- 1Center for Infectious Diseases, Beijing Youan Hospital, Capital Medical University, Beijing, China
- 2Beijing Key Laboratory for HIV/AIDS Research, Beijing, China
- 3Institute of Psychology, Chinese Academy of Sciences, Beijing, China
- 4State Key Laboratory of Cognitive Neuroscience and Learning, Beijing Normal University, Beijing, China
- 5Department of Psychology, Research Institute for International and Comparative Education, Shanghai Normal University, Shanghai, China
Objective: China has the largest population living with dementia, causing a tremendous burden on the aging society. Cardiovascular disease (CVD) may trigger a cascade of pathologies associated with cognitive aging. We aim to investigate the association between cardiovascular risk (CVR) factors and cognitive function in the nationally representative cohort in China.
Methods: Participants were recruited from 150 counties in 28 provinces via a four-stage sampling method. The outcomes included several cognitive tasks. The independent variable was a composite score of cardiovascular risk calculated from sex-specific equations. We fitted the time-lagged regression to model the association between CVR and cognition. Besides, we performed cross-group analyses to test for model invariance across sex and age. We thus constrained path coefficients to be equal across each grouping variable (e.g., sex) and compared the fit of this constrained model with an unconstrained model in which the path coefficients were allowed to vary by group.
Results: A total of 3,799 participants were included in the final analyses. We found that the CVR had a negative linear association with global cognition (β = −0.1, p < 0.01). Additionally, CVR had inverse linear associations with domain-specific measurements of memory and learning, calculation, orientation, and visual–spatial ability (all values of p < 0.01). Regarding sex and age moderation, males had a more pronounced association between higher CVR and worse general cognition, immediate recall, orientation, calculation, and visual–spatial ability (all values of p < 0.0001). In contrast, females exhibited a slightly larger negative association in delayed recall. Older participants (>65 years old) had a more pronounced association between higher CVR and worse calculation ability (p = 0.003).
Conclusion: CVD are risk factors for lower global cognition and cognitive subdomains in middle-aged and older adults in China.
Introducton
China has the largest population of patients aged over 60 living with dementia in the world, and it has an estimated population of 9.5 million (1), causing a severe public and economic burden on the social and health care systems (2). Cardiovascular disease (CVD) is the leading cause of death in China (3). Compared to the non-Asian older adults, the prevalence of hypertension, diabetes, and hyperlipidemia in China and other Asian countries might be higher and persists upward (4–6). Worsened cardiovascular health triggers a cascade of pathologies associated with cognitive impairment and dementia in older adults (7). Most of the clinical evidence is based on non-Asian populations (8–14).
Few studies exploring the association between composite cardiovascular risk (CVR) and cognition have been conducted in Chinese or other East Asia populations. Most studies examining the specific CVR (e.g., hypertension or diabetes) and cognition decline provided the mixed evidence (15–20). Most studies lacked rigorous sampling methods (17), large sample size, longitudinal follow-ups, or detailed information for other confounders (e.g., depression symptoms) (11), leading to unreliable results.
CVRs are prone to cluster in older and middle-aged adults (11). The sex-specific cardiac and vascular aging patterns in early adulthood play an essential role in later life (21). Independent examination of specific CVR may hinder our understanding of the complex interplay of different CVRs on cognition. To date, some studies examining the association of composite CVR [e.g., Framingham Cardiovascular Risk Score (FCRS)] and cognition (e.g., episodic memory) found a significant association between composite CVR and cognitive impairment, cognitive decline, dementia, and mortality rate in Whites (8, 9, 22) and Latino (23). Despite the wide use of FCRS, some have challenged the external validity to non-Whites (10). It is an urgent need to test whether FCRS is also a useful tool among Chinese adults.
This study uses the data from a nationally representative sample in Chinese to examine the composite CVR and cognitive function. Specifically, we investigate longitudinal associations between global vascular risk and domain-specific measurements. We hypothesize that higher CVR will be associated with lower cognitive performance. We also expect that sex and age modification may present in the current sample due to the heterogeneity of age- and sex-specific trajectories in cardiac and cognitive aging.
Methods
Participants and Protocol
The data were drawn from the first and fourth waves of the China Health and Retirement Longitudinal Study (CHARLS), a nationally representative longitudinal survey of the older residents in China. The baseline sample was obtained via a four-stage random sampling method, covering participants from 150 counties in 28 provinces in China in 2011. The study design and sampling method's detailed information can be found in Zhao et al. (24). Only waves one (2011) and four (2015) were used in the final analyses due to the blood tests' availability in these waves. Participants were excluded if they (1) are aged younger than 50 years old, (2) did not receive fasting blood test or had no testing results on CVD factors, (3) did not respond to any cognitive tests, and (4) reported having received a diagnosis of memory-related disease (such as Alzheimer disease, Parkinson, brain atrophy, or brain cancer). This study was approved by the Institutional Review Board of Beijing Youan Hospital.
Measurements
Cardiovascular risk was defined as a pooled score (Framingham cardiovascular risk score) using sex-specific equations combining age, systolic blood pressure and antihypertension treatment, diabetes, HDL, smoking, and total cholesterol.
Cognitive function comprised (1) a global cognitive measure, based on a pooled Z-score of immediate recall, delayed recall, figure copying, calculation, orientation, and digital-series reasoning, and (2) five domain-specific measurements. The Chinese verbal learning test is an episodic learning and memory test with two scores: (1) immediate recall, and (2) delayed recall. The summed total of correct words range from 0 to10 at each recall phase. We also adopted minus 7 and orientation tests from the Montreal Cognitive Assessment (MoCA). Considering the relatively low literacy among Chinese older adults, we adopted two overlapped pentagons instead of cubic in the figure-copying test.
Covariates in the regression model for CVR–cognition associations were education (high school or above vs. below high school), Hukou (agricultural vs. non-agricultural), marital status (married, separated, divorced, and widowed, and never married), regional distribution (western China, eastern China, and mid-China), employment status (farming, non-farming, both, unemployed) depressive symptoms (using a cutoff of 10 in CESD-10), BMI, waist-to-height ratio, and residence status (family housing vs. nursing home, hospital, or other), drinking status (>once/per month, < =once per month, no) and stroke (yes, no).
