- 1Department of Endocrinology and Metabolism, The Second Xiangya Hospital of Central South University, Changsha, China
- 2Department of Endocrinology, Key Laboratory of Endocrinology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences, Beijing, China
- 3Department of Osteoporosis and Bone Diseases, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai, China
- 4Department of Endocrinology, Guangdong General Hospital, Guangzhou, China
- 5Department of Endocrinology, West China Hospital, Sichuan University, Chengdu, China
- 6Department of Orthopedics, The Second Affiliated Hospital of Harbin Medical University, Harbin, China
- 7Department of Rheumatism and Immunology, People's Hospital of Xinjiang Uygur Autonomous Region, Urumqi, China
- 8Department of Pharmacoepidemiology, Merck Research Laboratories, Merck & Co., Inc., Kenilworth, NJ, United States
- 9Department of Medical Affairs, MSD (China) Co., Ltd., Shanghai, China
- 10Asia Pacific Unit, Department of Pharmacoepidemiology, MSD (China) R&D Co., Ltd., Beijing, China
Purpose: We aimed to investigate the status of serum 25-hydroxyvitamin D [25(OH)D] among Chinese postmenopausal women in a multicenter cross-sectional study.
Methods: Non-institutionalized postmenopausal women aged ≥55 years were recruited from urban and rural areas in 7 geographically different regions in China. Subject enrollment was executed during the summer and the winter. Vitamin D insufficiency and deficiency were defined as 25(OH)D < 30 and <20 ng/ml, and was measured by liquid chromatography-tandem mass spectrometry. Women were referred to a dual-energy x-ray absorptiometry (DXA) if they had a medium-to-high fracture risk suggested by Osteoporosis Self-Assessment Tool for Asians (OSTA).
Results: Among all subjects, 91.2% (1,535/1,684, 95%CI: 89.7, 92.5) had vitamin D insufficiency and 61.3% had vitamin D deficiency (1,033/1,684, 95%CI: 59.0, 63.7). The prevalence of vitamin D deficiency was significantly higher in urban dwellers (64.9 vs. 57.7% in rural, P = 0.002) and in winter-enrolled subjects (84.7 vs. 41.3% in summer, P < 0.0001). The prevalence of vitamin D inadequacy did not increase in trend by latitude and was numerically lower in women who had high fracture risk and osteoporosis. A non-curvilinear change of intact parathyroid hormone (iPTH) levels was observed at 25(OH)D >16.78 ng/mL.
Conclusions: The prevalence of vitamin D inadequacy was remarkable among Chinese postmenopausal women and independent of fracture risk assessed by OSTA or osteoporosis suggested by DXA. Winter season, urban residence, however not latitude, were significantly associated with a higher likelihood of vitamin D deficiency. Optimal vitamin D status for iPTH and bone-related outcomes merits further investigation in this population.
Introduction
Vitamin D plays an important role in bone health by increasing intestinal absorption of calcium and phosphate and acts as a critical component in the regulation of bone turnover. Sunlight exposure is the primary source of vitamin D followed by dietary intake of vitamin D-rich or fortified foods, where available. Vitamin D deficiency, as measured by serum 25-hydroxyvitamin D [25(OH)D] (1), is associated with increased bone turnover, muscle weakness and falls, osteoporosis and fractures, and endocrine disorders including rickets in the young, osteomalacia in the elderly, and secondary hyperparathyroidism (2, 3). Inadequacy in vitamin D is a worldwide problem with unfavorable consequences, especially in elderly women (4–6). Global evidence has shown a considerable prevalence of vitamin D insufficiency among North American (6), European (7, 8), as well as Asian populations (9). However, vitamin D status of the population in Southeast Asian countries received relatively less attention. Despite efforts to determine the optimal or sufficient concentration of serum 25(OH)D, there is still no universal consensus on a definition of vitamin D deficiency or insufficiency (i.e., 25(OH)D < 30 or 20 ng/mL) as reflected in the recent disagreement between the Institute of Medicine (IOM) guidelines (10) and the recommendations made by the Endocrine Society (11).
Postmenopausal women are at high risk of vitamin D deficiency. Maintenance of serum 25(OH)D may protect this population from adverse skeletal outcomes (1). Observational studies in North and Northeast China (12–18) investigated vitamin D inadequacy across various urban populations. Different cutoff values were used to define vitamin D deficiency and variations in serum 25(OH)D measurement occurred due to non-standardized assay methods. Comparison of study results is somewhat difficult. In examining previous studies, epidemiological data focusing on Chinese postmenopausal women were insufficient. In addition, the current standardized laboratory method for measuring 25(OH)D by liquid chromatography-tandem mass spectrometry (LC-MS/MS) (19) was not universally used. Therefore, those studies may not have accurately estimated the prevalence of vitamin D inadequacy in postmenopausal women in China. Therefore, we aimed to describe the distribution of serum 25(OH)D levels among Chinese postmenopausal women who lived in both rural and urban areas by conducting a nationwide, multicenter, cross-sectional, epidemiological study. Secondly, risk factors for vitamin D deficiency and the relationship between 25(OH)D and intact parathyroid hormone (iPTH) were explored in this sampled population.
Methods and Materials
Study Design
This was a nationwide, multicenter, cross-sectional study to investigate the distribution of 25(OH)D levels among rural and urban-dwelling Chinese postmenopausal women from 7 geographic regions in China by different latitudes (from 45.75 to 23.17° north, Supplementary Figure 1). The selected regions represented a variety of geographic locations by latitude in China in order to assess the regional difference in serum 25(OH)D levels and risk factors for vitamin D deficiency. One tertiary hospital in each region was selected as the coordinating site based on the site's location (a major city in the region) and the investigator's medical specialty (endocrinologist, orthopaedist, or rheumatologist). Subject enrollment began in July 2013 and completed in February 2014. Considering the seasonal impact on sunlight exposure, a two-season enrollment strategy by summer vs. winter was executed for the study. The study sample size was evenly allocated across 7 sites where subjects were equally enrolled from the urban and rural areas, and from summer and winter seasons, respectively. MSD designed and sponsored the study and analyzed the data. The study was conducted in accordance with the guidelines of the International Conference on Harmonization and local regulatory guidance and was approved by independent ethics committees of all sites before the initiation of any study-related procedure.
Subject and Enrollment
Women were eligible if they were Chinese aged 55 years or above and postmenopausal (defined as absence of menses either naturally or surgically for at least a year by self-reporting), and willing to comply study procedure as judged by the investigators; women were excluded if they were hospitalized or institutionalized (i.e., patient in long-term care or elderly care facility), had severe kidney disease under physician's care, had mentally or legally incapacitated, or other conditions that may preclude the completion of health-related questionnaire or informed consent process, or had participated in a study with an investigational medicinal product or device within 30 days prior to giving informed consent.
Subject enrollment was conducted in the summer (between July and September 2013) and the winter (between January and February 2014), respectively, in one calendar year for six geographic regions where seasons are distinct. A single enrollment period (between December 2013 and January 2014) was applied in the southern region (Guangdong) due to limited seasonal variation and relatively warmer climate. The investigators obtained a population list for potential participants from local rural committees or urban residents' committees and recruited subjects accordingly with the assistance from these committees via approved telephone contact, advertisements, or posters. For the recruitment of rural subjects, one representing area (one to two villages) was selected for community-based recruiting of women by approved posters and broadcasting. Women were then screened in an outpatient clinic in the coordinating site. Written informed consent was obtained from all subjects or their legal representatives before study screening.
