- 1Department of Biomedical Sciences, Faculty of Science, University of Ngaoundere, Ngaoundere, Cameroon
- 2General Medicine Service, Ngaoundere Regional Hospital, Ngaoundere, Cameroon
- 3Hypertension and Diabetes Unit, Ngaoundere Regional Hospital, Ngaoundere, Cameroon
Background and Objectives: Recent and contextualized data are needed to improve hypertension management known as a major cardiovascular disease risk factor regardless of the geographical area. This study aimed at assessing the prevalence of hypertension, awareness of hypertensive status, treatment, and control of hypertension as well as assessing the factors associated with risk of hypertension and awareness of hypertensive status in the population of Ngaoundere.
Methods: This was a community based cross sectional study carried out from February to December 2016. A three-stage sampling method was used for recruitment of participants. Demographic, clinical, and biological data were collected and analyzed using Statistical Package for Social Sciences version 20.0. Statistical significance was set at P < 0.05.
Results: In total, 948 participants were included in the study. The overall prevalence of hypertension was 46.94% (n = 445). Fraction of hypertensive participants who were aware of their status was 36.85% (n = 164). Among them, 39 (23.78%) were getting treatment and the control rate of treated hypertensives was 30.56%. Age, marital status, family history of hypertension, overweight, and high serum triglyceride level were identified as independent predicting factors of hypertension, whereas female gender, age, personal history of stroke or diabetes, family history of hypertension or heart failure, overweight, and abdominal obesity were those of hypertension awareness.
Conclusion: The present study revealed high prevalence, extremely low awareness, treatment, and control rates of hypertension in Ngaoundere community setting.
Introduction
Hypertension is a major cardiovascular disease risk factor and its prevalence has shown a rapid increase in Sub-Saharan Africa (1–6). This prevalence can be substantially reduced through prevention, early diagnosis, and proper management. According to World Health Organization (WHO), recent and contextualized epidemiological data are needed for this purpose. However, cardiovascular disease estimates remain uncertain in low-income countries because of the scarcity of epidemiological studies in some areas (5–7). A previous study showed that hypertension is the most frequent encountered cardiovascular condition and the main cause of major cardiovascular events in Ngaoundere hospital setting (8). It is then possible to hypothesize that an important cardiovascular risk factor such as hypertension still yet not well managed, and that cardiovascular disease prevention remain a great public health challenge in this region. Clearly, lack of evidence data on cardiovascular disease risk factors worsens the situation, thus the need to improve availability of reliable epidemiologic data on cardiovascular disease in this area. This study aimed at assessing the prevalence of hypertension, awareness of hypertensive status, treatment, and control of hypertension as well as assessing the factors associated with risk of hypertension and awareness of hypertensive status in population of Ngaoundere in Cameroon.
Methods
Study Population and Selection Criteria
A community based cross sectional study was conducted from February to December 2016 in Ngaoundere, Cameroon. Ngaoundere is the chief town of Adamawa Region. It is located in the high altitude guinea savannah ecological zone and is characterized by one rainy season from April to October and one dry season from November to March. The Foulbes, the Haoussas, the Gbaya, the Tikar, the Mboum, and the Dii are the leading ethnic groups in the area. The main economic activities are dairy farming and agriculture. Participants were selected following a three-stage cluster sampling method, among people aged 20 years or above and who have been living in the study area for at least 1 year. Individuals on corticosteroid therapy, hormonal contraceptives, or presenting with chronic kidney disease were excluded. Details of sampling procedure are described in a previous work (9).
Study Variables
Demographic (sex, age, marital status), anthropometric (body mass index, waist circumference), clinical (medical history, blood pressure, awareness, treatment, and control of hypertension), and biological variables (fasting serum glucose, triglyceride, and total cholesterol levels) were studied. Overweight and obesity were defined as body mass index ranges 25–29.9 and >29.9 kg/m2, respectively (10). Abdominal obesity was defined as waist circumference >102 cm for men and 88 cm for women (10, 11). Hypertension was defined as blood pressure >140/90 mmHg at the time of study or antihypertensive therapy for at least 15 days (12, 13). All participants who answered yes to the question “are you suffering from hypertension?” Were considered as aware of hypertension. Hypertension was considered to be controlled in all treated hypertensive subjects who had at the time of the study a blood pressure <140/90 mmHg.
Diabetes was defined as fasting blood glucose >1.26 g/L (14), or a self-report of previous diagnosis of diabetes. National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults, Adult Treatment Panel III Criteria were used to define high serum triglyceride and total cholesterol levels (more than 200 mg/dL for triglycerides; more than 240 mg/dL for total cholesterol) (15).
Data Collection
Demographic data and medical history were collected using a semi-structured questionnaire. Following The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure recommendations, blood pressure was measured in participants on sitting position after at least 5 min of rest (12). The investigators also ensured that the participants had not consumed tobacco or caffeinated beverages, had not practiced physical activity for at least 30 min prior to blood pressure measurement (12). Blood pressure was measured using an electronic blood pressure monitor type OMROM® HEM-8712. Two measurements were made with a time lapse of 3–5 min and the mean of the two measures was used for analysis. Weight, height, and waist circumference measurements were done following the WHO STEPwise approach (10). A TIAN SHAN®-2003B brand electronic weigh scale, a local stadiometer, and a non-stretchable flexible graduated tape were, respectively, used for this purpose. Body mass index was calculated by dividing weight (in kilograms) by the square of height (in meters) (16). Blood samples were collected in each participant after 8–12 h overnight fast. From those samples, fasting blood glucose, triglyceride, and total cholesterol levels were estimated via colorimetric reactions and spectrophotometric readout (9).