Statistic Strategies
Our analyses were conducted in three stages. First, we generated the descriptive statistics for a sample of interest to provide detailed baseline information. We used mean and standard deviation for continuous variables and proportion for categorical variables. Second, we fitted the time-lagged regression to model the association between CVR and cognition, including autoregression models and CVR main effect models. We used three primary indices to assess the adequacy of model-data fit: the comparative fit index (CFI), the standardized root mean square residual (SRMR), and the root mean square error of approximation (RMSEA). The acceptable level of model fit was CFI higher than 0.90, RMSEA lower than 0.08, and SRMR lower than 0.08 (25). Third, we performed cross-group analyses to test for model invariance across sex and age. Specifically, we constrained path coefficients to be equal across each grouping variable (e.g., sex) and compared the fit of this constrained model with an unconstrained model in which the path coefficients were allowed to vary by group. Model invariance can be assumed when the constrained model does not yield substantially poorer fit to the data than does the unconstrained version. Two indexes were used to compare the fit of the constrained and unconstrained models, the scaled difference in Satorra–Bentler (S–B) χ2 statistic and the difference in CFI values between models (26). The two models can be judged as invariant across moderator variables where their differences in fit do not reach the criterion for practical significance (ΔCFI differences > 0.01) (26).
Results
Study Characteristics
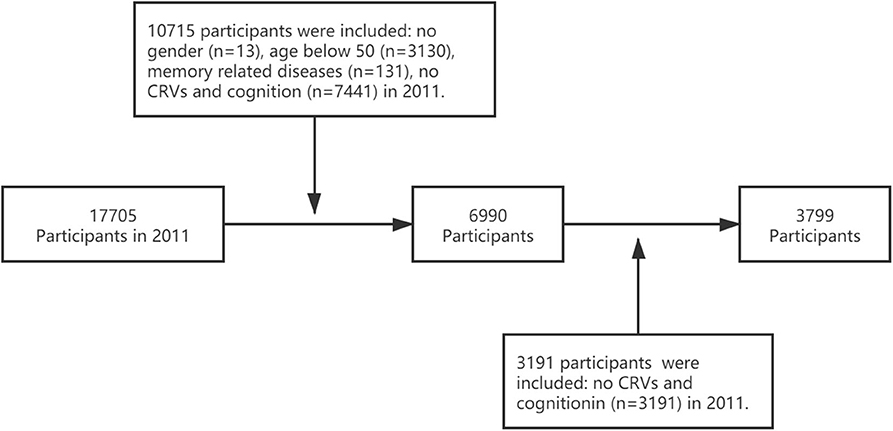
Of the total sample (n = 17,705), 10,715 participants from the baseline were excluded because they (1) were aged <50 years old (n = 3,130), (2) had no fasting blood test or no results on at least one CVD factor or cognition assessment (n = 7,441), (3) had the memory-related disease (n = 131), and (4) did not report gender (n = 13). We excluded 3,191 participants from the 2015 visit without CVR and cognition assessment. Finally, we included a total of 3,799 participants in the final analyses (Figure 1).
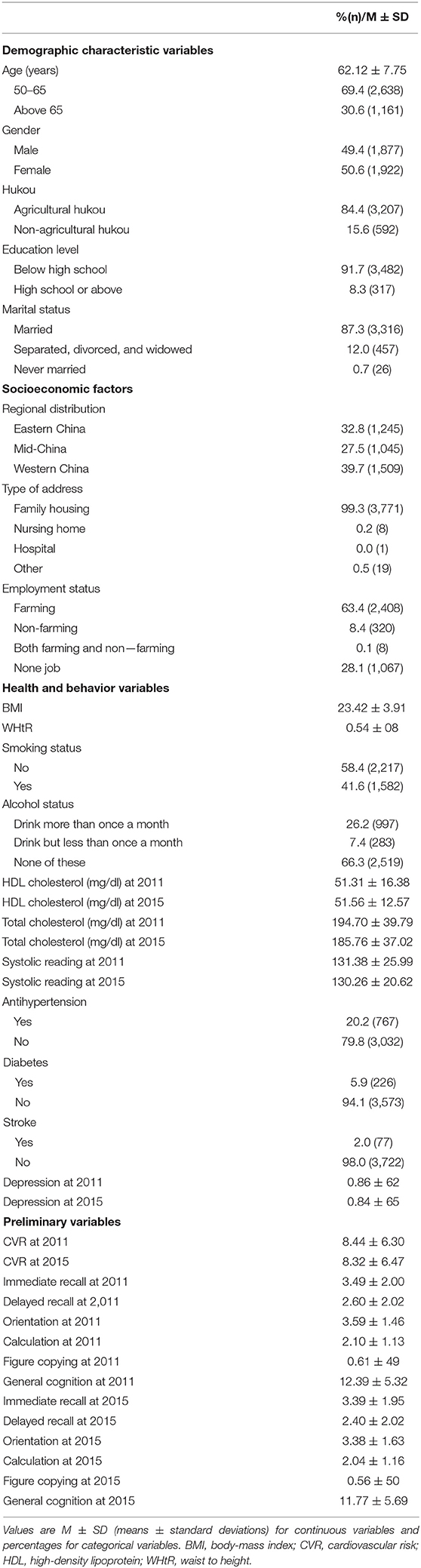
About half of the target participants were female (50.6%), and the mean age was 62.12 (SD = 7.75). Besides, 84.4% of the participants possessed agricultural hukou, while only 8.3% had high school or above degrees, and 87.3% were married. Around one third lived in eastern China (developed part), and almost all participants (99.3%) resided in family houses. Also, nearly three quarters conducted farming or/and no-farming jobs.
Other detailed information for health status and behavior are also shown in Table 1.