Clinical Assessment and Laboratory Measurement
A single study visit was arranged for the subject who was assessed as per study procedure onsite. Demographic data, medical history (non-active diseases/diagnoses) for the previous 5 years, and medication use (including vitamin D and calcium supplements) within the 4 weeks prior to the study visit were recorded for each subject. Height and weight were measured with shoes and heavy clothing removed using a standardized portable stadiometer and weighing scale. Fracture risk was assessed using the Osteoporosis Self-Assessment Tool for Asians (OSTA) (20), which has a demonstrated role in predicting fracture risks in Asian populations.
Subject Questionnaire
A structured, 30-item interviewer-administered questionnaire was used by the investigator onsite to assess potential factors influencing serum 25(OH)D levels including, general health, fall or fracture history, sun exposure (including time spent outside with and without sun protection and the body parts exposed), physical activity and daily, and weekly or monthly consumption of vitamin D-containing foods, such as eggs and fish. A sun exposure index was calculated using the reported number of hours per week spent outside without sun protection in the previous month multiplied by the percentage of the body exposed to sunlight (9% for the face, 1% for each hand, 9% for each arm, and 18% for each leg). Sun exposure of the chest, back, and abdomen were not included (21).
Laboratory Measurement
A fasting blood sample by 10 ml was collected from each subject and sent to a central laboratory (Quest Diagnostics, Shanghai, China). Serum 25(OH)D samples were measured using an API4000 (SCIEX™) LC-MS/MS, which quantified concentrations of 25(OH)D2 and 25(OH)D3 for the determination of total 25(OH)D. The limits of quantification (LOQs) for 25(OH)D2 and 25(OH)D3 were 2 and 3 ng/ml, respectively (LOQ total 25(OH)D = 3 ng/ml). The concentration of iPTH was measured using chemiluminescence (DPC Immulite 2000, SIEMENS) with an LOQ of 0.3 pg/mL. An additional fasting blood sample by 5 ml was collected from a subset of subjects enrolled from 3 regions (Beijing, Shanghai and Hunan) during the winter to measure bone turnover markers including serum C-terminal telopeptide of type I collagen (β-CTX) and serum N-aminoterminal propeptide of type I collagen (P1NP) using electrochemiluminescence (Roche E601 platform).
BMD Measurement
Bone mineral density (BMD) of the total hip, the lumbar spine, and the femoral neck were measured by dual-energy X-ray absorptiometry (DXA) with either a Hologic® or GE Lunar machine. Calibration with the manufacturer's phantom performed for routine clinical practice at each testing site was accepted.
Objectives and Outcome Measures
The primary objective was to describe the distribution of serum 25(OH)D levels among postmenopausal women aged 55 years and older in different geographic regions of China overall and by the risk of fracture (low, medium or high) as assessed by OSTA. Secondary objectives were to examine the risk factors for vitamin D deficiency and to estimate the relationship between serum 25(OH)D and iPTH levels. An exploratory objective was set to estimate the correlation of serum 25(OH)D with bone turnover markers β-CTX and P1NP levels.
Vitamin D insufficiency was defined as serum 25(OH)D < 30 ng/mL; vitamin D deficiency was defined as serum 25(OH)D < 20 ng/ml and < 15 ng/mL (1, 3, 10). Osteoporosis was defined as a BMD T-score ≤ -2.5 at any anatomical site; osteopenia was defined as a BMD T-score between −2.5 and −1.0 (22). Fracture risk was stratified as low (>-1), medium (−1 to −4), or high (< -4) as calculated based on body weight and age formulated by OSTA (20).
Sample Size and Statistical Analysis
Based on the literature (13–18), a prevalence estimate of 50% for vitamin D deficiency was used for sample size consideration. Assuming a 5% precision as expressed by a 95% confidence interval (CI) of the point estimate and a 10% discontinuation rate, a sample size of 424 postmenopausal women was needed. In order to evaluate residential (rural vs. urban) and seasonal (summer vs. winter) differences, the above sample size was quadrupled to a total of ~1,680.
Descriptive statistics were used to address the primary objective. Distribution of vitamin D levels was analyzed and presented categorically as the proportion and corresponding 95%CI of vitamin D inadequacy as defined and numerically as the mean ± SD (SE) for serum vitamin D levels among all subjects whose serum 25(OH)D were measured. The primary analysis was also performed in subjects stratified by fracture risk level as assessed by OSTA, and grouped by region, residence and season. A post-hoc Chi-Square test was used to compare the prevalence of low vitamin D status among subgroups whenever applicable. Univariate and multivariate logistic regression analyses were applied to identify risk factors for vitamin D deficiency. Results were represented as odds ratio (OR) with corresponding 95% CI and P-value. In multivariate logistic regression, variables including latitude, travel to the sunny area and walking outside were excluded due to collinearity with sunlight exposure. All selected variables from univariate analysis retained in the multivariate model presented by adjusted OR with corresponding 95%CI and P-value. In terms of the relationship between 25(OH)D and iPTH, Pearson's correlation coefficient was performed. Levels of iPTH were plotted against serum 25(OH)D to assess any relationship between the two values. A quadratic fit model with plateau was used to evaluate the association between serum 25(OH)D and PTH levels (18). In addition, the association between serum 25(OH)D and bone turnover markers ß-CTx and P1NP was explored by using univariate linear regression analysis. Clinical and biochemical variables including age, BMI, iPTH, and years since menopause were fit into the model. Analysis of variance (ANOVA) was used to compare the mean levels of β-CTx and P1NP in different subgroups categorized by serum 25(OH)D levels.
For demographics and clinical data, descriptive statistics were made to display the results. Chi-square or t-test was used to test the statistical significance for categorical or continuous variables wherever appropriate. There was no imputation for missing data in terms of 25(OH)D or other variables. All statistical analyses were performed using SAS 9.3 (SAS Institute, Cary, NC, USA) and a P-value of 0.05 was considered statistically significant unless otherwise specified.
Results
Subject Enrollment and Characteristics
The study recruited a total of 1,713 women from 7 regions in China, among which 25 women had screening failure and therefore, 1,688 subjects were included in the study analysis (Figure 1). Of those eligible, 1,684 postmenopausal women had 25(OH)D levels measured whereas four women did not complete the blood sampling procedure.
