
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Endocrinol. , 25 May 2018
Sec. Clinical Diabetes
Volume 9 - 2018 | https://doi.org/10.3389/fendo.2018.00248
 Tarik Elhadd1,2
Tarik Elhadd1,2 Georgios Ponirakis3
Georgios Ponirakis3 Zeinab Dabbous2
Zeinab Dabbous2 Mashhood Siddique2
Mashhood Siddique2 Subitha Chinnaiyan2
Subitha Chinnaiyan2 Rayaz A. Malik2,3*
Rayaz A. Malik2,3*
Background: Metformin may lead to B12 deficiency and neuropathy. There are no published data on the prevalence of Metformin-related B12 deficiency and neuropathy in the Arabian Gulf.
Aims: Determine whether Metformin intake is associated with B12 deficiency and whether B12 deficiency is associated with diabetic peripheral neuropathy (DPN) and painful diabetic neuropathy.
Methods: Patients with type 2 diabetes mellitus (T2DM) (n = 362) attending outpatient clinics at HMC underwent assessment of B12 levels, the DN4 questionnaire, and vibration perception threshold (VPT).
Results: Comparing Metformin to non-Metformin users there were no differences in B12 levels, VPT, or DN4. The prevalence of B12 deficiency (B12 <133 pmol/l) was lower (P < 0.01) in Metformin (8%) compared to non-Metformin (19%) users. Patients with B12 deficiency had a comparable prevalence and severity of sensory neuropathy and painful neuropathy to patients without B12 deficiency.
Conclusion: Serum B12 levels were comparable between Metformin and non-Metformin users with T2DM in Qatar. T2DM patients on Metformin had a lower prevalence of B12 deficiency. Furthermore, the prevalence and severity of neuropathy and painful diabetic neuropathy were comparable between patients with and without B12 deficiency.
Metformin remains first-line therapy in type 2 diabetes mellitus (T2DM), with around 120 million users worldwide. It is increasingly used in overweight T2DM patients and those with polycystic ovary syndrome (1). Most international guidelines recommend Metformin after lifestyle measures for T2DM patients.
Metformin therapy was shown to be associated with a significant reduction in the level of vitamin B12 over 50 years ago (2, 3). A number of observational and placebo-controlled studies have confirmed that Metformin may reduce vitamin B12 levels (4–10). Indeed a recent study from Pakistan found that 29.7% of patients on Metformin had B12 deficiency (11) and another study from Brazil showed that B12 deficiency occurred in 22.4% of patients with T2DM on Metformin, and was further reduced in those on proton pump inhibitors (PPI)/H2-antagonists (10). However, a recent meta-analysis showed that only 10/17 studies showed that Metformin use led to B12 deficiency and in four prospective studies B12 was reduced by approximately 57 pmol/L, within 6 weeks to 3 months of commencing Metformin (12).
A potential consequence of B12 deficiency is that it could directly result in neuropathy or exacerbate diabetic neuropathy. Indeed, the recent 2017 ADA position statement on diabetic neuropathy has emphasized the importance of excluding B12 deficiency in patients with diabetic neuropathy (13). However, there are conflicting reports on the association between Metformin-induced B12 deficiency and neuropathy, with some reports showing an association (14, 15) while others have refuted this (11, 16–18). Furthermore, in a recent study from Turkey, while the prevalence of B12 deficiency was 38.4% there was no difference in B12 levels in those with and without neuropathy (19). Despite this there is wide spread administration of vitamin B12 therapy in patients in the Middle East and Far East, with a recent analysis from five teaching hospitals in Jordan, indicating that cyanocobalamin (B12), was the second most common injectable therapy after insulin (20). There are no published data on Metformin-related B12 deficiency or the relationship between B12 deficiency and diabetic neuropathy in the MENA region.
We have compared vitamin B12 levels in outpatients with T2DM in Qatar, in relation to Metformin use and further assessed for the prevalence and severity of painful neuropathy and sensory neuropathy in patients with B12 deficiency.
Participants with T2DM (n = 362) were recruited from the National Diabetes & Endocrine Centers in Al-Wakra Hospital and Hamad General Hospital. The study was performed between March 6, 2017 and September 28, 2017.
Exclusion criteria included patients with a prior history of pernicious anemia, chronic kidney disease, previous bariatric surgery, gastrectomy, or small bowel resection for inflammatory bowel disease. This study was approved by the Institutional Review Board (IRB) of WCM-Q and HMC and all participants gave informed consent to take part in the study. The research adhered to the tenets of the declaration of Helsinki.