Association Between Composite CVR and Cognition
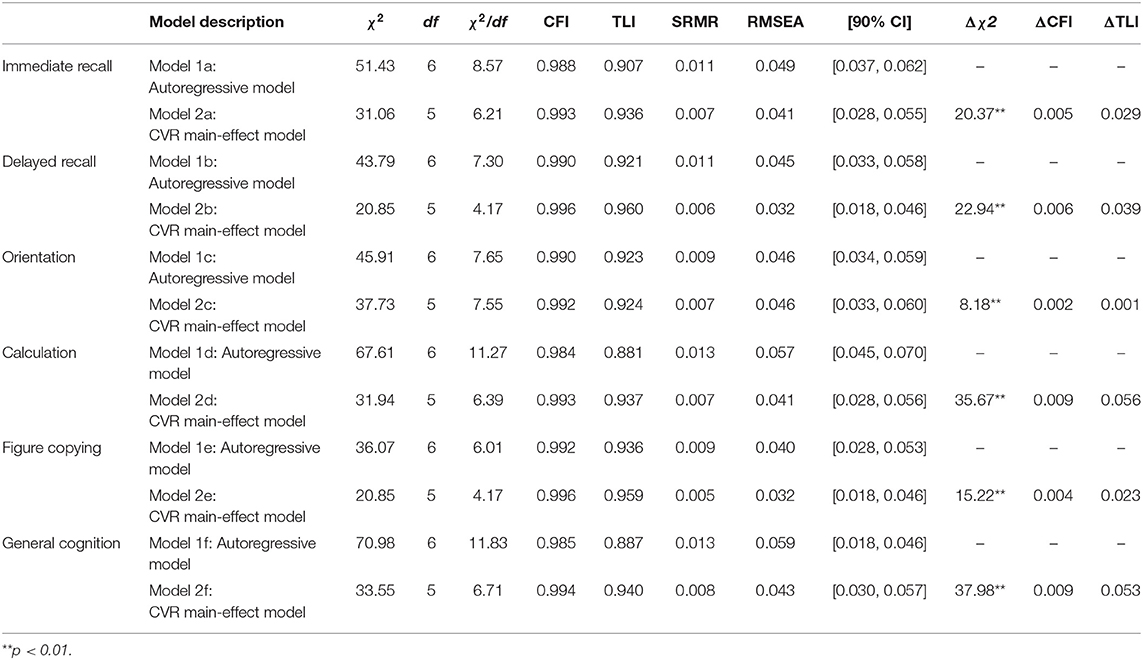
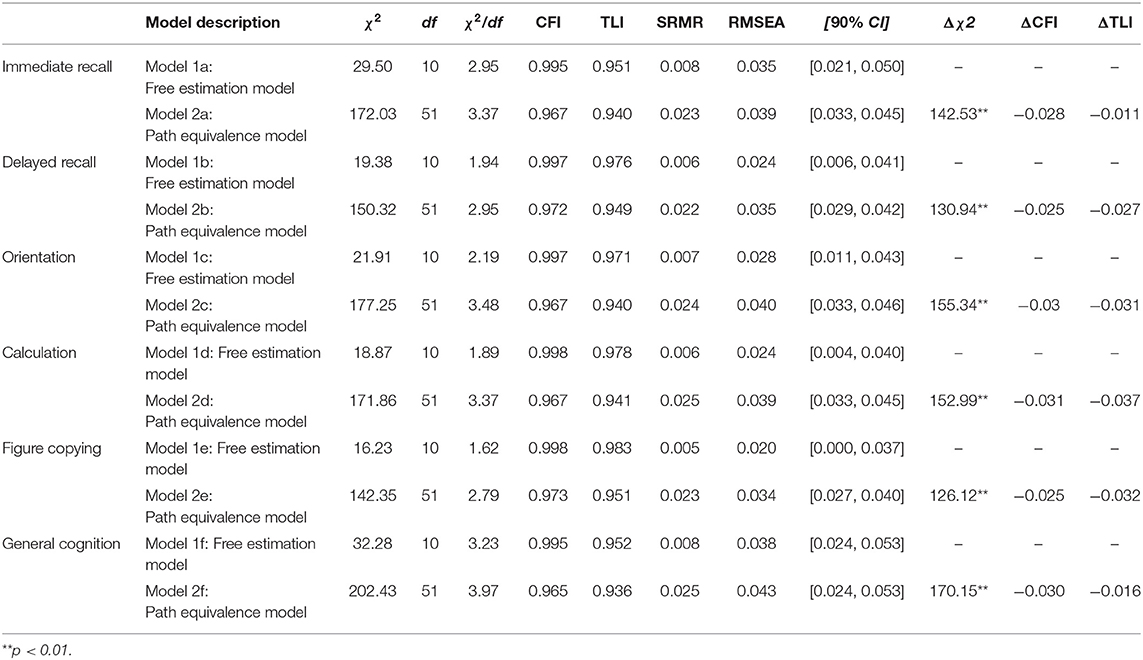
The model fit index (CFI) ranged from 0.984 to 0.996, RMSEA from 0.032 to 0.059, and SRMR from 0.005 to 0.013 (Table 1). More indices for model fit are also shown in Table 2.