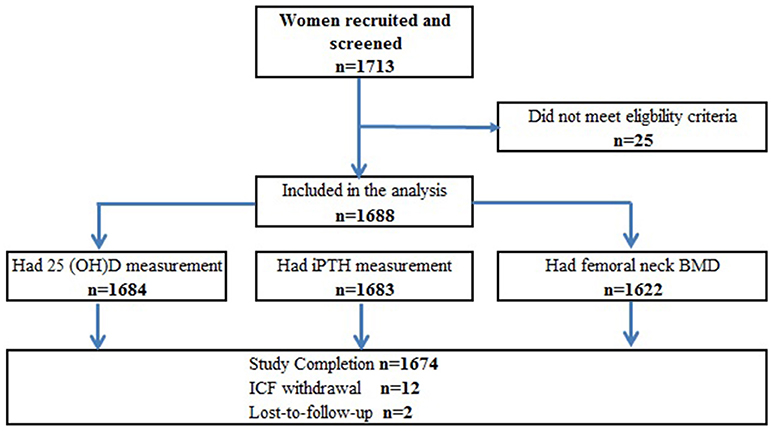
Figure 1. Study flowchart for enrolment. Four subjects had 25(OH)D < LLoQ and were not included in the analysis for the continuous variable. Subjects who had missing femoral neck DXA may have BMD measured at another anatomical site. Study completion was deemed as subjects who had all study procedures as per protocol. Subjects failed to return for the remained study procedure were deemed lost-to-follow-up. All subjects with non-missing data were included in the corresponding analysis.
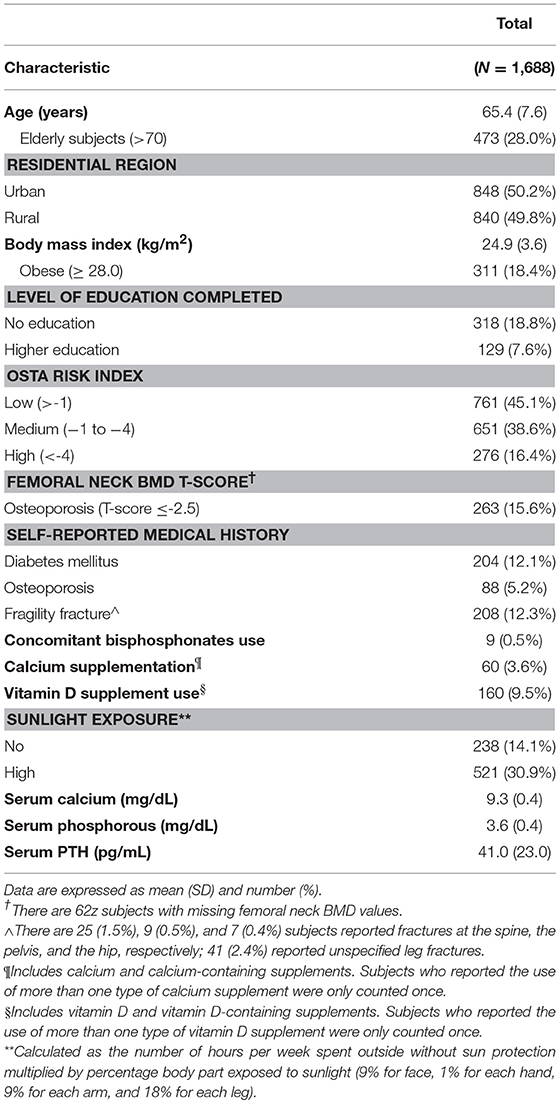
Results of the subject's characteristics are shown in Table 1. The subjects' mean (SD) age was 65.4 (7.6) years. Women who were elderly (>70 years) and obese accounted for 28.0, 3.6%, respectively, in the analyzed population. The proportion of women who had a high fracture risk as assessed by OSTA was 16.4% (276/1,688) in the analyzed population. There were 208 women (12.3%) reported fragility fractures, among which 25 (1.5%), 9 (0.5%), and 7 (0.4%) subjects had fractures at the spine, the pelvis, and the hip, respectively. Very few postmenopausal women used concomitant bisphosphonates [0.9% (9/1,688)] or calcium-containing supplements [3.6% (60/1,688)] in the study. Of all included subjects, 9.5% (160/1,688) had vitamin D supplementation and 30.9% (521/1,688) had high sunlight exposure. Subjects' mean serum calcium, phosphorus and PTH levels were within the normal ranges.
Serum 25(OH)D Distribution and Vitamin D Inadequacy
Among all subjects with quantified 25(OH)D levels, the mean (SD) serum 25(OH)D was 18.0 (8.4) ng/ml. Mean serum 25(OH)D levels appeared comparable among geographic regions but were significantly higher in women who were enrolled in the summer as compared that in those who were enrolled in the winter within each region and overall (all P < 0.0001). A numerically higher mean serum 25(OH)D value was observed among rural residents compared to urban residents (mean difference ~1.3 ng/mL), which remained consistent across the regions, except for the Northwest and Southwest regions where higher mean serum 25(OH)D levels were observed in urban residents. Data on mean serum 25(OH)D levels by season and by residential region are displayed in Supplementary Table 1 and Supplementary Figure 2, respectively.
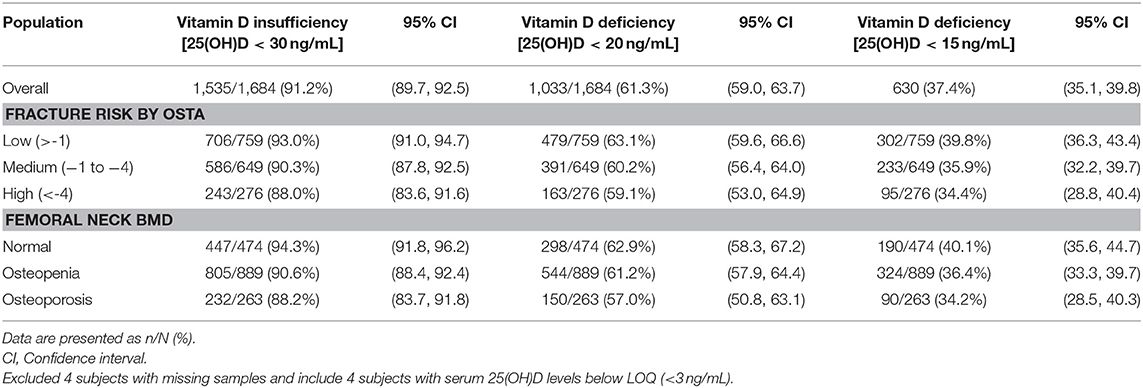
Table 2 presents the prevalence of vitamin D inadequacy as defined by different cutoff values overall and in subjects grouped by fracture risk assessed by OSTA and by osteoporosis measured by DXA. Vitamin D insufficiency, defined as 25(OH)D < 30 ng/mL, was 91.2% (1,535/1,684, 95%CI: 89.7, 92.5%) among all included subjects; vitamin D deficiency, defined as 25(OH)D < 20 or 15 ng/mL, was 61.3% (1,033/1,684, 95%CI: 59.6, 63.7%), 37.4% (630/1,684, 95%CI: 35.1, 39.8%), respectively, among all included subjects. Rates of vitamin D insufficiency and deficiency did not differ among various groups categorized by fracture risks or densitometric osteoporosis and were generally similar to those in the overall studied population.