Data Analysis
Data were analyzed using Statistical Package for Social Sciences version 20.0. Pearson's Chi-square and Fisher's exact tests were used to compare proportions. Univariate and multivariate logistic analyses were used to assess the crude and adjusted effect of seemingly significant predictors of hypertension and awareness of hypertension. A P < 0.05 was considered as statistically significant.
Ethical Considerations
The study was approved by the Ethical Committee of the University of Ngaoundere, the Local Ethical Committee (Reference no. 1121/L/RC/RA/DSP/HR/NGD/CLE) and the National Ethics Committee for Human Health Research. It was also approved by the Regional Delegate of Public Health for Adamawa Region (Reference no. 651/l/RA/DSP/SAG/BPF/NGD). Prior to individual data collection, each participant was clearly informed about the study and freely signed a written consent form.
Results
A total of 948 participants were included in the study, comprising 464 (48.95%) men and 484 (51.05%) women. Their mean age was 38.82 ± 14.92 years (range 20–87). Most of the participants were married (Table 1).
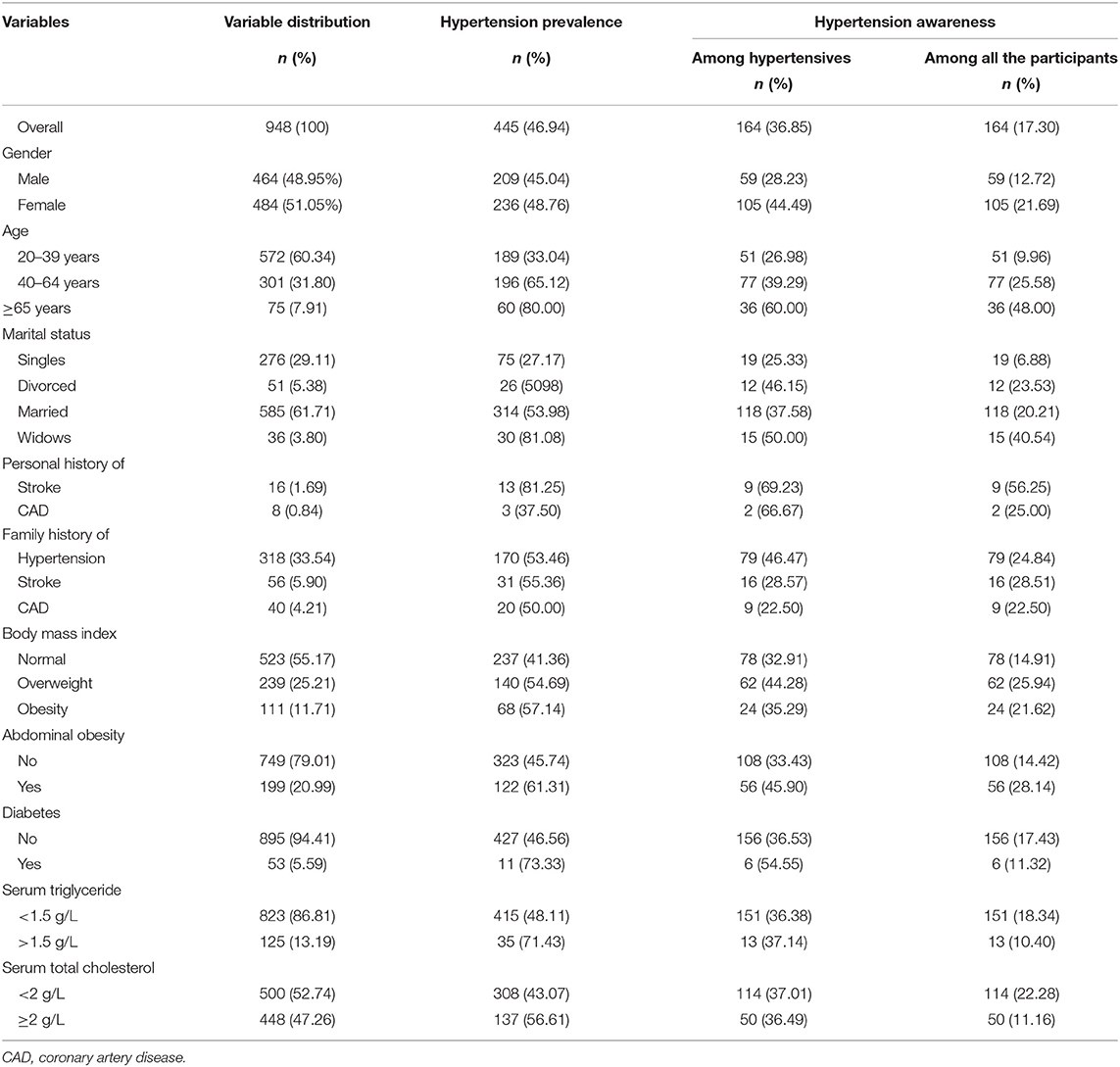
Table 1. Baseline characteristics of the study participants, hypertension prevalence, and awareness.