Data including age, duration of diabetes, blood pressure, body mass index (BMI), and medications including Metformin were recorded. HbA1c, lipid profile, renal function, and serum B12 were assessed.
Blood was drawn directly into a dedicated evacuated tube (BD Diagnostic—Preanalytical Systems, Oxford, UK) and centrifuged at 3,500 g for 10 min and serum analyzed immediately or stored at −20°C until analysis on Beckman Dxi 600 (Beckman Coulter Inc., Brea, CA, USA). The Vitamin B12 assay is a competitive-binding immunoenzymatic assay. The amount of analyte in the sample was determined by means of a stored, multipoint calibration curve (Beckman Coulter Assay Manual 2015, Beckman Coulter Inc., Brea, CA, USA). Analytical sensitivity <50 pg/ml, traceability; traceable to an internal standard manufactured using the purified cyanocobalamin. Assay precision: 4.8–11.4%. B12 levels <133 pmol/l were considered deficient.
Vibration perception threshold (VPT) was measured on the pulp of the large toe with a Neurothesiometer (Horwell, Scientific Laboratory Supplies, Wilford, Nottingham, UK). The test was repeated three times and the average value was recorded. VPT at a cutoff point ≥15V was defined as DPN (21).
The Douleur Neuropathique 4 (DN4) was used to identify neuropathic pain (22, 23). The DN4 is comprised of 10 questions (7 symptoms and 3 signs) and a score ≥4 identifies neuropathic pain with high sensitivity (83%) and specificity (90%) (24).
Variables were compared between groups using a t-test and χ2 test for continuous and categorical data, respectively. Data are expressed as mean (SD) of mean.
Univariate analysis by simple linear regression was applied to determine which variables are associated with B12 levels, VPT, and DN4 as outcome measures. Multiple linear regression analysis was used to determine the association between B12 levels, VPT, and DN4 after adjusting for confounding factors. Assumptions of linear regression were satisfied for normality, collinearity, and outliers. Additionally, residual plots were used to determine whether the models fit the assumptions.
All analyses were performed using StatsDirect version 3.0. A two-tailed P value of <0.05 was considered significant.
Age, systolic (SBP), BMI, HbA1c, triglycerides, HDL, and B12 levels were comparable between Metformin (n = 235) and non-Metformin users (n = 64). Metformin users had a shorter duration of diabetes (10.27 ± 7.45 vs 12.89 ± 8.89, P = 0.03), but higher diastolic blood pressure (DBP) (77.72 ± 9.91 vs 74.52 ± 9.42, P = 0.02), total cholesterol (4.48 ± 1.10 vs 4.15 ± 1.02, P = 0.03), and LDL (2.56 ± 0.88 vs 2.30 ± 0.82, P = 0.04). B12 levels were comparable between Metformin and non-Metformin users (P = 0.87). However, the prevalence of B12 deficiency was lower in Metformin (8%) compared to non-Metformin (19%) users, P < 0.01.
The prevalence of neuropathy (30 vs 39%) and neuropathic pain (31 vs 33%) were comparable between Metformin and non-Metformin users. The proportion of patients taking medications, which could influence B12 levels, including PPI, calcium supplements, multivitamins, B12 supplements, and sulfonylureas were comparable between Metformin and non-Metformin users (Table 1).
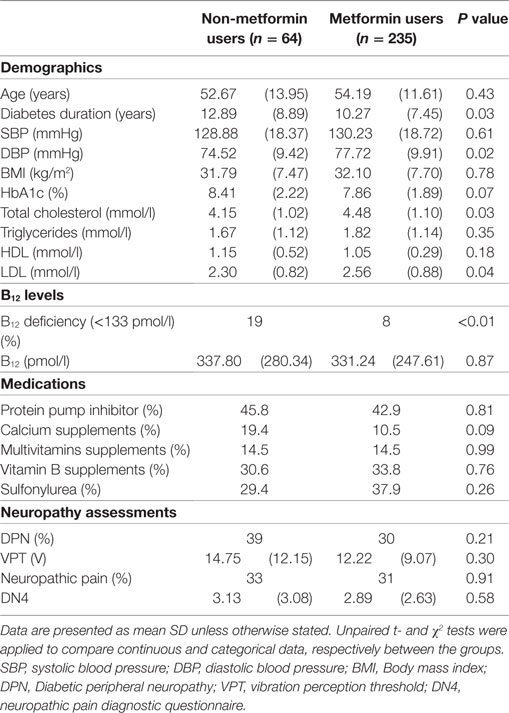
Table 1. Comparison of demographic and clinical characteristics between non-Metformin users and Metformin users.