The prevalence of vitamin D insufficiency or deficiency was significantly lower in women who enrolled in the summer, compared to those who enrolled in the winter (all P < 0.01, 41.3 vs. 84.7% for serum 25(OH)D < 20 ng/mL, Figure 2A). A statistically significant difference in the prevalence of serum 25(OH)D inadequacy defined by different 25(OH)D cutoffs was seen between rural and urban dwellers enrolled in the summer (all P < 0.01, 46.8 vs. 35.7% for serum 25(OH)D < 20 ng/mL, Figure 2B). Cumulative distribution curves of serum 25(OH)D levels by region and season (summer and winter) are shown in Supplementary Figure 3. Regional variation in the prevalence of vitamin D inadequacy was more distinct in the summer than that in the winter.
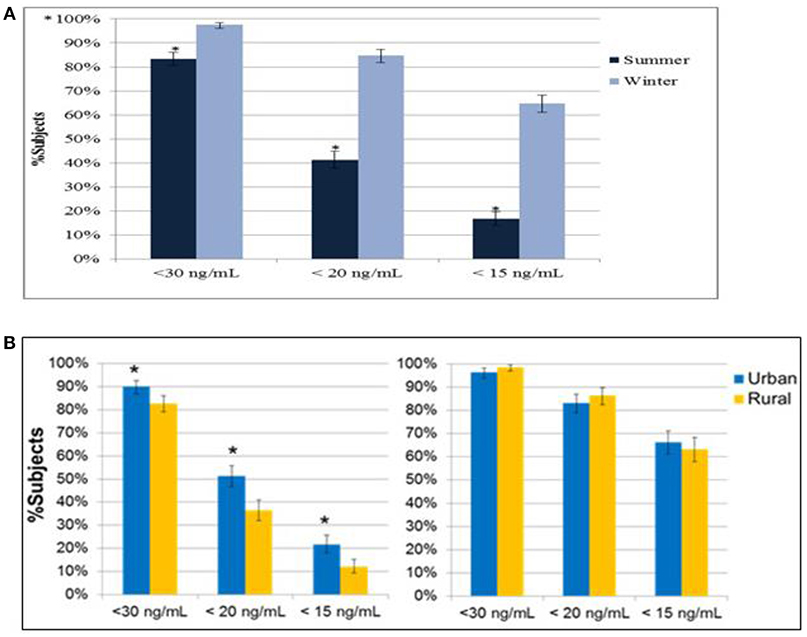
Figure 2. (A) Prevalence of vitamin D inadequacy by season. *P < 0.01 from Chi-square test of the comparison of summer vs. winter subjects. (B) Prevalence of vitamin D inadequacy in urban and rural dwellers. *P < 0.01 from Chi-square test of the comparison of urban vs. rural dwellers.
Risk Factors for Vitamin D Deficiency
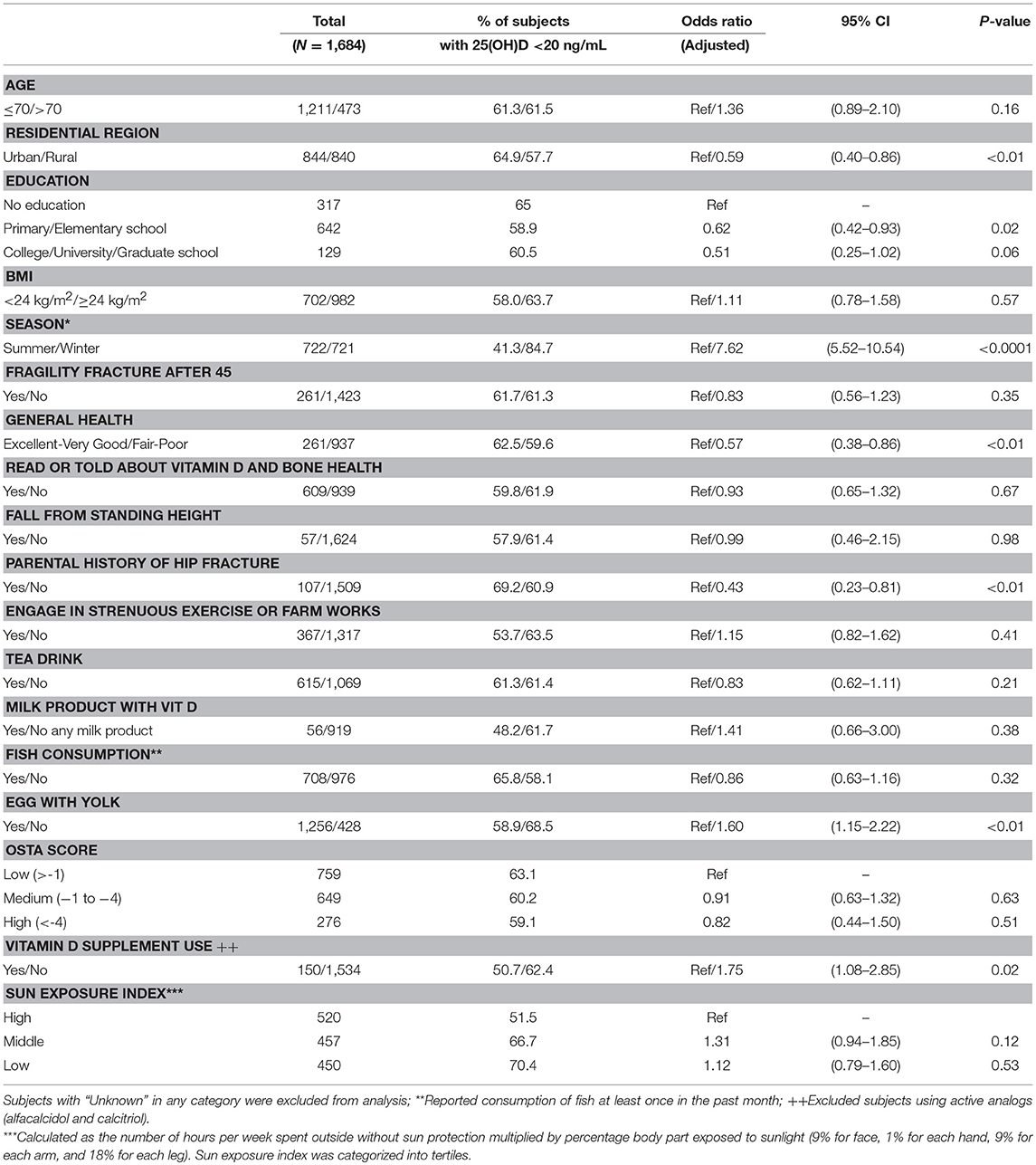
The subject's demographic, lifestyle and clinical characteristics were analyzed individually to explore factors associated with vitamin D deficiency defined as serum 25(OH)D < 20 ng/ml by using univariate logistic regression (Supplementary Table 2). Overweight, region (Northwest, North, and Southwest), winter season, no exercise, no milk products or fish consumption, no vitamin D supplement, and no or low sunlight exposure were individual factors significantly associated with an increased risk of vitamin D deficiency (ORs between 1.28 and 7.90, all P < 0.05). Notably, a high fracture risk assessed by OSTA or densitometric osteoporosis was not associated with vitamin D deficiency.