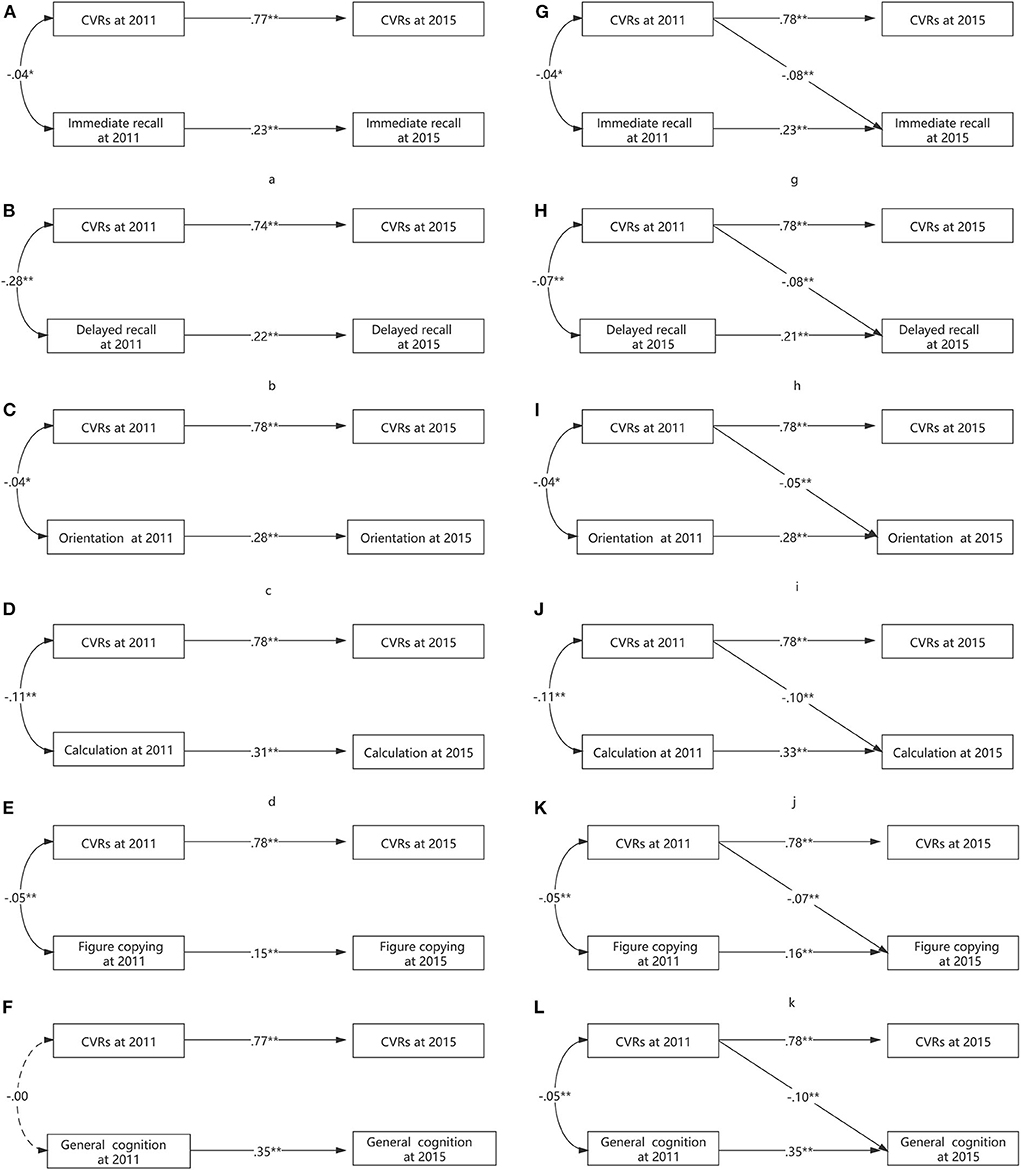
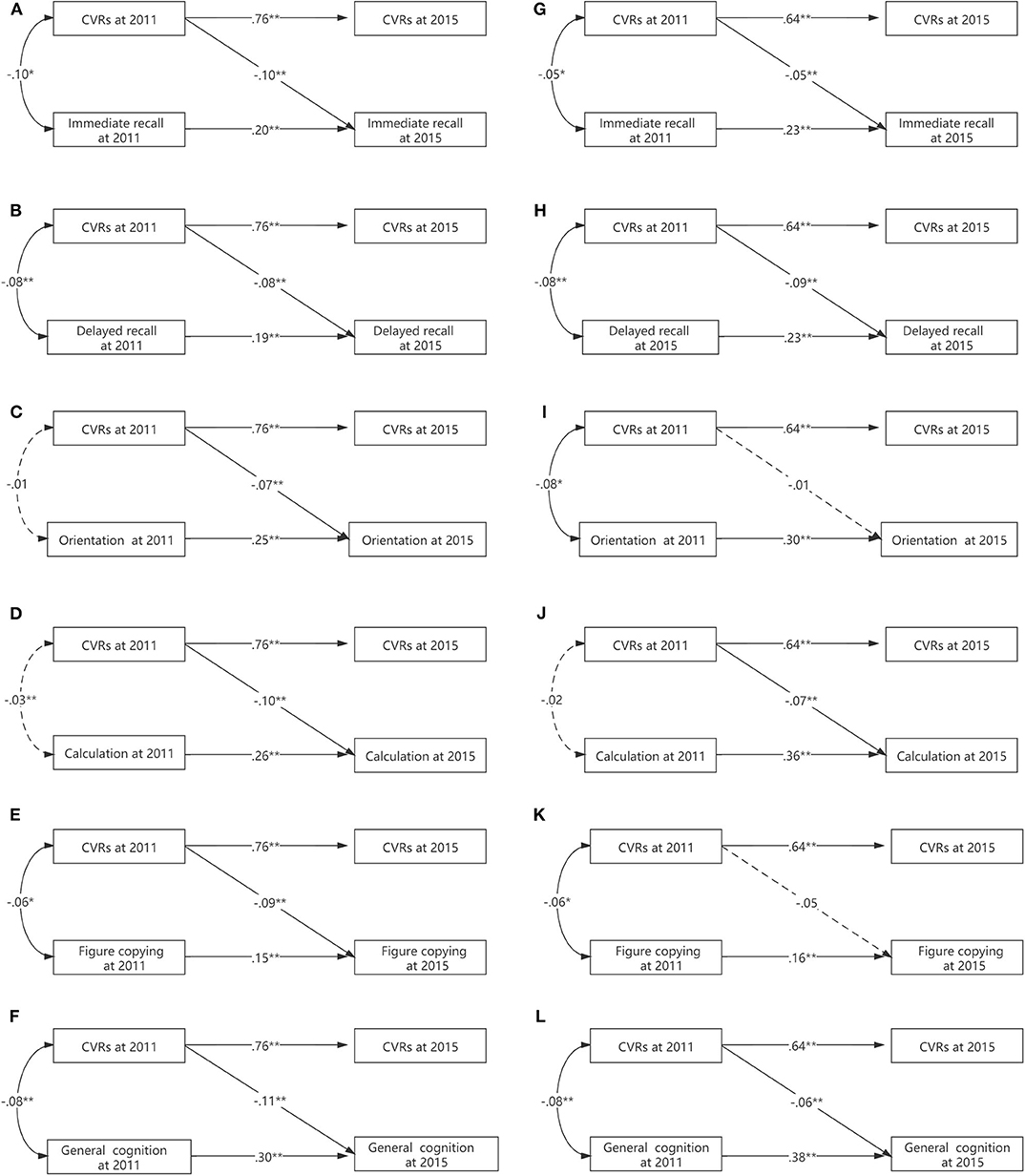
At baseline, we found that the FCRS had a consistent negative linear association with global cognition (β = −0.05, p < 0.01). Additionally, FCRS had inverse linear associations with domain-specific measurements of memory and learning (delayed recall and immediate recall), the calculation (100 minus 7), orientation, and visual–spatial ability (figure copying) (Figure 2).