Of the 362 T2DM patients, 32 (8.8%) fulfilled the criteria for B12 deficiency (serum B12 <133 pmol/l). However, in those with B12 deficiency, the percentage taking Metformin was significantly lower than in those without B12 deficiency (60 vs 80%, P = 0.03). Patients with B12 deficiency were significantly younger (49.16 ± 9.72 vs 54.56 ± 12.71, P = 0.01) and had a shorter duration of diabetes (7.03 ± 5.39 vs 11.68 ± 7.89, P < 0.001), but comparable SBP, DBP, BMI, HbA1c, cholesterol, triglycerides, HDL, and LDL. The prevalence and severity of neuropathy and neuropathic pain was comparable between those with and without B12 deficiency (Table 2).
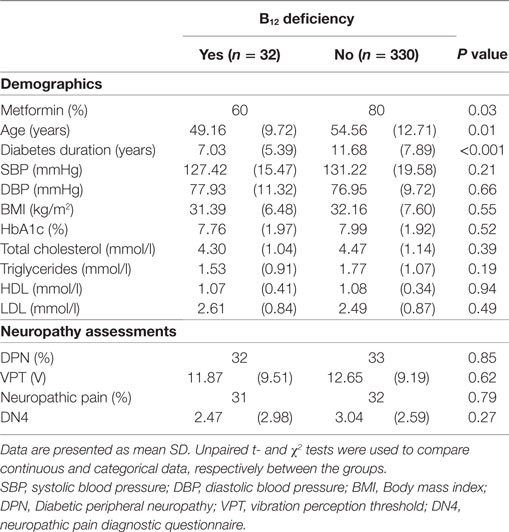
Table 2. Comparison of demographic and clinical characteristics between those with (serum B12 <133 pmol/l) and without B12 deficiency.
Simple linear regression analysis showed that VPT was positively associated with B12 (r = 0.18 P < 0.001). However, multiple linear regression analysis showed that this association was lost (β = 0.003, P = 0.25) after adjustment for confounding factors, including, age, diabetes duration, SBP, HbA1c, and PPI use. DN4 had no association with B12 levels.
Simple linear regression analysis shows that B12 levels were not associated with the use of Metformin, sulfonylurea, or calcium supplementation, but were associated with age (r = 0.15, P < 0.01), duration of diabetes (r = 0.16, P < 0.01), HbA1c (r = 0.11, P = 0.05), vitamin D (r = 0.17, P < 0.01), PPI use (r = 0.11, P < 0.05), multivitamin use (r = 0.11, P < 0.05), and B12 supplementation (r = 0.13, P < 0.05). However, multiple linear regression analysis showed that B12 levels maintained an association only with HbA1c (β = 12.72, P = 0.04) and vitamin D use (β = 2.72, P = 0.02), after adjustment for confounding factors.
This is the first study from the Middle East region to assess the association between Metformin exposure and B12 levels and its relationship to diabetic neuropathy. We show no difference in B12 levels between Metformin and non-Metformin users and actually show that the prevalence of B12 deficiency was lower in patients on Metformin. This is in contrast to some but not all previously published studies (12). Furthermore, we show no difference in the prevalence of DPN or painful diabetic neuropathy in T2DM patients with and without B12 deficiency.
The 2018 ADA Clinical Practice Recommendations endorse screening Metformin users for vitamin B12 deficiency and the 2017 ADA diabetic neuropathy statement recommends that all patients with diabetic neuropathy should be assessed for B12 deficiency, to exclude a treatable cause of neuropathy (13). However, previous studies examining the relationship between Metformin use and B12 deficiency (12); and indeed between B12 deficiency and neuropathy have been conflicting (11, 14–18). Indeed, a study has shown a lower prevalence of DPN in T2DM patients on Metformin compared to those not on Metformin (6). Ahmed et al. (17) used the neuropathy total scoring system (NTSS) and showed that subjects with normal B12 levels had a comparable prevalence of DPN to those with low B12 levels (36.8 vs 32.3%), and no correlation between B12 levels and NTSS (17). Russo et al. compared 79 subjects with DPN and 184 without DPN and found no relationship to Metformin use (16). Chen et al. using a neurothesiometer and monofilaments in addition to a structured questionnaire also showed no relationship between Metformin use and peripheral neuropathy (25). In contrast Singh et al. showed that Metformin users had lower levels of B12 and a higher Toronto Neuropathy Scoring System (14). Roy et al. showed that patients on Metformin had a lower level of B12 and a reduction in median, ulnar, and peroneal nerve conduction (15). In the DPPOS study, while Metformin was associated with an increased risk of B12 deficiency, only 13 of the 56 participants on Metformin with low vitamin B12 had neuropathy, but there was no difference in neuropathy symptoms or the total Michigan Neuropathy Screening Instrument score (7). A recent study from India has shown an association between Metformin use and B12 levels as well as DPN assessed using the Toronto Clinical Scoring System and median, ulnar, peroneal, and posterior tibial nerve conduction velocity (26).