A multivariate logistic regression model was established to explore the likelihood of vitamin D deficiency presented by adjusted OR by accommodating all variables analyzed in single logistic regression (Table 3). Variables with collinearity including latitude, travel to the sunny area and walking outside were excluded from the model analysis, as sunlight exposure was retained. Rural dwellers were less likely to have vitamin D deficiency (adjusted OR: 0.59, 95%CI: 0.40, 0.86, P < 0.01); women enrolled in the winter season had a 7.62-fold likelihood of having vitamin D deficiency as compared with those who were enrolled in the summer season (adjusted OR: 7.62, 95%CI: 5.52, 10.54, P < 0.0001); women with no vitamin D use had a 1.75-fold higher relative risk for vitamin D deficiency (adjusted OR: 1.75, 95%CI: 1.08. 2.85, P = 0.02); women who reported fair/poor health or no parental fractures had a relatively lower risk of vitamin D deficiency (P < 0.01). Sunlight exposure and fracture risk level by OSTA appeared to have no statistically significant association with vitamin D deficiency as adjusted for other variables in the model.
Relationship of Serum 25(OH)D to PTH, β-CTX, and P1NP
Figure 3A suggested changes of iPTH levels over serum 25(OH)D intervals in 1679 subjects with quantified iPTH and 25(OH)D. A significant inverse correlation between serum iPTH and 25(OH)D was observed (r = −0.21, p < 0.01). The relationship between these two parameters was further analyzed by using a quadratic fit with plateau model (Figure 3B). Serum iPTH levels reached a plateau at a serum 25(OH)D level by 16.78 ng/ml, suggesting that the observed inverse relationship occurred below this cutoff value and iPTH remained stable for serum 25(OH)D above the cutoff.
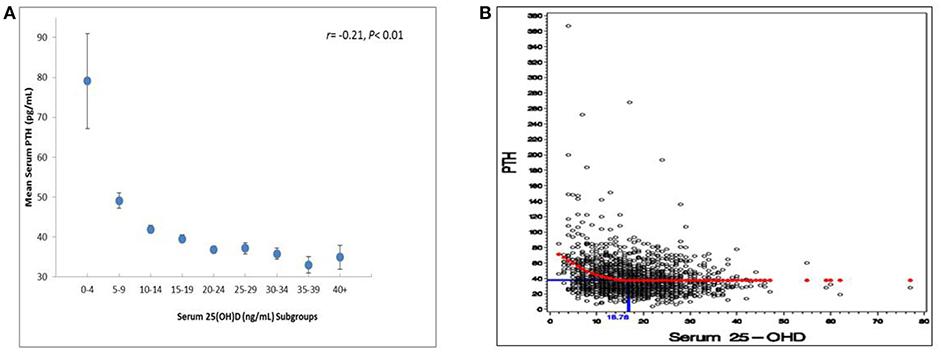
Figure 3. (A) Relationship between serum 25(OH)D and serum PTH levels (N = 1,679). Subjects with serum 25(OH)D levels >50 ng/ml were excluded (n = 4 summer and n = 1 winter). (B) Applied quadratic fit with plateau model to predict iPTH cutoff for 25(OH)D trends. Subjects with serum 25(OH)D levels >50 ng/ml were excluded (n = 4 summer and n = 1 winter).
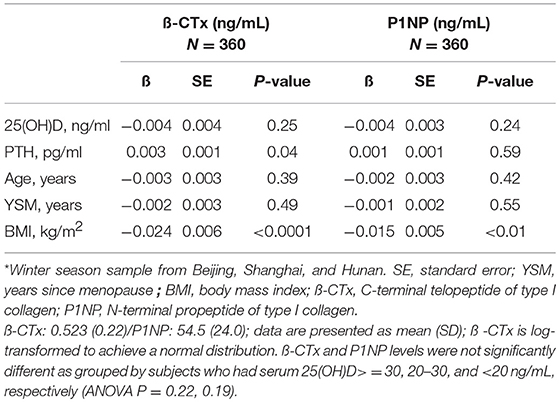
A study subset of 360 women enrolled in the winter season from 3 geographic regions underwent the measurement of serum ß-CTx and serum P1NP. Univariate linear regression analysis showed that serum iPTH was significantly associated with serum ß-CTx (ß = 0.003, P = 0.04) but not P1NP (ß = 0.001, P = 0.59); BMI was inversely associated with serum ß-CTx (ß = −0.024, P < 0.0001) and P1NP (ß = −0.015, P < 0.01). In women grouped as 25(OH)D ≥30, 20–30, and < 20 ng/ml, respectively, neither ß-CTx nor P1NP differed significantly based on the analysis of variance (P = 0.22, P = 0.19), Table 4.
Discussion
Findings from this multicenter, cross-sectional study in China suggested a considerable prevalence of vitamin D inadequacy among postmenopausal women from different geographic regions across the country. Although fracture risk level assessed by OSTA did not impact significantly on vitamin D status, urban dwelling, and the winter season contributed to lower 25(OH)D levels and were the associated risk factors on vitamin D deficiency among the analyzed population. In addition, our analyses did not show a curvilinear relationship between serum iPTH and serum 25(OH)D.
This study is among the few epidemiological studies to investigate serum 25(OH)D status using the standard LC-MS/MS assay in a large, geographically diverse population in China and Southeast Asia. The study compared serum 25(OH)D levels and prevalence rates in various scenarios including the season, residence location, and geographic region. The study well defined non-institutionalized postmenopausal women and obtained potential participant lists from the community. All blood samples were taken at the coordinating sites and sent to a central laboratory for further determination. Therefore, inter-laboratory variations were diminished and comparison with external study results can be realized and underestimation of 25(OH)D levels may be lessened (23).
Nevertheless, this study has limitations. The interview-based questionnaire caused the subject's recall bias on self-reporting events including fracture history and use of health supplements. DXA quality control was not done centrally which may cause measurement variations on BMD. Due to a cross-sectional design, a snapshot of the disease status at a certain time is given. The incident hypovitaminosis D over time cannot be assessed and causality cannot be inferred between suboptimal vitamin D and risk factors. The investigators recruited community and village women; however, a randomized sampling method was not performed to minimize selection bias. The study cannot be considered a strict population-based research and therefore, findings may not be generalizable to all postmenopausal women in China.