Hypertension Prevalence and Awareness
The overall prevalence of hypertension was 46.94% (n = 445) in the study population, 45.04% in men and 48.76% in women. Older participants and those with high body mass index had higher prevalence of hypertension than younger participants and those with lower body mass index. Diabetic participants and those having a personal history of stroke, a family history of hypertension, abdominal obesity, high serum triglyceride, and total cholesterol levels recorded higher prevalence of hypertension than their counterparts (Table 1).
A proportion of 36.85% of hypertensive participants (17.30% of whole study population) were aware of their status. Women were more aware of their hypertensive status than men (44.49 vs. 28.23%). Moreover, older participants were more aware of their status than youngers (Table 1).
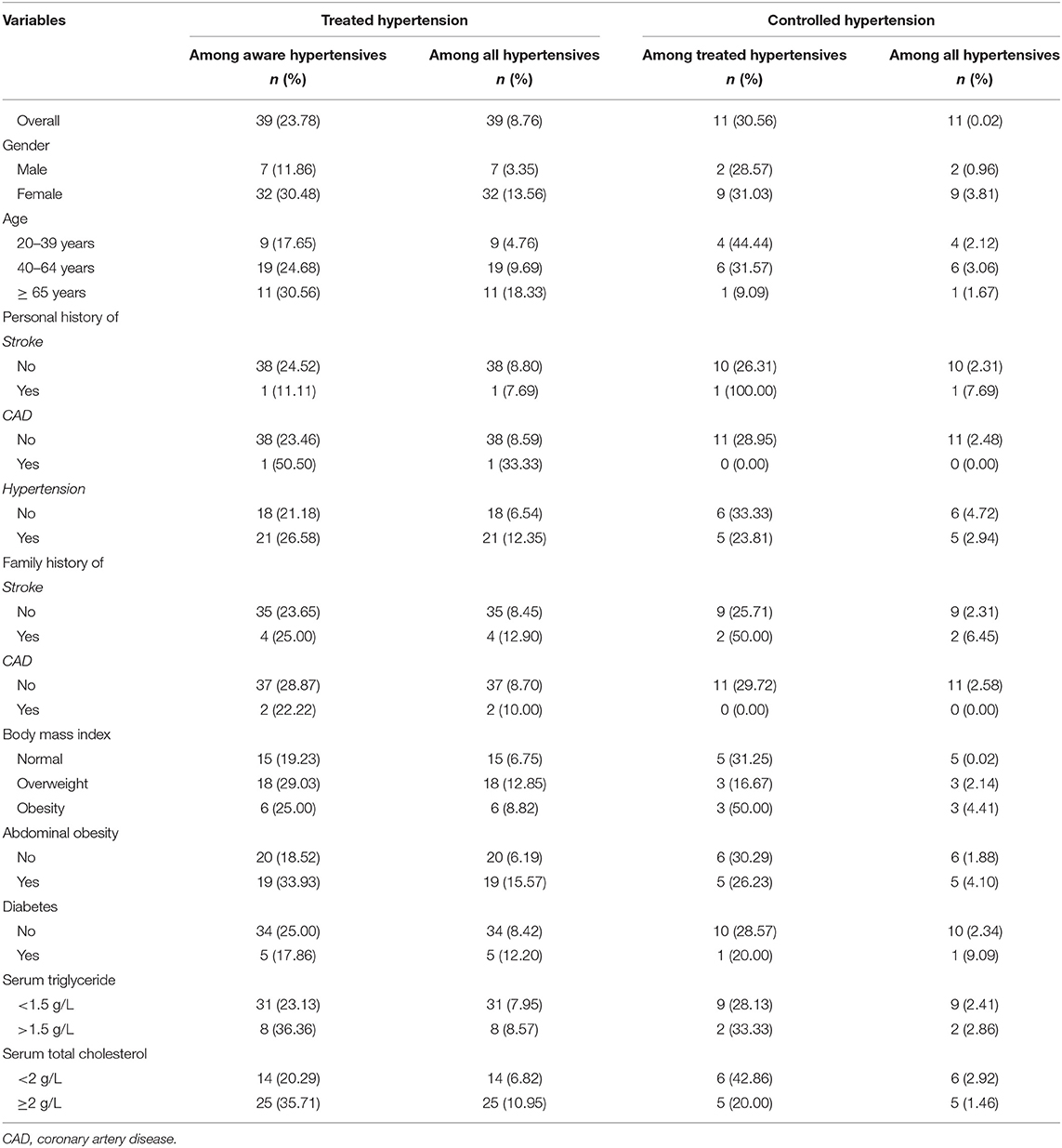
Hypertension Treatment and Control
A total of 39 (23.78%) aware hypertensive participants were on blood pressure lowering medication. So, only 8.76% of all the hypertensive participants were treated. The use of drug treatment for hypertension was higher among women than men (30.48 vs. 11.86%). It was also higher in older participants than youngers. Similarly, it was higher in hypertensive participants with a personal or family history of coronary artery disease and in those with abdominal obesity than those without (Table 2).