At follow-up, we found that the baseline FCRS had an inverse linear association with follow-up global cognition (β = −0.07, p < 0.01). Besides, baseline FCRS had inverse linear associations with domain-specific measurements of memory and learning (delayed recall and immediate recall), the calculation (100 minus 7), orientation, and visual–spatial ability (figure copying) (Figure 2).
Sex Modification
Tests of interactions for CVR with sex provided evidence for modification, indicated by ΔCFI > 0.01 in all outcomes (Table 3). Males had a more pronounced association between higher CVR and worse general cognition, immediate recall, orientation, calculation, and visual–spatial ability (all values of p < 0.0001), while females exhibited a slightly larger negative association in delayed recall (Figure 3).
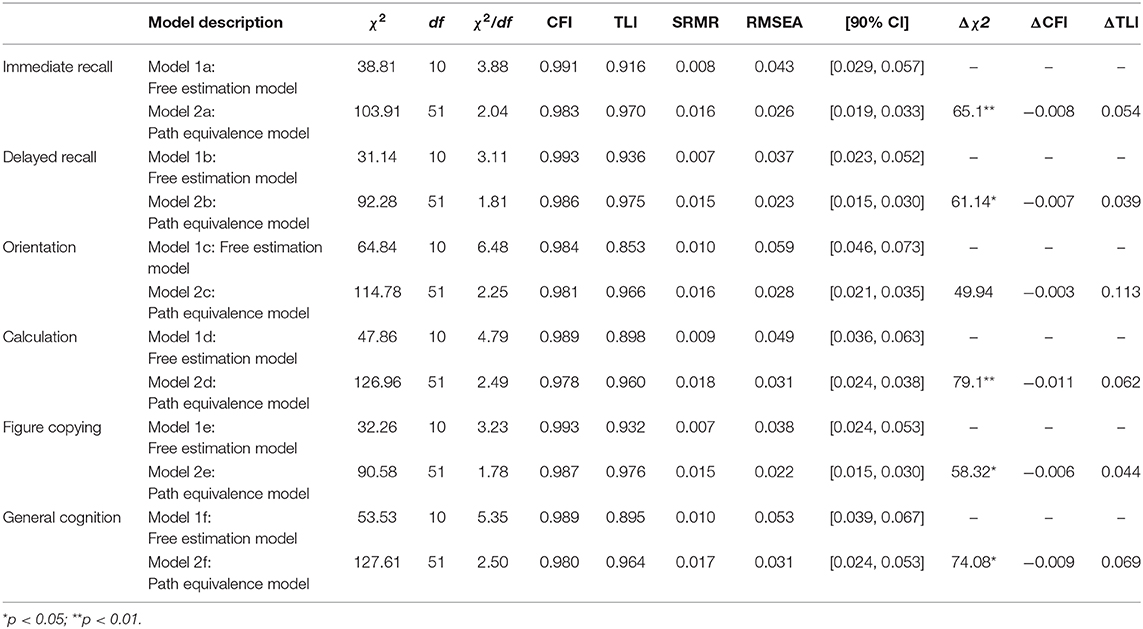
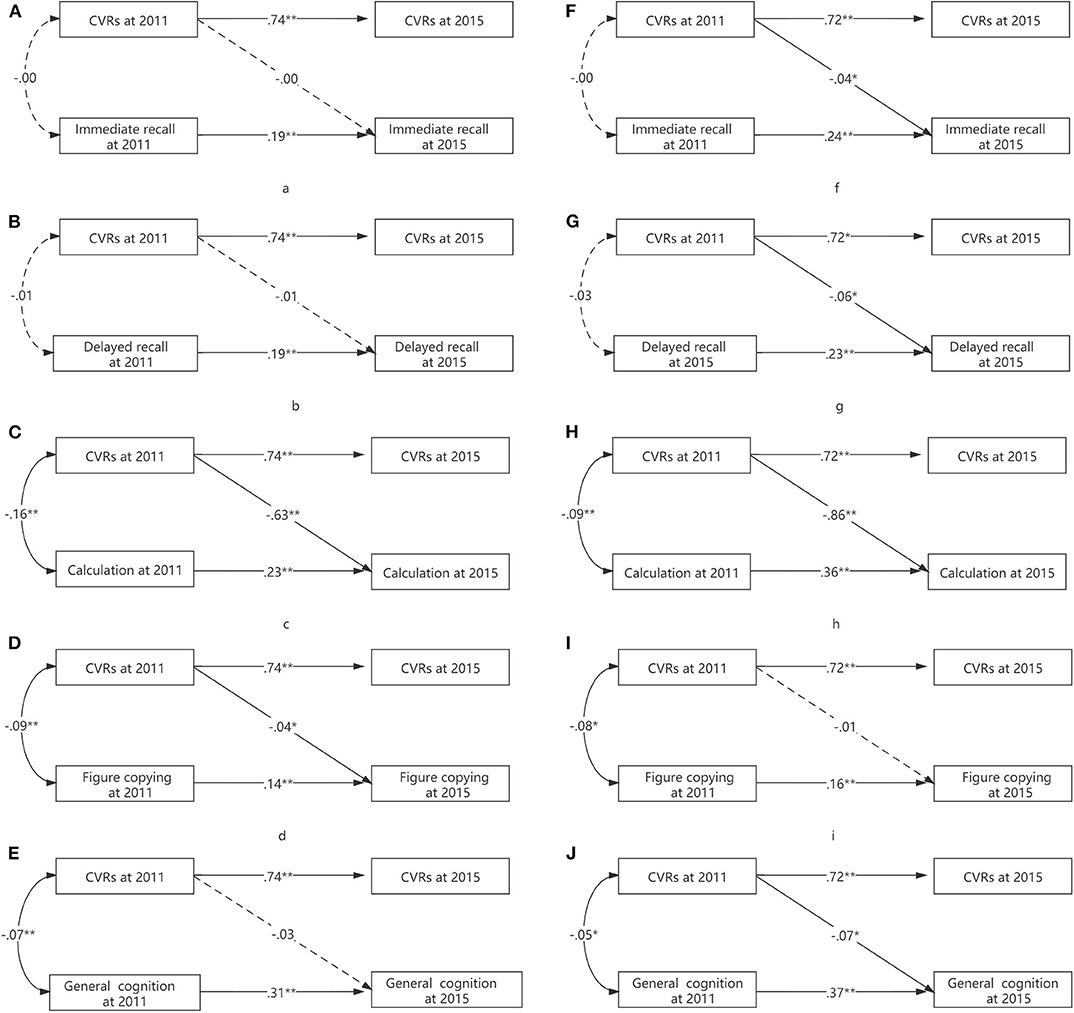
Age Modification
Tests of interactions for CVR with age provided some evidence for modification in the calculation test (ΔCFI = 0.11) (Table 4). Older participants (>65 years old) had a more pronounced association between higher CVR and worse calculation ability (p = 0.003) (Figure 4).