Given that we showed a lower prevalence of B12 deficiency in patients taking Metformin, we assessed confounding factors such as other medications, which may alter B12 levels. Sulfonylurea use in combination with Metformin is a significant independent risk factor for B12 deficiency (8). B12 levels have also been reported to be lower in older adults with prolonged PPI and H2 blocker use in one study (27) but not in another study (28). Vitamin B supplementation is prevalent in the Middle East and may also influence B12 levels (29, 30). We show no association between B12 levels and concomitant use of sulfonylureas or calcium supplementations, but we do show small and significant associations with age, duration of diabetes, HbA1c, and treatment with vitamin D, PPI’s, multivitamins, and B12.
This is the first study to assess the relationship between Metformin use B12 deficiency and the prevalence and severity of DPN and diabetic painful neuropathy in Qatar. The prevalence of both sensory neuropathy and painful diabetic neuropathy was comparable to previously published data (31–33). A limitation of this study is that it is a retrospective cohort study, but VPT and DN4 were assessed without the investigators being aware of the treatment or B12 status. The majority of patients had been prescribed Metformin as first-line therapy in accord with international guidelines, unless they were intolerant or it was withdrawn (34), and, therefore, it was not possible to recruit a larger number of patients not on Metformin. We cannot establish the exact duration of Metformin exposure, although we can assume that Metformin was prescribed shortly after diagnosis and, therefore, exposure is approximately equivalent to the duration of diabetes, which was approximately 10 years. As noted in the meta-analysis of Chapman et al. the B12 lowering effect of Metformin occurs within 6 weeks to 3 months of commencing Metformin (12).
In conclusion, we show no difference in B12 levels or the severity of DPN or painful diabetic neuropathy in Metformin compared to non-Metformin users. We also show no difference in vibration perception or painful diabetic neuropathy in those with and without B12 deficiency. These data urge the need for further larger, prospective studies to confirm or refute the current findings to support or challenge the highly prevalent practice of prescribing B12 for neuropathy across the Middle East.
This study was carried out in accordance with the recommendations of Investigator guidance: Investigator obligations (HRP-800), Institutional Review Board (IRB) of WCM-Q and HMC. The protocol was approved by the IRB of WCM-Q and HMC. All subjects gave written informed consent in accordance with the Declaration of Helsinki.
RM, TE, and GP had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: RM and TE. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: RM, TE, and GP. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: GP and RM. Administrative, technical, or material support: all authors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank all the participants for their efforts and commitment to be involved in the study. This work was supported by a grant from Qatar Foundation (BMRP 20038654).
1. Viollet B, Guigas B, Sanz Garcia N, Leclerc J, Foretz M, Andreelli F. Cellular and molecular mechanisms of metformin: an overview. Clin Sci (Lond) (2012) 122:253–70. doi:10.1042/CS20110386
2. Berchtold P, Bolli P, Arbenz U, Keiser G. [Disturbance of intestinal absorption following metformin therapy (observations on the mode of action of biguanides)]. Diabetologia (1969) 5:405–12. doi:10.1007/BF00427979
3. Tomkin GH, Hadden DR, Weaver JA, Montgomery DA. Vitamin-B12 status of patients on long-term metformin therapy. Br Med J (1971) 2:685–7. doi:10.1136/bmj.2.5763.685
4. DeFronzo RA, Goodman AM. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. The Multicenter Metformin Study Group. N Engl J Med (1995) 333:541–9. doi:10.1056/NEJM199508313330902
5. de Jager J, Kooy A, Lehert P, Wulffele MG, van der Kolk J, Bets D, et al. Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. BMJ (2010) 340:c2181. doi:10.1136/bmj.c2181
6. de Groot-Kamphuis DM, van Dijk PR, Groenier KH, Houweling ST, Bilo HJ, Kleefstra N. Vitamin B12 deficiency and the lack of its consequences in type 2 diabetes patients using metformin. Neth J Med (2013) 71:386–90.