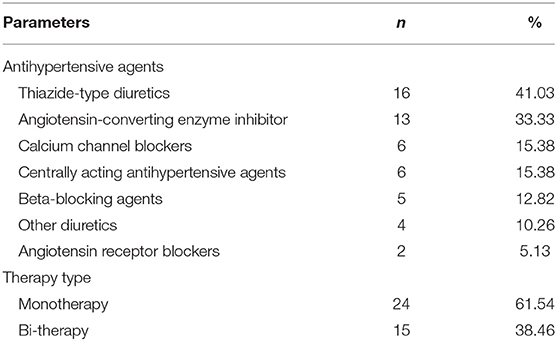
Thiazide-type diuretics and angiotensin-converting enzyme inhibitors were the most frequent antihypertensive agent used for hypertension treatment in the study population. These drug classes were used by 41.03% (n = 16) and 33.33% (n = 13) of the treated hypertensive participants, respectively. The least used antihypertensive agent was angiotensin receptor blockers (Table 3).
The hypertension control rate was 30.56% (n = 11) among treated hypertensives and 0.02% among the overall hypertensive participants. The level of blood pressure control was higher in women (31.03%) than in men (28.57%). It was also higher in participants with personal or family history of stroke than those without (Table 2).
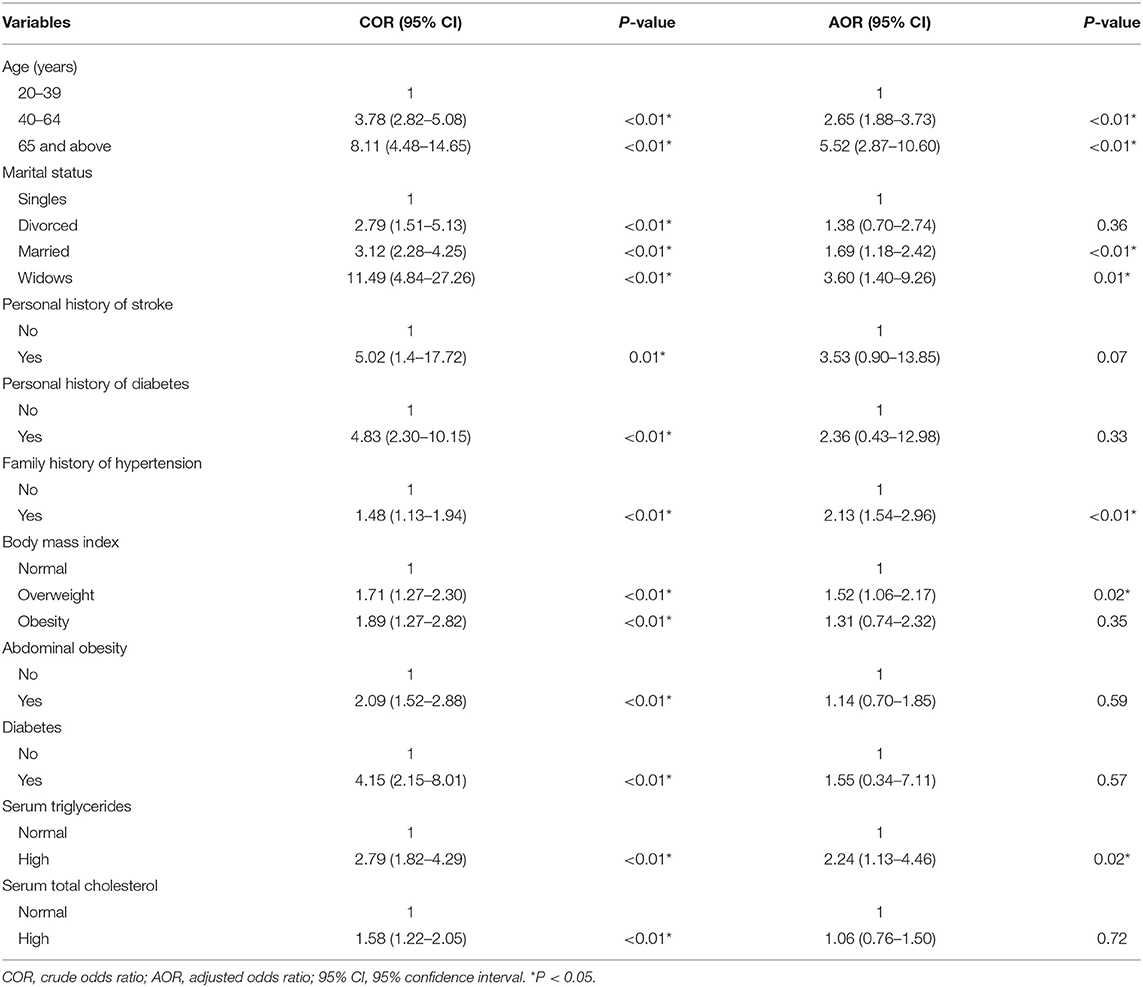
Factors Associated With Hypertension
The association of independent variables with hypertension was investigated using both univariate and multivariate logistic regression techniques. In univariate logistic regression analysis; age, gender, marital status, personal history of stroke or diabetes, family history of hypertension, body mass index, waist circumference, diabetes, serum triglyceride, and total cholesterol levels showed significant associations with hypertension (Table 4). Therefore, all those variables were used in multivariate analysis, which showed that age, marital status and family history of hypertension, body mass index, and serum triglyceride level were independently associated with the odds of having hypertension. Participants aged ≥ 65 years and those aged 40–64 years were five times (AOR = 5.52; P < 0.01) and two times (AOR = 2.65; P < 0.01), respectively, more likely to present hypertension than those aged 20–39 years (Table 4).
