computers (iPads) in the undergraduate medical curriculum. Adv Med Educ Pract. (2018) 9:567–70. doi: 10.2147/AMEP.S163623
8. Baker N, Verran J. The future of microbiology laboratory classes–wet, dry or in combination? Nat Rev Microbiol. (2004) 2:338–42. doi: 10.1038/nrmicro868
9. Blewett EL, Kisamore JL. Evaluation of an interactive, case-based review session in teaching medical microbiology. BMC Med Educ. (2009) 9:56. doi: 10.1186/1472-6920-9-56
11. Kirschner PA, DeBruckyere P. The myths of the digital native and multitasker. Teach Teac Educ. (2017) 67:135–42. doi: 10.1016/j.tate.2017.06.001
12. Foer J. Moonwalking With Einstein: The Art and Science of Remembering Everything. New York, NY: Penguin Press (2011).
13. Daley BJ, Torre DM. Concept maps in medical education: an analytical literature review. Med Educ. (2010) 44:440–8. doi: 10.1111/j.1365-2923.2010.03628.x
14. Laight DW. Attitudes to concept maps as a teaching/learning activity in undergraduate health professional education: influence of preferred approach to learning. Med Teach. (2006) 28:e64–7. doi: 10.1080/01421590600617574
15. Dobbins WN, Souder E, Smith RM. Living with fair use and TEACH: a quest for compliance. Comput Inform Nurs. (2005) 23:120–4. doi: 10.1097/00024665-200505000-00005
16. Spallek H, Schleyer TK. Educational implications for copyright in a digital world. J Dent Educ. (1999) 63:673–81.
17. Lyons MG. Open access is almost here: navigating through copyright, fair use, and the TEACH Act. J Contin Educ Nurs. (2010) 41:57–64. doi: 10.3928/00220124-20100126-03
20. Aboul-Enein BH, Puddy WC, Bowser JE. The 1925 diphtheria antitoxin run to nome - alaska: a public health illustration of human-animal collaboration. J Med Humanit. (2016) 40:287–96. doi: 10.1007/s10912-016-9428-y
21. Kennelly PJ, Bond JS, Masters BS, Dennis EA, Brenner C, Raben DM. Desperately seeking Flexner: time to reemphasize basic science in medical education. Acad Med. (2013) 88:1405–6. doi: 10.1097/ACM.0b013e3182a225be
22. Brauer DG, Ferguson KJ. The integrated curriculum in medical education: AMEE Guide No. 96. Med Teach. (2015) 37:312–22. doi: 10.3109/0142159X.2014.970998
23. Weston WW. Do we pay enough attention to science in medical education? Can Med Educ J. (2018) 9:e109–14.
24. Tebo AE, Detrick B, Hamilton RG, Khanolkar A, O'Gorman MR, Schmitz JL, et al. Clinical laboratory immunology: an indispensable player in laboratory medicine. Am J Clin Pathol. (2014) 142:437–44. doi: 10.1309/AJCPX25MFWNEYRIG
25. Norman G. Research in clinical reasoning: past history and current trends. Med Educ. (2005) 39:418–27. doi: 10.1111/j.1365-2929.2005.02127.x
26. Matos J, Petri CR, Mukamal KJ, Vanka A. Spaced education in medical residents: an electronic intervention to improve competency and retention of medical knowledge. PLoS ONE. (2017) 12:e0181418. doi: 10.1371/journal.pone.0181418
27. Zureick AH, Burk-Rafel J, Purkiss JA, Hortsch M. The interrupted learner: how distractions during live and video lectures influence learning outcomes. Anat Sci Educ. (2018) 11:366–76. doi: 10.1002/ase.1754
28. Colsman A, Sticherling M, Stopel C, Emmrich F. Computer-assisted learning in medicine. How to create a novel software for immunology. Arch Dermatol Res. (2006) 298:1–6. doi: 10.1007/s00403-006-0665-1
29. Debard N, Py P, Kraehenbuhl JP, Fuchs J. The influence of the Internet on immunology education. Nat Rev Immunol. (2005) 5:736–40. doi: 10.1038/nri1687
30. Fournie JJ, Gaits F, Bonneville M. Science and society: promoting the learning of immunology in developing countries. Nat Rev Immunol. (2005) 5:893–8. doi: 10.1038/nri1709
31. Faggioni T, da Silva Ferreira NC, Lopes RM, Fidalgo-Neto AA, Cotta-de-Almeida V, Alves LA. Open educational resources in immunology education. Adv Physiol Educ. (2019) 43:103–9. doi: 10.1152/advan.00116.2018
32. Chen SF, Deitz J, Batten JN, DeCoste-Lopez J, Adam M, Alspaugh JA, et al. A multi-institution collaboration to define core content and design flexible curricular components for a foundational medical school course: implications for national curriculum reform. Acad Med. (2019) 94:819–25. doi: 10.1097/ACM.0000000000002663
33. Le TT, Prober CG. A proposal for a shared medical school curricular ecosystem. Acad Med. (2018) 93:1125–8. doi: 10.1097/ACM.0000000000002194
34. Sutherland S, Jalali A. Social media as an open-learning resource in medical education: current perspectives. Adv Med Educ Pract. (2017) 8:369–75. doi: 10.2147/AMEP.S112594
35. Cohen Z, Cohen JJ. Inflammablog: peer-to-peer online learning in immunology. Immunol Res. (2013) 55:71–4. doi: 10.1007/s12026-012-8374-7
36. Banerjee Y, Tambi R, Gholami M, Alsheikh-Ali A, Bayoumi R, Lansberg P. Augmenting flexnerism via twitterism: need for integrating social media application in blueprinting pedagogical strategies for undergraduate medical education. JMIR Med Educ. (2019) 5:e12403. doi: 10.2196/12403
37. Hennessy CM, Kirkpatrick E, Smith CF, Border S. Social media and anatomy education: Using twitter to enhance the student learning experience in anatomy. Anat Sci Educ. (2016) 9:505–15. doi: 10.1002/ase.1610
38. Forgie SE, Duff JP, Ross S. Twelve tips for using Twitter as a learning tool in medical education. Med Teach. (2013) 35:8–14. doi: 10.3109/0142159X.2012.746448
39. Davis MM, Tato CM, Furman D. Systems immunology: just getting started. Nat Immunol. (2017) 18:725–32. doi: 10.1038/ni.3768
40. Kingsley K, Galbraith GM, Herring M, Stowers E, Stewart T, Kingsley KV. Why not just Google it? An assessment of information literacy skills in a biomedical science curriculum. BMC Med Educ. (2011) 11:17. doi: 10.1186/1472-6920-11-17
41. Kingsley KV, Kingsley K. A case study for teaching information literacy skills. BMC Med Educ. (2009) 9:7. doi: 10.1186/1472-6920-9-7
Keywords: immunology, medical, education, digital, clinical
Citation: Haidaris CG and Frelinger JG (2019) Inoculating a New Generation: Immunology in Medical Education. Front. Immunol. 10:2548. doi: 10.3389/fimmu.2019.02548
Received: 27 June 2019; Accepted: 14 October 2019;
Published: 01 November 2019.
Edited by:
Fulvio D'Acquisto, University of Roehampton London, United KingdomReviewed by:
Amit Rawat, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaKingston H. Mills, Trinity College Dublin, Ireland
Copyright © 2019 Haidaris and Frelinger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Constantine G. Haidaris, Y29uc3RhbnRpbmVfaGFpZGFyaXNAdXJtYy5yb2NoZXN0ZXIuZWR1
 Constantine G. Haidaris
Constantine G. Haidaris John G. Frelinger
John G. Frelinger