Discussion
We found that higher CVR was associated with cognitive decline in various cognitive tasks. These results extended the evidence from other ethnicities (8, 9, 22) to Chinese. Additionally, existing evidence drives mainly from young older adults. Our sample fixed this limitation by recruiting the participants with a wide range of age spectrum (50–93 years old). We also found age and sex modification effects on multiple cognitive tasks but in different patterns: age modification effects on the calculation test while sex modification effects on all tests.
Regarding the association between CVR and cognitive function, our results were consistent with previous original articles in older adults (27–31). The association remains significant even after adjusting other demographic and socioeconomic covariates, indicating CVR might be an independent factor for cognition. Besides, our results found the negative association between CVR and all cognitive tasks. A recent fMRI study comprising 9,722 participants found that CVR was associated with higher white matter hyperintensity volumes, poorer white matter microstructure in association and thalamic pathways, and lower frontal, temporal volumes (32). This large-scale brain atrophy may be the cause of the cognitive decline in multiple cognitive domains. Also, CVD (e.g., hypertension) may lead to cerebral hypoperfusion, which may also trigger cascade impacts on various brain regions (33).
Regarding the modification effects of sex, sex modified all cognitive tasks. Sex differences were observed in global cognitive function (34, 35) and in several cognitive domains (e.g., episodic memory and executive function) among older adults (36–38). Besides, sex differences were also overserved in CVD's prevalence or incidence (39–41), indicated by higher CVD in men. Middle-aged and older Chinese have a much higher probability of abdominal obesity in men and more likely to meet the criteria of metabolic syndrome (42). Interestingly, Asperholm et al. (37) conducted a meta-analytic study examining sex differences in various episodic memory tasks and found that men may use their spatial advantage in spatially episodic memory tasks. In contrast, women do well in episodic memory tasks that are verbalized recall and non-verbal and non-spatial tasks that are neither verbal nor spatial. Though there are sex differences in both CVD and cognitive function, the role of sex in the relationship between CVD and cognition is complex and requires additional investigation.
With respect to the modification effects of age, the aging process is associated with altered brain intrinsic connectivity (43) and brain atrophy (44). The aging process is also associated with cognitive decline in multiple cognitive domains (45, 46). The age and CVR interaction in predicting cognitive function also partially replicated in other ethnicity (22). Old-old participants demonstrated a steeper slope in the calculation test than the young-old, which means calculation ability might be a sensitive behavior marker in evaluating the age moderation. Therefore, calculation training programs should be adopted as preventive strategies in middle-aged and young-old adults and mitigating methods for the old-old.
The study has several strengths. First, it used CHARLS data, the most representative and technically sound cohort with the largest sample size. Second, we adopted a composite CVR score to elucidate the association, which provided a relatively comprehensive picture of this issue. Third, the longitudinal study offers us opportunities to evaluate the temporal relationship between CVR and cognition.
Several limitations should also be addressed. First, we could not link genetic risk factors (e.g., APOE) with cognitive function. APOE plays a vital role in lipid metabolism and amyloid pathology cognitive function (47, 48). Second, we did not collect MRI data. A recent study using UK Biobank data has identified that the CVD is associated with brain atrophy in large-scale brain regions (32). These limitations should be solved in future megacohorts by comprehensively evaluating the risk profiles. Third, we did not adopt an in-depth multimodality cognitive assessment. Other cognitive domains (e.g., complex attention or executive function) should also be taken into consideration. Fourth, the rate of loss-to-follow is high, which may lead to selection bias. Participants in worse conditions at baseline may be more likely to drop out of the cohort due to illness or mortality in the follow-up visits.
Conclusion
CVD are risk factors for lower global cognitive function and subdomains in middle-aged and older adults in China. Sex significantly moderates the CRV–cognition associations while age only moderating the CRV–calculation association.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: http://charls.pku.edu.cn/index/en.html.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of Beijing Youan Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JH, WH, and WW were responsible for the study concept and design. JH, RS, and BC analyzed the data. JH, JF, RS, CG, and WW interpreted the data. JH drafted the manuscript. All authors revised and approved the manuscript.