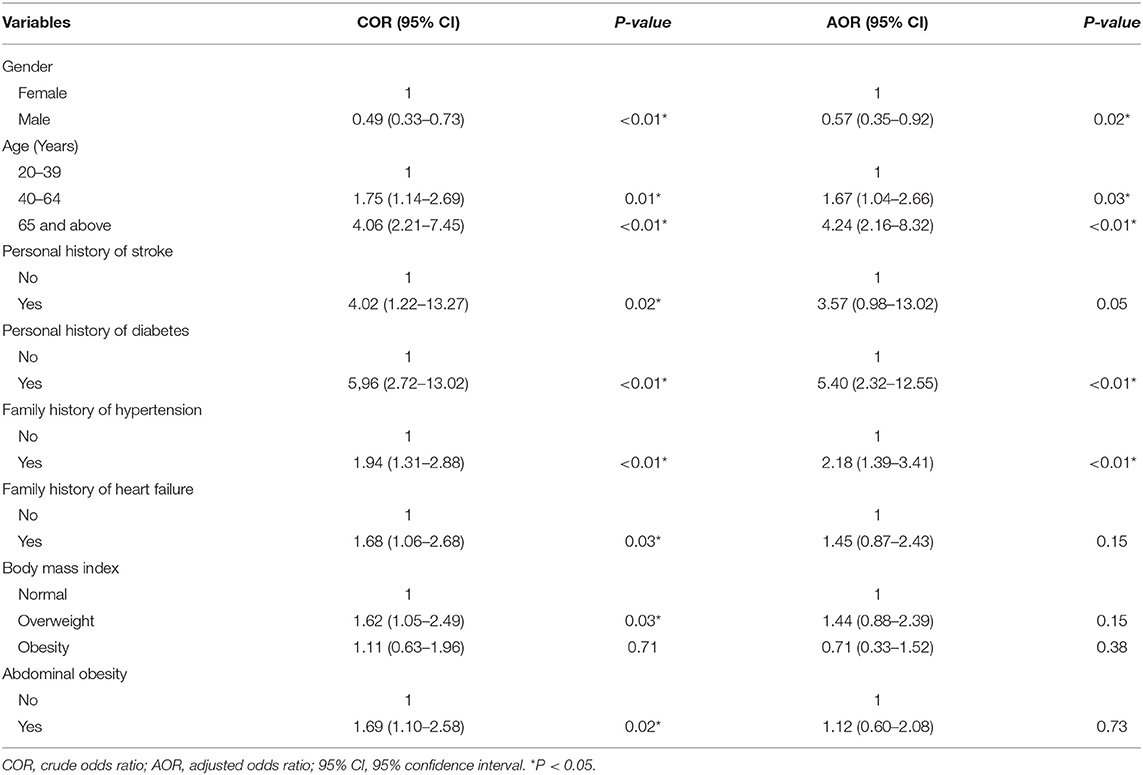
Factors Associated With Hypertension Awareness
In univariate logistic regression analysis, female gender, age, personal history of stroke or diabetes, family history of hypertension or heart failure, body mass index, and abdominal obesity showed significant associations with hypertension awareness (Table 5). Those factors were then used in multivariate logistic regression analysis, which revealed that female gender, age, personal history of diabetes, and family history of hypertension were independently associated with hypertension awareness. Thus, female participants were more likely to be aware of their hypertensive status than males (AOR = 0.49; P = 0.02). Moreover, Participants aged ≥ 65 years were four times (AOR = 4.24; P < 0.01) more likely to be aware of their hypertensive status than those aged 20–39 years (Table 5).
Discussion
The main findings of this study are the higher prevalence of hypertension and its significant association with age and marital status, the lower hypertension awareness, treatment, and control in Ngaoundere urban community. These findings highlight the importance of reliable data in the hypertension prevention and control process in our setting. Bearing in mind the higher but not currently apparent prevalence of hypertension, it is necessary to consider hypertension as a huge public health problem in this region.
Hypertension Prevalence and Associated Factors
The prevalence of hypertension is gradually increasing in sub-Saharan Africa (17, 18). In this region, the prevalence of hypertension increased from 19.7 to 30.8% between 1990 and 2010 (19). Recent studies indicate a prevalence of hypertension among adult subjects close to 45% in African urban areas. Hypertension prevalence rates of 38.9, 45.2, 47, and 41.4%, have been reported in similar study populations in South Africa (20), Angola (21), Nigeria (22), and Democratic Republic of Congo (23), respectively. The 46.94% prevalence rate of hypertension found in the study is close to those reported in many other African countries, but higher as compared to those reported in higher-income countries for similar age group populations (2, 24), suggesting an influence of income level in the prevention and treatment of cardiovascular diseases. In Israel for example, the well-developed health system including national health insurance coverage have substantially increased access to treatment for the low income groups and so, have improved the prevention and control of hypertension (24).
Results of the study indicated that age, marital status and family history of hypertension, body mass index, and serum triglyceride level were factors independently associated with the odds of having hypertension.
Age has been identified as a determinant of blood pressure level (3, 6, 20, 24–26). In the present study, the prevalence of hypertension was 33.04% in participants aged 20–39 years, 65.12% in subjects aged 40–64 years and 80.00% in subjects aged 65 years and above. Moreover, multivariate analysis showed that participants aged ≥ 65 years and those aged 40–64 years were more likely to have hypertension than those aged 20–39 years. These results are consistent with those of previous studies and confirm the relationship between age and hypertension (24–26).