The prevalence of low serum 25(OH)D varies by region, population, and cutoff value used for hypovitaminosis D. Worldwide investigations (24) suggested prevalence of vitamin D deficiency [25(OH)D<20 ng/mL] was 8–57% in Caucasians and 2–70% in Southeast Asians across different age groups. Higher prevalence rates of hypovitaminosis D were seen in children, pregnant women and elderly people including postmenopausal women (24), or if 25(OH)D<30 ng/mL is used as cutoff (1). Among postmenopausal Caucasians, a study reported that hypovitaminosis D [defined 25(OH)D < 30 ng/mL, < 20 ng/mL] was 52, 18%, respectively, in North American elderly women who received concomitant bisphosphonates (21). A mean serum 25(OH)D of 30.4 ng/ml was observed. Numerically higher prevalence rates were found in Europe. In a large study on 8,532 postmenopausal subjects, the prevalence of 25(OH)D inadequacy (defined as 25(OH)D < 50 ng/mL, < 80 ng/mL) was 32.1 and 79.6%, respectively (25), and a mean serum 25(OH)D level of 27.2 ng/mL was observed. In a systematic review of 36 published studies (26), the prevalence of vitamin D deficiency [serum 25(OH) < 20 ng/ml)] ranged from 1.6 to 86% among community-living and institutionalized postmenopausal women, and a higher prevalence was seen in women with osteoporosis (12.5–76%) or with a history of fracture (50–70%) by using lower cutoff values in defining hypovitaminosis D. Our study, however, suggested a considerably higher prevalence of suboptimal vitamin D among Chinese postmenopausal women [25(OH)D < 30 ng/mL: 91.2%, 25(OH)D < 20 ng/mL: 61.3%], which was supported by a few published studies from East Asian regions (89.7, 72.1% in Beijing and central south China, and 65.0% in Korea] (13, 16, 27), and South Asia (>70% across different age groups in India) (28). It is difficult to directly compare attributable socioeconomic and lifestyle factors among populations. Differences in hypovitaminosis D in Caucasians and Chinese may be explained at the study level, including recruitment strategy, population sampling or assay method. As a low proportion (9.5%) of women in our study had vitamin D supplementation, hypovitaminosis D would be unsurprisingly frequent. Based on observational studies and randomized trials (1, 29), a serum 25(OH)D level of 20 ng/mL was shown to protect most people against bone-related events such as fractures and falls. Screening vitamin D deficiency and prescribing vitamin D supplements need more clinical attention in Chinese postmenopausal women.
Vitamin D is critical for bone mineralization. There has so far been no robust evidence on skeletal benefits associated with 25(OH)D levels based on pooled analyses on observational studies (30, 31). Moreover, the association of vitamin D with BMD and osteoporosis remains controversial. Several studies have shown that 25(OH)D is positively correlated with BMD (32–35) when 25(OH)D levels are low (36), whereas no such an association has been found in other studies (37–39). In our study, vitamin D inadequacy was not associated with higher fracture risk as assessed by OSTA or densitometric osteoporosis. Further, there was no statistically significant difference in bone turnover markers including ß-CTx and P1NP among a subset of subjects grouped by 25(OH)D interval from three geographic regions. Results must be interpreted with caution as very few women had bisphosphonates in addition to a low proportion of vitamin D or calcium supplementation. Another interesting finding is the lack of correlation between vitamin D insufficiency and fragility fracture prevalence. The subject's self-reporting on fragile fractures was prone to bias and thus, limited the precision in the analysis of association between these two morbidities. The prevalence of fragile fractures was low and major fragile fractures were very few, compared with previous reports (40). Results might not be generalizable even if this small cohort had more vitamin D supplementation or markedly lower vitamin D levels than those among most women in the study. For risk factors on fragile fractures in Chinese postmenopausal women, no sufficient evidence has been generated so far. Our study focused on risk factors for hypovitaminosis, but some results might be interpreted to link the lower prevalence of major fragile fractures. We recruited women who were relatively younger and had higher BMI, lower proportion of high OSTA or osteoporosis, and infrequent falls. These clinically meaningful factors have an association with fragile fractures, as supported by treatment guidelines (41, 42). Our study did not analyse the association between fragile fractures and fracture risk assessment (BMD or OSTA). However, results suggested an observed parallel trend among these clinical parameters. A lower proportion of women with densitometric osteoporosis or OSTA high risk was consistent with fewer fragile fractures. Findings indicated the primary role of BMD or OSTA in the screening of patients with high fracture risks among Chinese postmenopausal women, albeit further evidence needed.
Vitamin D levels may be affected by a number of factors including age, cultural behavior, latitude and season, and outdoor activity (24). Our subgroup analyses suggested the prevalence of hypovitaminosis D was significantly higher in women enrolled in the winter, and in women living in the urban community, respectively. Adjusted for all variables in the multivariate logistic model, urban dwelling, winter season, parental history of hip fracture, no consumption of eggs with yolks, and lack of vitamin D supplement was found to have a significant association with vitamin D deficiency among postmenopausal women. The study did not include smoking as a lifestyle factor in the study analysis, because we considered a very low proportion of subjects who smoke. Influence of occupation on vitamin D levels were measured as “engage in strenuous exercise or farm works” and “sun exposure index” as potential risk factors in the multivariate logistic model. As expected, season and residence location were major factors affecting vitamin D status. Latitude, however, was not a substantial influence. No prevalence gradient of vitamin D deficiency by latitude was observed, although rates varied by region (ranging from 50 to 71.3%). Similarly, one recent population-based study on 33 Chinese healthy adults suggested vitamin D deficiency was independent of latitude changes (43). These results suggested that there might be factors other than distance to the equator affect vitamin D status among Chinese postmenopausal women.
Our data indicate that the relationship between iPTH and 25(OH)D is not curvilinear, similar to previous studies. An inverse correlation between these two parameters was seen but iPTH levels remained stable in women who had 25(OH)D at 16.78 ng/mL or above. Historically, the normal lower limit of 25(OH)D was set at 30 ng/mL because PTH levels rise as 25(OH)D falls below this threshold, along with optimal calcium absorption (1, 44). In addition, the rationale for such a threshold extended to extra-skeletal benefits including cancer prevention (45). Recent osteoporosis guidelines have also suggested the optimum level of 25(OH)D is 30 ng/mL or above (41, 42). On the contrary, the IOM indicated that 20 ng/mL is appropriate for at least 97.5% of population (16 ng/mL for 50% of population) to maintain bone health as regulated by calcium and PTH status (46). A most recent trial has demonstrated ineffectiveness of maintaining vitamin D 30 mg/mL to cancer prevention in women >55 years of age (47). In the present study, the 25(OH)D threshold for such a rationale was 16.78 ng/mL, although calcium absorption was not possible to measure. A few studies in Chinese (48) and African (49) populations revealed very similar vitamin D levels (17–19 ng/mL) for PTH stability. The existing literature brings concerns the current cut-off for vitamin D deficiency among Chinese postmenopausal women. In terms of 25(OH)D < 20 ng/mL, a majority of women were vitamin D deficient and thus the use of vitamin D supplements was far from satisfactory, which is similar to other countries or regions. However, the proportion of vitamin D deficiency was dramatically lower when 25(OH)D < 15 ng/mL was used for the definition (61.3 vs. 37.4%). Although there is no consensus, there may be a reason to tune down 25(OH)D levels in the clinical setting. Future endeavors can be made to confirm optimal vitamin D status managed by diet intake and nutrient supplementation in relation to skeletal outcomes for this indicated population.
In conclusion, the prevalence of vitamin D inadequacy was remarkable among Chinese postmenopausal women and was independent of fracture risk assessed by OSTA or osteoporosis suggested by DXA. Winter season, urban residence, however not latitude, were significantly associated with a higher likelihood of vitamin D deficiency. Optimal vitamin D status for iPTH and bone-related outcomes merits further investigation in this population.
Author Contributions
ZX, WX, ST, JG, JC, SP, TW, and EL conceived and designed research. ZX, WX, WW, ZZ, CL, LW, TW, and EL collected data and conducted research. ZX, WX, ZZ, CL, JC, SP, and TW analyzed and interpreted data. ZX, WW, ST, SP, and TW wrote the initial paper. ZX, WX, CL, LW, JG, JC, SP, HY, and EL revised the paper. EL had primary responsibility for final content. All authors read and approved the final manuscript.