7. Aroda VR, Edelstein SL, Goldberg RB, Knowler WC, Marcovina SM, Orchard TJ, et al. Long-term metformin use and vitamin B12 deficiency in the diabetes prevention program outcomes study. J Clin Endocrinol Metab (2016) 101:1754–61. doi:10.1210/jc.2015-3754
8. Kang D, Yun JS, Ko SH, Lim TS, Ahn YB, Park YM, et al. Higher prevalence of metformin-induced vitamin B12 deficiency in sulfonylurea combination compared with insulin combination in patients with type 2 diabetes: a cross-sectional study. PLoS One (2014) 9:e109878. doi:10.1371/journal.pone.0109878
9. Reinstatler L, Qi YP, Williamson RS, Garn JV, Oakley GP Jr. Association of biochemical B(1)(2) deficiency with metformin therapy and vitamin B(1)(2) supplements: the National Health and Nutrition Examination Survey, 1999–2006. Diabetes Care (2012) 35:327–33. doi:10.2337/dc11-1582
10. Damiao CP, Rodrigues AO, Pinheiro MF, Cruz RAF, Cardoso GP, Taboada GF, et al. Prevalence of vitamin B12 deficiency in type 2 diabetic patients using metformin: a cross-sectional study. Sao Paulo Med J (2016) 134:473–9. doi:10.1590/1516-3180.2015.01382111
11. Khan A, Shafiq I, Hassan Shah M. Prevalence of vitamin B12 deficiency in patients with type II diabetes mellitus on metformin: a study from Khyber Pakhtunkhwa. Cureus (2017) 9:e1577. doi:10.7759/cureus.1577
12. Chapman LE, Darling AL, Brown JE. Association between metformin and vitamin B12 deficiency in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab (2016) 42:316–27. doi:10.1016/j.diabet.2016.03.008
13. Pop-Busui R, Boulton AJ, Feldman EL, Bril V, Freeman R, Malik RA, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care (2017) 40:136–54. doi:10.2337/dc16-2042
14. Singh AK, Kumar A, Karmakar D, Jha RK. Association of B12 deficiency and clinical neuropathy with metformin use in type 2 diabetes patients. J Postgrad Med (2013) 59:253–7. doi:10.4103/0022-3859.123143
15. Roy RP, Ghosh K, Ghosh M, Acharyya A, Bhattacharya A, Pal M, et al. Study of vitamin B12 deficiency and peripheral neuropathy in metformin-treated early type 2 diabetes mellitus. Indian J Endocrinol Metab (2016) 20:631–7. doi:10.4103/2230-8210.190542
16. Russo GT, Giandalia A, Romeo EL, Scarcella C, Gambadoro N, Zingale R, et al. Diabetic neuropathy is not associated with homocysteine, folate, vitamin B12 levels, and MTHFR C677T mutation in type 2 diabetic outpatients taking metformin. J Endocrinol Invest (2016) 39:305–14. doi:10.1007/s40618-015-0365-9
17. Ahmed MA, Muntingh G, Rheeder P. Vitamin B12 deficiency in metformin-treated type-2 diabetes patients, prevalence and association with peripheral neuropathy. BMC Pharmacol Toxicol (2016) 17:44. doi:10.1186/s40360-016-0088-3
18. Ma J, Yu H, Liu J, Chen Y, Wang Q, Xiang L. Metformin attenuates hyperalgesia and allodynia in rats with painful diabetic neuropathy induced by streptozotocin. Eur J Pharmacol (2015) 764:599–606. doi:10.1016/j.ejphar.2015.06.010
19. Olt S, Oznas O. Investigation of the vitamin B12 deficiency with peripheral neuropathy in patients with type 2 diabetes mellitus treated using metformin. North Clin Istanb (2017) 4:233–6. doi:10.14744/nci.2017.98705
20. Al-Azayzih A, Al-Azzam SI, Alzoubi KH, Shawaqfeh M, Masadeh MM. Evaluation of drug-prescribing patterns based on the WHO prescribing indicators at outpatient clinics of five hospitals in Jordan: a cross-sectional study. Int J Clin Pharmacol Ther (2017) 55:425–32. doi:10.5414/CP202733
21. Wiles PG, Pearce SM, Rice PJ, Mitchell JM. Vibration perception threshold: influence of age, height, sex, and smoking, and calculation of accurate centile values. Diabet Med (1991) 8:157–61. doi:10.1111/j.1464-5491.1991.tb01563.x