There was also a significant association between hypertension and marital status. Multivariate analysis showed that married and widowed participants were more likely to be hypertensive than single participants. This association could be explained by the influence of age, assuming that widows are commonly older than marrieds, whom are commonly older than singles. Marital status has previously shown association with hypertension (24, 27, 28), being married affecting lifestyle, health-related behaviors, psychosocial support and adherence to dietary advice, and medical treatment (24, 29). However, level and direction of the effect differ from a study to another, being sometimes conflicting. Marriage failure have been said to inflict a great psychological stress, which is involved in increasing the risk of having hypertension (27). In a multicenter study carried out in six adjacent Middle Eastern Gulf countries, Hadi Khafaji et al. found that widowed marital status was associated with a higher cardiovascular risk profile (29). Contrariwise, marriage have been described by other authors as factor mitigating or exacerbating exposure to cardiovascular risk factors in some societies (24, 28). Analyzing data from two Japanese representative surveys that are the Comprehensive Survey of Living Conditions (CSLC) and the National Health and Nutritional Survey (NHNS), Fukuda and Hiyoshi noticed sex difference in the association between marital status and cardiovascular risk factors. They found that being married was associated with lower prevalence of cardiovascular risk factors among men and with higher prevalence of obesity, hypertension, and multiple risk factors among women (28). All these contradictions attest that the influence of marital status on arterial hypertension and cardiovascular risk factors need to be more specifically explored and explained.
Regarding family history of hypertension and body mass index, the results of the study showed that participants who reported a family history of hypertension were two times (p < 0.01) more susceptible to be hypertensive than those who did not. Similarly, overweight participants were 1.52 (p = 0.02) times more at risk of hypertension than those whose body mass indexes were equal to 25 kg/m2 or lower. The association of the two variables with hypertension is consistent with results of Wang et al. (2), Peer et al. (20), and Hammami et al. (25), suggesting that, there may be a single or combined effect of genetic and lifestyle factors in the genesis and the progression of high blood pressure.
The prevalence of hypertension was significantly higher in subjects with personal history of stroke than in those without (81.25 vs. 46.35%; p = 0.01). Although, this association appeared only in univariate analysis in the present study, hypertension is known to be a major risk factor for stroke (20, 25, 30). A study carried out in the United States showed that 77% of first-time stroke victims had high blood pressure (30). Another study carried out in South Africa indicated that the risk of being hypertensive was five times higher for patients suffering from stroke compared to others (31). Presented results are in line with these observations.
Hypertension Awareness and Associated Factors
The importance of hypertension awareness toward its treatment and control is unquestionable, as awareness is the first stage of any disease management process. In resources-constrain settings, factors like misperceptions and lack of sensitization tend to alter people level of awareness (23, 31). Usually in the study area, people with high blood pressure do not express the need for management until complications occur. In this context, even blood pressure checkup for early high blood pressure detection is not frequent; people and stakeholders seeming disarrayed by infectious diseases. This could justify the low proportion of participants aware of their hypertensive status in the present study. The 36.85% proportion of participants aware of their status is lower than those reported in most of western countries (24, 32, 33). This difference could be explained by numerous economic and social facilities used to enhance sensitization, to carry out screenings, and to manage high blood pressure in western countries (1, 34, 35).
Hypertension Treatment and Control
For better control of blood pressure, awareness is never sufficient if not followed by good therapeutic approach and follow-up. In our context, the management of hypertensive patients still a major challenge for caregivers as well as for the whole population. Presented results showed that 23.78% of aware hypertensive participants were using blood pressure lowering drugs. This fraction is close to the 30.5% reported in the VITARAA study (23), but it remains low as compared to that of western countries. Several factors may explain the low fraction of participants on antihypertensive treatment. Studies in low-income countries have shown that the high cost of drugs may be associated with the lack of treatment in known hypertensive patients (36–38). In our environment, low-cost antihypertensive (generic) drugs supply is not constant in public health facilities and some hypertensive patients are not able to buy their medicines all the times compromising therefore the better control of their blood pressure. Other factors such as lack of health insurance coverage for almost the entire population, local beliefs could explain low treatment rate observed (35, 36, 39).
For the treatment of hypertension, thiazide-type diuretics and angiotensin-converting enzyme inhibitors were the most frequently used antihypertensive agents in the study. The first group were used by 41.03% of the treated hypertensive participants and the second by 33.33%. These results are consistent with updated hypertension management recommendations (13, 40). This could be explained by the availability of some of these antihypertensive agents in generic form and the prescribing habits of general practitioners in our setting. Although calcium channel blockers have been shown to be one of the most effective antihypertensive agents in general black population (13), this group of drugs was not the most frequently used. In our context, nifedipine (10 mg short-acting nifedipine) still the common calcium channel blocker available in public health care facilities. Its principal mechanisms of action are peripheral and coronary vasodilation (41). Its harmful clinical effects include proischemic effect, complex ventricular tachyarrhythmias, Prohemorrhagic Effects, and marked hypotension (41). These side effects probably limit its current use for long term treatment of hypertension. Angiotensin receptor blockers were the least used (5.13%, n = 2), probably because of the high cost of this group of drugs.