Funding
This study was funded by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. The medical writing was funded by MSD China and was prepared by Madjaden Bioscience and Dr. Jue Wang, Global Medical Affairs, MSD China.
Conflict of Interest Statement
JC, SP, HY, and TW were employees of MSD at the time of study conduct and analysis.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer XY declared a shared affiliation, with no collaboration, with one of the authors CL to the handling editor.
Acknowledgments
The authors would like to thank all subjects, investigators, and study personnel who participated in this study. The investigators who contributed to the study were: Dr. Houde Zhou and Dr. Zhifeng Sheng. Study personnel who contributed to the study included: Xingshu Zhu and Tengfei Man. We would also like to thank the National Natural Science Foundation of China (81072219, 81272973, 81471055, and 81672646) for the support.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2018.00782/full#supplementary-material
Supplementary Table 1. Mean serum 25(OH)D (ng/mL) by overall, region and season.
Supplementary Table 2. Univariate analysis on relative risk for vitamin D deficiency (< 20 ng/mL).
Supplementary Figure 1. Distribution of enrolled subjects by province and region. *Subjects were enrolled from urban and rural areas in seven provinces located in seven different geographic regions of China.
Supplementary Figure 2. Mean serum 25(OH)D levels by residential region. Rural residents had a higher mean serum 25(OH)D level as compared with urban residents, which remained consistent across the regions, except for the Northwest and Southwest regions where higher mean serum 25(OH)D levels were observed in urban residents.
Supplementary Figure 3. Cumulative distribution for serum 25(OH)D overall and by region. Cumulative distribution curves of serum 25(OH)D levels by region and season (summer and winter) are displayed. Regional variation in the distribution of serum 25(OH)D was more distinct in the summer compared to the winter when the distributions for all regions were more similar to the overall distribution. Lower serum 25(OH)D was observed in the North and Southwest regions in both the summer and winter.
References
1. Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. (2011) 364:248–54. doi: 10.1056/NEJMcp1009570
2. Cashman KD, Hill TR, Cotter AA, Boreham CA, Dubitzky W, Murray L, et al. Low vitamin D status adversely affects bone health parameters in adolescents. Am J Clin Nutr. (2008) 87:1039–44. doi: 10.1093/ajcn/87.4.1039
3. Wimalawansa SJ. Vitamin D in the new millennium. Curr Osteoporos Rep. (2012) 10:4–15. doi: 10.1007/s11914-011-0094-8
4. Bolland MJ, Bacon CJ, Horne AM, Mason BH, Ames RW, Wang TK, et al. Vitamin D insufficiency and health outcomes over 5 y in older women. Am J Clin Nutr. (2010) 91:82–9. doi: 10.3945/ajcn.2009.28424
5. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. (2008) 87:1080S−6S. doi: 10.1093/ajcn/87.4.1080S
6. Zittermann A, Iodice S, Pilz S, Grant WB, Bagnardi V, Gandini S. Vitamin D deficiency and mortality risk in the general population: a meta-analysis of prospective cohort studies. Am J Clin Nutr. (2012) 95:91–100. doi: 10.3945/ajcn.111.014779
7. Akkermans MD, van der Horst-Graat JM, Eussen SR, van Goudoever JB, Brus F. Iron and vitamin D deficiency in healthy young children in Western Europe despite current nutritional recommendations. J Pediatr Gastroenterol Nutr. (2016) 62:635–42. doi: 10.1097/MPG.0000000000001015
8. Cashman KD, Dowling KG, Skrabakova Z, Gonzalez-Gross M, Valtuena J, De Henauw S, et al. Vitamin D deficiency in Europe: pandemic? Am J Clin Nutr. (2016) 103:1033–44. doi: 10.3945/ajcn.115.120873
9. Nimitphong H, Holick MF. Vitamin D status and sun exposure in southeast Asia. Dermatoendocrinology (2013) 5:34–7. doi: 10.4161/derm.24054
10. Rosen CJ, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, et al. IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab. (2012) 97:1146–52. doi: 10.1210/jc.2011-2218
11. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. (2011) 96:1911–30. doi: 10.1210/jc.2011-0385
12. Foo LH, Zhang Q, Zhu K, Ma G, Trube A, Greenfield H, et al. Relationship between vitamin D status, body composition and physical exercise of adolescent girls in Beijing. Osteoporos Int. (2009) 20:417–25. doi: 10.1007/s00198-008-0667-2
13. Li S, Ou Y, Zhang H, Zhang Z, Zhou H, Liu L, et al. Vitamin D status and its relationship with body composition, bone mineral density and fracture risk in urban central south Chinese postmenopausal women. Ann Nutr Metab. (2014) 64:13–9. doi: 10.1159/000358340
14. Lu HK, Zhang Z, Ke YH, He JW, Fu WZ, Zhang CQ, et al. High prevalence of vitamin D insufficiency in China: relationship with the levels of parathyroid hormone and markers of bone turnover. PLoS ONE (2012) 7:e47264. doi: 10.1371/journal.pone.0047264
15. Xiang F, Jiang J, Li H, Yuan J, Yang R, Wang Q, et al. High prevalence of vitamin D insufficiency in pregnant women working indoors and residing in Guiyang, China. J Endocrinol Invest. (2013) 36:503–7. doi: 10.3275/8814
16. Zhao J, Xia W, Nie M, Zheng X, Wang Q, Wang X, et al. The levels of bone turnover markers in Chinese postmenopausal women: Peking Vertebral Fracture study. Menopause (2011) 18:1237–43. doi: 10.1097/gme.0b013e31821d7ff7
17. Zhen D, Liu L, Guan C, Zhao N, Tang X. High prevalence of vitamin D deficiency among middle-aged and elderly individuals in northwestern China: its relationship to osteoporosis and lifestyle factors. Bone (2015) 71:1–6. doi: 10.1016/j.bone.2014.09.024
18. Zhu H, Gan J, Du Y, Hong W, Li H, Cheng Q, et al. Vitamin D status in healthy men and women in Shanghai. Bone (2010) 47:S447–S448. doi: 10.1016/j.bone.2010.09.308
19. Galior K, Ketha H, Grebe S, Singh RJ. 10 years of 25-hydroxyvitamin-D testing by LC-MS/MS-trends in vitamin-D deficiency and sufficiency. Bone Rep. (2018) 8:268–73. doi: 10.1016/j.bonr.2018.05.003
20. Koh LK, Sedrine WB, Torralba TP, Kung A, Fujiwara S, Chan SP, et al. A simple tool to identify asian women at increased risk of osteoporosis. Osteoporos Int. (2001) 12:699–705. doi: 10.1007/s001980170070
21. Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, et al. Prevalence of Vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab. (2005) 90:3215–24. doi: 10.1210/jc.2004-2364
22. World Health Organisation. Assessment of Fracture Risk and Its Implication to Screening for Postmenopausal Osteoporosis: Technical Report Series 843. Geneva: WHO (1994).