Funding
This work was also supported by the National 13th 5-Year Grand Program on Key Infectious Disease Control (2018ZX10715-005-002-002 to CG, 2017ZX10202101-001-004 to WW, 2017ZX10202101-004-001 to TZ, and 2018ZX10301-407-005 and 2018ZX10302103-001-003 to TJ), the Beijing Municipal of Science and Technology Major Project (D161100000416003 to HW and D161100000416005 to CG), Fund of Key Laboratory of Capital Medical University (BJYAHKF2017002 to WH), and the Beijing Key Laboratory for HIV/AIDS Research (BZ0089). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the China Center for Economic Research, National School of Development, Peking University, for providing the data.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2020.560947/full#supplementary-material
References
1. Wu YT, Ali GC, Guerchet M, Prina AM, Chan KY, Prince M, et al. Prevalence of dementia in mainland China, Hong Kong and Taiwan: an updated systematic review and meta-analysis. Int J Epidemiol. (2018) 47:709–19. doi: 10.1093/ije/dyy007
2. Jia LF, Quan MN, Fu Y, Zhao T, Li Y, Wei CB, et al. Dementia in China: epidemiology, clinical management, research advances. Lancet Neurol. (2020) 19:81–92. doi: 10.1016/S1474-4422(19)30290-X
3. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. (2019) 16:203–12. doi: 10.1038/s41569-018-0119-4
4. Mobasseri M, Shirmohammadi M, Amiri T, Vahed N, Hosseini Fard H, Ghojazadeh M. Prevalence and incidence of type 1 diabetes in the world: a systematic review and meta-analysis. Health Promotion Persp. (2020) 10:98–115. doi: 10.34172/hpp.2020.18
5. Bao M, Wang L. The longitudinal trend of hypertension prevalence in Chinese adults from 1959 to 2018: a systematic review and meta-analysis. Ann Pall Med. (2020) 9:2485–97. doi: 10.21037/apm-19-377
6. Noubiap JJ, Nansseu JR, Nyaga UF, Sime PS, Francis I, Bigna JJ. Global prevalence of resistant hypertension: a meta-analysis of data from 3.2 million patients. Heart. (2019) 105:98–105. doi: 10.1136/heartjnl-2018-313599
7. Qiu C, Fratiglioni L. A major role for cardiovascular burden in age-related cognitive decline. Nat Rev Cardiol. (2015) 12:267–77. doi: 10.1038/nrcardio.2014.223
8. Dregan A, Stewart R, Gulliford MC. Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study. Age Ageing. (2013) 42:338–45. doi: 10.1093/ageing/afs166
9. Joosten H, van Eersel ME, Gansevoort RT, Bilo HJ, Slaets JP, Izaks GJ. Cardiovascular risk profile and cognitive function in young, middle-aged, elderly subjects. Stroke. (2013) 44:1543–9. doi: 10.1161/STROKEAHA.111.000496
10. Warsch JR, Rundek T, Paik MC, Elkind MS, Sacco RL, Wright CB. Association between northern Manhattan study global vascular risk score and successful aging. J Am Geriatr Soc. (2013) 61:519–24. doi: 10.1111/jgs.12166
11. Sacco RL, Khatri M, Rundek T, Xu Q, Gardener H, Boden-Albala B, et al. Improving global vascular risk prediction with behavioral and anthropometric factors. The multiethnic NOMAS (Northern Manhattan Cohort Study). J Am Coll Cardiol. (2009) 54:2303–11. doi: 10.1016/j.jacc.2009.07.047
12. Houle B, Gaziano T, Farrell M, Gomez-Olive FX, Kobayashi LC, Crowther NJ, et al. Cognitive function and cardiometabolic disease risk factors in rural South Africa: baseline evidence from the HAALSI study. BMC Public Health. (2019) 19:1579. doi: 10.1186/s12889-019-7938-z
13. A NDV, Bernstein JPK, Weitzner D, Calamia M, Keller JN. The effects of cardiovascular risk factors on repeatable battery for the assessment of neuropsychological status (RBANS) performance in cognitively healthy older adults. Arch Clin Neuropsychol. (2019) 24:acz039. doi: 10.1093/arclin/acz039
14. Ashrafi F, Taheri MS, Farzaneh A, Behnam B, Ahmadi MA. Cognitive functions and white matter lesions on magnetic resonance images in a sample of normal Iranian population with cardiovascular risk factors. Neuroradiol J. (2019) 32:108–14. doi: 10.1177/1971400919825862
15. Streit S, Poortvliet RKE, den Elzen WPJ, Blom JW, Gussekloo J. Systolic blood pressure and cognitive decline in older adults with hypertension. Ann Fam Med. (2019) 17:100–7. doi: 10.1370/afm.2367
16. Devore E, Hall KE, Schernhammer ES, Grodstein F. Midlife hypertension and hypercholesterolemia in relation to cognitive function later in life in black women. Am J Nurs. (2019) 119:22–30. doi: 10.1097/01.NAJ.0000553179.89954.bc
17. Weidung B, Littbrand H, Nordstrom P, Carlberg B, Gustafson Y. The association between SBP and mortality risk differs with level of cognitive function in very old individuals. J Hypertens. (2016) 34:745–52. doi: 10.1097/HJH.0000000000000831
18. Cukierman T, Gerstein HC, Williamson JD. Cognitive decline and dementia in diabetes - systematic overview of prospective observational studies. Diabetologia. (2005) 48:2460–9. doi: 10.1007/s00125-005-0023-4
19. Liang XN, Shan Y, Ding D, Zhao QH, Guo QH, Zheng L, et al. Hypertension and high blood pressure are associated with dementia among chinese dwelling elderly: the shanghai aging study. Front Neurol. (2018) 9:7. doi: 10.3389/fneur.2018.00664
20. Gao SJ, Jin YL, Unverzagt FW, Liang CK, Hall KS, Ma F, et al. Hypertension and cognitive decline in rural elderly chinese. J Am Geriatr Soc. (2009) 57:1051–7. doi: 10.1111/j.1532-5415.2009.02267.x
21. Merz AA, Cheng S. Sex differences in cardiovascular ageing. Heart. (2016) 102:825–31. doi: 10.1136/heartjnl-2015-308769
22. Harrison SL, de Craen AJ, Kerse N, Teh R, Granic A, Davies K, et al. Predicting risk of cognitive decline in very old adults using three models: the framingham stroke risk profile; the cardiovascular risk factors, aging, and dementia model; and oxi-inflammatory biomarkers. J Am Geriatr Soc. (2017) 65:381–9. doi: 10.1111/jgs.14532
23. Tarraf W, Kaplan R, Daviglus M, Gallo LC, Schneiderman N, Penedo FJ, et al. Cardiovascular risk and cognitive function in middle-aged and older hispanics/latinos: results from the hispanic community health study/study of latinos (HCHS/SOL). J Alzheimer's Dis. (2020) 73:103–16. doi: 10.3233/JAD-190830
24. Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the china health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
25. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria vs. new alternatives. Struct Equ Modeling. (1999) 6:1–55. doi: 10.1080/10705519909540118
26. Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. (2001) 66:507–14. doi: 10.1007/BF02296192
27. Lai MMY, Sharman MJ, Ames DJ, Ellis KA, Cox KL, Hepworth G, et al. Relationship of established cardiovascular risk factors and peripheral biomarkers on cognitive function in adults at risk of cognitive deterioration. J Alzheimer's Dis. (2020) 74:163–71. doi: 10.3233/JAD-190953
28. Karalija N, Wahlin A, Ek J, Rieckmann A, Papenberg G, Salami A, et al. Cardiovascular factors are related to dopamine integrity and cognition in aging. Ann Clin Transl Neurol. (2019) 6:2291–303. doi: 10.1002/acn3.50927
29. Guiney H, Lucas SJE, Cotter JD, Machado L. Investigating links between habitual physical activity, cerebrovascular function, and cognitive control in healthy older adults. Neuropsychologia. (2019) 125:62–9. doi: 10.1016/j.neuropsychologia.2019.01.011
30. Callisaya ML, Beare R, Moran C, Phan T, Wang W, Srikanth VK. Type 2 diabetes mellitus, brain atrophy and cognitive decline in older people: a longitudinal study. Diabetologia. (2019) 62:448–58. doi: 10.1007/s00125-018-4778-9
31. Palta P, Carlson MC, Crum RM, Colantuoni E, Sharrett AR, Yasar S, et al. Diabetes and cognitive decline in older adults: the ginkgo evaluation of memory study. J Gerontol Ser A. Biol Sci Med Sci. (2017) 73:123–30. doi: 10.1093/gerona/glx076
32. Cox SR, Lyall DM, Ritchie SJ, Bastin ME, Harris MA, Buchanan CR, et al. Associations between vascular risk factors and brain MRI indices in UK Biobank. Eur Heart J. (2019) 40:2290–300. doi: 10.1093/eurheartj/ehz100
33. Cipolla MJ, Liebeskind DS, Chan SL. The importance of comorbidities in ischemic stroke: impact of hypertension on the cerebral circulation. J Cerebral Blood Flow Metabol. (2018) 38:2129–49. doi: 10.1177/0271678X18800589
34. Xu H, Vorderstrasse AA, Dupre ME, McConnell ES, Ostbye T, Wu B. Gender differences in the association between migration and cognitive function among older adults in China and India. Arch Gerontol Geriatr. (2019) 81:31–8. doi: 10.1016/j.archger.2018.11.011
35. Lee S, Lee S, Lee E, Youm Y, Cho HS, Kim WJ. Gender differences in social network of cognitive function among community-dwelling older adults. Geriatr Gerontol Int. (2020) 20:467–73. doi: 10.1111/ggi.13906
36. Seinstra M, Grzymek K, Kalenscher T. Gender-specific differences in the relationship between autobiographical memory and intertemporal choice in older adults. PloS ONE. (2015) 10:e0137061. doi: 10.1371/journal.pone.0137061
37. Asperholm M, Hogman N, Rafi J, Herlitz A. What did you do yesterday? A meta-analysis of sex differences in episodic memory. Psychol Bull. (2019) 145:785–821. doi: 10.1037/bul0000197
38. McCarrey AC, An Y, Kitner-Triolo MH, Ferrucci L, Resnick SM. Sex differences in cognitive trajectories in clinically normal older adults. Psychol Aging. (2016) 31:166–75. doi: 10.1037/pag0000070
39. Mathenge N, Fan W, Wong ND, Hirsch C, Delaney CJ, Amsterdam EA, et al. Pre-diabetes, diabetes and predictors of incident angina among older women and men in the cardiovascular health study. Diabet Vasc Dis Res. (2020) 17:1479164119888476. doi: 10.1177/1479164119888476
40. Qu Y, Yang J, Zhang F, Li C, Dai Y, Yang H, et al. Gender-related differences in clinical characteristics and outcomes of premature coronary artery disease: insight from the focus registry. J Int cardiol. (2019) 2019:6762089. doi: 10.1155/2019/6762089
41. Ricciardi D, Arena G, Verlato R, Iacopino S, Pieragnoli P, Molon G, et al. Sex effect on efficacy of pulmonary vein cryoablation in patients with atrial fibrillation: data from the multicenter real-world 1STOP project. J Inter Cardiac Electrophysiol. (2019) 56:9–18. doi: 10.1007/s10840-019-00601-3
42. Yang F. Prevalence of the metabolic syndrome in the middle-aged and older Chinese population. Int Diabetes Dev Ctries. (2017) 37:176–82. doi: 10.1007/s13410-016-0472-y
43. Damoiseaux JS. Effects of aging on functional and structural brain connectivity. NeuroImage. (2017) 160:32–40. doi: 10.1016/j.neuroimage.2017.01.077
44. Pini L, Pievani M, Bocchetta M, Altomare D, Bosco P, Cavedo E, et al. Brain atrophy in alzheimer's disease and aging. Ageing Res Rev. (2016) 30:25–48. doi: 10.1016/j.arr.2016.01.002
45. Olaya B, Bobak M, Haro JM, Demakakos P. Trajectories of verbal episodic memory in middle-aged and older adults: evidence from the english longitudinal study of ageing. J Am Geriatr Soc. (2017) 65:1274–81. doi: 10.1111/jgs.14789
46. Zettel-Watson L, Suen M, Wehbe L, Rutledge DN, Cherry BJ. Aging well: processing speed inhibition and working memory related to balance and aerobic endurance. Geriatr Gerontol Int. (2017) 17:108–15. doi: 10.1111/ggi.12682
47. Yamazaki Y, Zhao N, Caulfield TR, Liu CC, Bu G. Apolipoprotein E and Alzheimer disease: pathobiology and targeting strategies. Nat Rev Neurol. (2019) 15:501–18. doi: 10.1038/s41582-019-0228-7
Keywords: cardiovascular risk, cognition, longitudinal study, older adult, national representative data set
Citation: Hua W, Hou J, Jiang T, Su B, Fu J, Sun R, Chang B, Xia W, Wu H, Zhang T, Guo C and Wang W (2020) The Longitudinal Association Between Cardiovascular Risk and Cognitive Function in Middle-Aged and Older Adults in China: A Nationally Representative Cohort Study. Front. Cardiovasc. Med. 7:560947. doi: 10.3389/fcvm.2020.560947
Received: 03 July 2020; Accepted: 11 September 2020;
Published: 19 October 2020.
Edited by:
Takatoshi Kasai, Juntendo University, JapanCopyright © 2020 Hua, Hou, Jiang, Su, Fu, Sun, Chang, Xia, Wu, Zhang, Guo and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen Wang, WW91YW5zdWlkMjAyMCYjeDAwMDQwO2hvdG1haWwuY29t; Caiping Guo, Z2NwZHQwMDEmI3gwMDA0MDsxMjYuY29t
†These authors share first authorship
 Wei Hua1†
Wei Hua1† Jianhua Hou
Jianhua Hou Bin Su
Bin Su Jiangning Fu
Jiangning Fu Hao Wu
Hao Wu Tong Zhang
Tong Zhang