22. Harifi G, Ouilki I, El Bouchti I, Ouazar MA, Belkhou A, Younsi R, et al. Validity and reliability of the Arabic adapted version of the DN4 questionnaire (Douleur Neuropathique 4 Questions) for differential diagnosis of pain syndromes with a neuropathic or somatic component. Pain Pract (2011) 11:139–47. doi:10.1111/j.1533-2500.2010.00399.x
23. Spallone V, Morganti R, D’Amato C, Greco C, Cacciotti L, Marfia GA. Validation of DN4 as a screening tool for neuropathic pain in painful diabetic polyneuropathy. Diabet Med (2012) 29:578–85. doi:10.1111/j.1464-5491.2011.03500.x
24. Unal-Cevik I, Sarioglu-Ay S, Evcik D. A comparison of the DN4 and LANSS questionnaires in the assessment of neuropathic pain: validity and reliability of the Turkish version of DN4. J Pain (2010) 11:1129–35. doi:10.1016/j.jpain.2010.02.003
25. Chen S, Lansdown A, Moat S, Ellis R, Goringe A, Dunstan F, et al. An observational study of the effect of metformin on B12 status and peripheral neuropathy. Br J Diabetes Vasc Dis (2012) 12:189–93. doi:10.1177/1474651412454924
26. Gupta K, Jain A, Rohatgi A. An observational study of vitamin b12 levels and peripheral neuropathy profile in patients of diabetes mellitus on metformin therapy. Diabetes Metab Syndr (2018) 12:51–8. doi:10.1016/j.dsx.2017.08.014
27. den Elzen WP, Groeneveld Y, de Ruijter W, Souverijn JH, le Cessie S, Assendelft WJ, et al. Long-term use of proton pump inhibitors and vitamin B12 status in elderly individuals. Aliment Pharmacol Ther (2008) 27:491–7. doi:10.1111/j.1365-2036.2008.03601.x
28. Dharmarajan TS, Kanagala MR, Murakonda P, Lebelt AS, Norkus EP. Do acid-lowering agents affect vitamin B12 status in older adults? J Am Med Dir Assoc (2008) 9:162–7. doi:10.1016/j.jamda.2007.10.004
29. El-Khateeb M, Khader Y, Batieha A, Jaddou H, Hyassat D, Belbisi A, et al. Vitamin B12 deficiency in Jordan: a population-based study. Ann Nutr Metab (2014) 64:101–5. doi:10.1159/000355440
30. Asiri YA, Al-Arifi MN. Polypharmacy and patterns in drug prescribing at a primary healthcare centre in the Riyadh region of Saudi Arabia. Int J Pharm Pract (2011) 19:123–8. doi:10.1111/j.2042-7174.2010.00083.x
31. Malik RA, Aldinc E, Chan SP, Deerochanawong C, Hwu CM, Rosales RL, et al. Perceptions of painful diabetic peripheral neuropathy in South-East Asia: results from patient and physician surveys. Adv Ther (2017) 34:1426–37. doi:10.1007/s12325-017-0536-5
32. Almuhannadi H, Ponirakis G, Khan A, Malik RA. Diabetic neuropathy and painful diabetic neuropathy: cinderella complications in South East Asia. J Pak Med Assoc (2018) 68:85–9.
33. Petropoulos IN, Javed S, Azmi S, Khan A, Ponirakis G, Malik RA. Diabetic neuropathy and painful diabetic neuropathy in the Middle East and North Africa (MENA) region: much work needs to be done. J Taibah Univ Med Sci (2016) 11:284–94.
Keywords: metformin, vitamin B12 deficiency, diabetic neuropathy, diabetic painful neuropathy, type 2 diabetes mellitus
Citation: Elhadd T, Ponirakis G, Dabbous Z, Siddique M, Chinnaiyan S and Malik RA (2018) Metformin Use Is Not Associated With B12 Deficiency or Neuropathy in Patients With Type 2 Diabetes Mellitus in Qatar. Front. Endocrinol. 9:248. doi: 10.3389/fendo.2018.00248
Received: 03 February 2018; Accepted: 02 May 2018;
Published: 25 May 2018
Edited by:
Soroku Yagihashi, Hirosaki University, JapanCopyright: © 2018 Elhadd, Ponirakis, Dabbous, Siddique, Chinnaiyan and Malik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rayaz A. Malik, cmFtMjA0NUBxYXRhci1tZWQuY29ybmVsbC5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.