23. Li L, Zeng Q, Yuan J, Xie Z. Performance evaluation of two immunoassays for 25-hydroxyvitamin D. J Clin Biochem Nutr. (2016) 58:186–92. doi: 10.3164/jcbn.15-61
24. Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, et al. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. (2009) 20:1807–20. doi: 10.1007/s00198-009-0954-6
25. Bruyere O, Malaise O, Neuprez A, Collette J, Reginster JY. Prevalence of vitamin D inadequacy in European postmenopausal women. Curr Med Res Opin. (2007) 23:1939–44. doi: 10.1185/030079907X219562
26. Gaugris S, Heaney RP, Boonen S, Kurth H, Bentkover JD, Sen SS. Vitamin D inadequacy among post-menopausal women: a systematic review. QJM (2005) 98:667–76. doi: 10.1093/qjmed/hci096
27. Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, et al. Vitamin D insufficiency in Korea–a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab. (2011) 96:643–51. doi: 10.1210/jc.2010-2133
28. Babu US, Calvo MS. Modern India and the vitamin D dilemma: evidence for the need of a national food fortification program. Mol Nutr Food Res. (2010) 54:1134–47. doi: 10.1002/mnfr.200900480
29. Manson JE, Brannon PM, Rosen CJ, Taylor CL. Vitamin D deficiency - is there really a pandemic? N Engl J Med. (2016) 375:1817–20. doi: 10.1056/NEJMp1608005
30. Chung M, Balk E, Brendel M. Vitamin D and Calcium: A Systematic Review of Health Outcomes. Evidence report/technology assessment no. 183. Rockville, MD: Agency for Healthcare Research and Quality (2009).
31. Cranney A, Horsley T, O'Donnell S. Effectiveness and Safety of Vitamin D in Relation to Bone Health. Evidence report/technology assessment no. 158. Rockville, MD: Agency for Healthcare Research and Quality (2007).
32. Ardawi MS, Qari MH, Rouzi AA, Maimani AA, Raddadi RM. Vitamin D status in relation to obesity, bone mineral density, bone turnover markers and vitamin D receptor genotypes in healthy Saudi pre- and postmenopausal women. Osteoporos Int. (2011) 22:463–75. doi: 10.1007/s00198-010-1249-7
33. Fradinger EE, Zanchetta JR. Vitamin D and bone mineral density in ambulatory women living in Buenos Aires, Argentina. Osteoporos Int. (2001) 12:24–7. doi: 10.1007/s001980170153
34. Mezquita-Raya P, Munoz-Torres M, Luna JD, Luna V, Lopez-Rodriguez F, Torres-Vela E, et al. Relation between vitamin D insufficiency, bone density, and bone metabolism in healthy postmenopausal women. J Bone Miner Res. (2001) 16:1408–15. doi: 10.1359/jbmr.2001.16.8.1408
35. Nakamura K, Tsugawa N, Saito T, Ishikawa M, Tsuchiya Y, Hyodo K, et al. Vitamin D status, bone mass, and bone metabolism in home-dwelling postmenopausal Japanese women: Yokogoshi Study. Bone (2008) 42:271–7. doi: 10.1016/j.bone.2007.09.056
36. Bischoff-Ferrari HA, Dietrich T, Orav EJ, Dawson-Hughes B. Positive association between 25-hydroxy vitamin D levels and bone mineral density: a population-based study of younger and older adults. Am J Med. (2004) 116:634–9. doi: 10.1016/j.amjmed.2003.12.029
37. Garnero P, Munoz F, Sornay-Rendu E, Delmas PD. Associations of vitamin D status with bone mineral density, bone turnover, bone loss and fracture risk in healthy postmenopausal women. OFELY Study Bone (2007) 40:716–22. doi: 10.1016/j.bone.2006.09.026
38. Hosseinpanah F, Rambod M, Hossein-nejad A, Larijani B, Azizi F. Association between vitamin D and bone mineral density in Iranian postmenopausal women. J Bone Miner Metab (2008) 26:86–92. doi: 10.1007/s00774-007-0791-7
39. Tsai KS, Hsu SH, Cheng JP, Yang RS. Vitamin D stores of urban women in Taipei: effect on bone density and bone turnover, and seasonal variation. Bone (1997) 20:371–4. doi: 10.1016/S8756-3282(97)00010-0
40. Xia WB, He SL, Xu L, Liu AM, Jiang Y, Li M, et al. Rapidly increasing rates of hip fracture in Beijing, China. J Bone Miner Res. (2012) 27:125–9. doi: 10.1002/jbmr.519
41. Camacho PM, Petak SM, Binkley N, Clarke BL, Harris ST, Hurley DL, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis - 2016. Endocr Pract. (2016) 22:1–42. doi: 10.4158/EP161435.GL
42. Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. (2014) 25:2359–81. doi: 10.1007/s00198-014-2794-2
43. Yu S, Fang H, Han J, Cheng X, Xia L, Li S, et al. The high prevalence of hypovitaminosis D in China: a multicenter vitamin D status survey. Medicine (Baltimore) (2015) 94:e585. doi: 10.1097/MD.0000000000000585
44. Steingrimsdottir L, Gunnarsson O, Indridason OS, Franzson L, Sigurdsson G. Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intake. JAMA (2005) 294:2336–41. doi: 10.1001/jama.294.18.2336
45. Manson JE, Bassuk SS, Lee IM, Cook NR, Albert MA, Gordon D, et al. The VITamin D and OmegA-3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials (2012) 33:159–71. doi: 10.1016/j.cct.2011.09.009
46. Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. (2011) 96:53–8. doi: 10.1210/jc.2010-2704
47. Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N Engl J Med. (2018). doi: 10.1056/NEJMoa1809944 [Epub ahead of print].
48. Li M, Lv F, Zhang Z, Deng W, Li Y, Deng Z, et al. Establishment of a normal reference value of parathyroid hormone in a large healthy Chinese population and evaluation of its relation to bone turnover and bone mineral density. Osteoporos Int. (2016) 27:1907–16. doi: 10.1007/s00198-015-3475-5
Keywords: vitamin D deficiency, postmenopausal women, winter, urban, intact parathyroid hormone
Citation: Xie Z, Xia W, Zhang Z, Wu W, Lu C, Tao S, Wu L, Gu J, Chandler J, Peter S, Yuan H, Wu T and Liao E (2019) Prevalence of Vitamin D Inadequacy Among Chinese Postmenopausal Women: A Nationwide, Multicenter, Cross-Sectional Study. Front. Endocrinol. 9:782. doi: 10.3389/fendo.2018.00782
Received: 30 September 2018; Accepted: 12 December 2018;
Published: 07 January 2019.
Edited by:
Giacomina Brunetti, Università degli Studi di Bari, ItalyReviewed by:
Luca Pietrogrande, University of Milan, ItalyXijie Yu, West China Hospital of Sichuan University, China
Copyright © 2019 Xie, Xia, Zhang, Wu, Lu, Tao, Wu, Gu, Chandler, Peter, Yuan, Wu and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eryuan Liao, bGlhb2VyeXVhbjA4MjIwMThAMTI2LmNvbQ==
Zhongjian Xie, emhvbmdqaWFuLnhpZUBvdXRsb29rLmNvbQ==
 Zhongjian Xie
Zhongjian Xie Weibo Xia2
Weibo Xia2