The 28.21% hypertension control rate reported among treated hypertensive participants in the study was close to that of 24.6% reported by Dzudie et al. (3), but higher than those of 9.4% and 13.6% reported by Musinguzi and Nuwaha (6) and Katchunga et al. (23), respectively. The last two studies participants were recruited both in rural and urban area. In resource-constrain countries, rural areas are usually characterized by scarcity and remoteness of health facilities, very low resources, and poor level of education of the population. These factors may limit hypertension management and control thus, justifying the observed differences. The low hypertension control rate observed in the town of Ngaoundere may be due to the fact that people habitually put in competition traditional and modern medicine approaches of disease management. Nevertheless, the health facilities/population ratio is still low in this community and, there is a need to improve both medical staff training and health facilities technical platform for a better prevention and management of cardiovascular diseases.
Strengths and Limitations
The present study is the first to analyze at one time data on the prevalence, awareness, and treatment of hypertension in a community setting in Ngaoundere. However, some limitations should be mentioned: the prevalence of hypertension was based on single blood pressure measurement and, treatment of hypertension was restricted to the use of antihypertensive agents, without consideration of non-pharmaceutical therapeutic strategies such as lifestyle modifications. Dietary factors and physical activity are important in pathogenesis and prevention of hypertension, but these were not assessed in the study. Moreover, it is known that economic factors play a significant role in access to health care especially in poor countries. Economic status of participants were not assessed in this study. In consequence, it was not possible to determine whether the participants who were aware and were on treatment had a better economic status or not.
Conclusion
The present study revealed a high prevalence of hypertension and very low awareness, treatment, and control rates of this cardiovascular disease risk factor in Ngaoundere urban community. Further research is needed to identify various other factors associated with hypertension prevalence, awareness and control in resource – constrained African societies.
Data Availability
All datasets analyzed for this study are included in the manuscript.
Ethics Statement
Local Ethics Committee for Human Health Research, Reference no. 1121/L/RC/RA/DSP/HR/NGD/CLE. All the participants freely consented to participate in the study, after information and explanation given to them by the investigator.
Author Contributions
OM contributed to the conception and study design, data interpretation, drafting of the manuscript, and approval of the final manuscript. TN contributed to the data collection and interpretation, drafting of the manuscript, and approval of the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors express their heartfelt gratitude to all the study participants. Their acknowledgment extends to community health agents and district heads who helped mobilizing and communicating well with participants.
References
1. Doulougou B, Kouanda S, Ouédraogo GH, Meda BI, Bado A, Zunzunegui MV. Awareness, treatment, control of hypertension and utilization of health care services following screening in the north central region of Burkina Faso. Pan Afr Med J. (2014) 19:259. doi: 10.11604/pamj.2014.19.259.4707
2. Wang J, Zhang L, Wang F, Liu L, Wang H. Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens. (2014) 27:1355–61. doi: 10.1093/ajh/hpu053
3. Dzudie A, Kengne A P, Muna W F T, Hamadou Ba, Menanga A, Kouam Kouam C, et al. Prevalence, awareness, treatment and control of hypertension in a self-selected sub-Saharan African urban population: a cross-sectional study. BMJ Open. (2012) 2:e001217. doi: 10.1136/bmjopen-2012-001217
4. Arabzadeh S, Sadeghi M, Rabiei K, Sarrafzadegan N, Taheri L, Golshahi J. Determinants of uncontrolled hypertension in an Iranian population. ARYA Atheroscler. (2014) 10:25–31.
6. Musinguzi G, Nuwaha F. Prevalence, awareness and control of hypertension in Uganda. PLoS ONE. (2013) 8:e62236. doi: 10.1371/journal.pone.0062236
8. Pancha OM, Ngoufack JO, Koona KA, Falmata M, Kingue S. Place et profil évolutif des maladies cardiovasculaires en milieu hospitalier nord camerounais: Le Cas de L'Hôpital Régional de Ngaoundéré. Health Sci Dis. (2015) 16:1–7. Available online at: https://www.hsd-fmsb.org/index.php/hsd/article/view/470/pdf_240
9. Ngoufack JOT, Mbouemboue OP, Sakinatou I, Velinga AC, Tamanji TM, Koona Koona JA. Association between blood pressure, waist circumference, cholesterolaemia and triglyceridaemia in a population of cameroonian adults. Res J Health Sci. (2017) 5:27–35. doi: 10.4314/rejhs.v4i4.4
10. WHO. Noncommunicable Diseases and Mental Health Cluster. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance/Noncommunicable Diseases and Mental Health. Geneva: World Health Organization. (2005). Available online at: http://www.who.int/iris/handle/10665/43376
11. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren WMM, et al. European guidelines on cardiovascular disease prevention in clinical practice (version 2012). Eur Heart J. (2012) 33:1635–701. doi: 10.1093/eurheartj/ehs254
12. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. (2003) 289:2560–72. doi: 10.1001/jama.289.19.2560
13. James PA, Oparil S, Carter BL, Cushman WC, Himmelfarb CD, Handler J, et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA. (2014) 2013:E1–14. doi: 10.1001/jama.2013.284427
14. American Diabetes Association. Classification and Diagnosis of Diabetes. Diab Care. (2017) 40(Suppl 1):S11–24. doi: 10.2337/dc17-S005
15. Grundy SM, Becker D, Clark LT, Cooper RS, Denke MA, Howard J, et al. Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III): final report. Circulation. (2002) 106:3143. doi: 10.1161/circ.106.25.3143
16. Eknoyan G. Adolphe Quetelet (1796–1874)-the average man and indices of obesity. Historical note. Nephrol Dial Transplant. (2008) 23:47–51. doi: 10.1093/ndt/gfm517
17. Nejjari C, Arharbi M, Chentir M-T, Boujnah R, Kemmoue O, Megdiche H, et al. Epidemiological Trial of Hypertension in North Africa (ETHNA): an international multicentre study in Algeria, Morocco and Tunisia. J Hypertens. (2013) 31:49–62. doi: 10.1097/HJH.0b013e32835a6611
18. Steichen O. Hypertension artérielle du sujet noir (monographie). La revue du praticien. (2010) 60:654–9. Available online at: www.larevuedupraticien.fr
19. Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. PLoS ONE. (2014) 9:e104300. doi: 10.1371/journal.pone.0104300
20. Peer N, Steyn K, Lombard C, Gwebushe N, Levitt N. A high burden of hypertension in the urban black population of Cape Town: the cardiovascular risk in black South Africans (CRIBSA) study. PLoS ONE. (2013) 8:e78567. doi: 10.1371/journal.pone.0078567
21. Capingana DP, Magalhães P, Silva ABT, Gonçalves MAA, Baldo MP, Rodrigues SL, et al. Prevalence of cardiovascular risk factors and socioeconomic level among public-sector workers in angola. BMC Public Health. (2013) 13:732. doi: 10.1186/1471-2458-13-732
22. Ekanem US, Opara DC, Akwaowo CD High blood pressure in a semi-urban community in south-south Nigeria: a community–based study. Afr Health Sci. (2013) 13:56–61. doi: 10.4314/ahs.v13i1.8
23. Katchunga PB, M'Buyamba-Kayamba J-R, Masumbuko B E, Lemogoum D, Kashongwe Z M, Degaute J-P, et al. Hypertension artérielle chez l'adulte congolais du sud kivu: résultats de l'étude vitaraa. Presse Med. (2011) 40:e315–23. doi: 10.1016/j.lpm.2010.10.036
24. Abu-Saad K, Chetrit A, Eilat-Adar S, Alpert G, Atamna A, Gillon-Keren M, et al. Blood pressure level and hypertension awareness and control differ by marital status, sex, and ethnicity: a population-based study. Am J Hypertension. (2014) 27:1511–20. doi: 10.1093/ajh/hpu081
25. Hammami S, Mehri S, Hajem S, Koubaa N, Frih1 MA, Kammoun S, et al. Awareness, treatment and control of hypertension among the elderly living in their home in Tunisia. BMC Cardiovasc Disord. (2011) 11:1–7. doi: 10.1186/1471-2261-11-65
26. Katte J-C, Dzudie A, Sobngwi E, Mbong EN, Fetse GT, Kouam Kouam C, et al. Coincidence of diabetes mellitus and hypertension in a semi-urban Cameroonian population: a cross-sectional study Katte et al. BMC Public Health. (2014) 14:696. doi: 10.1186/1471-2458-14-696
27. Tucker WI. Psychiatric factors in essential hypertension. N Engl J Med. (1950) 243:211–5. doi: 10.1056/NEJM195008102430602
28. Fukuda Y, Hiyoshi A. Associations of household expenditure and marital status with cardiovascular risk factors in Japanese adults: analysis of nationally representative surveys. J Epidemiol. (2013) 23:21–7. doi: 10.2188/jea.JE20120021
29. Hadi Khafaji HA, Al Habib K, Asaad N, Singh R, Hersi A, Al Falaeh H, et al. Marital status and outcome of patients presenting with acute coronary syndrome: an observational report. Clin Cardiol. (2012) 35:741–8. doi: 10.1002/clc.22034
30. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2015 update: a report from the American Heart Association. Circulation. (2015) 131:e29–322. doi: 10.1161/CIR.0000000000000350
31. Peltzer K, Phaswana-Mafuy AN. Hypertension and associated factors in older adults in South Africa. Cardiovasc J Afr. (2013) 24:66–71. doi: 10.5830/CVJA-2013-002
32. Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. (2009) 27:963–75. doi: 10.1097/HJH.0b013e3283282f65
33. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. (2010) 303:2043–50. doi: 10.1001/jama.2010.650
34. Bovet P, Gervasoni JP, Mkamba M, Balampama M, Lengeler C, Paccaud F. Low utilization of health care services following screening for hypertension in Dar es Salaam (Tanzania): a prospective population-based study. BMC Public Health. (2008) 8:407. doi: 10.1186/1471-2458-8-407
35. Mendis S, Abegunde D, Oladapo O, Celletti F, Nordet P. Barriers to management of cardiovascular risk in a low resource setting using hypertension as an entry point. J Hypertens. (2004) 22:5964. doi: 10.1097/01.hjh.0000098150.70956.af
36. Pancha OM; Yiagnigni E, Koona KA, Cacko J, Ndobo P. Determinants of hypertension awareness and treatment among patients under cardiology follow up in a Cameroonian Regional Hospital. Int J Collab Res Intern Med Public Health. (2012) 4:1663–72. Available online at: core.ac.uk
37. Dennis T, Meera NK, Binny K, Sekhar MS, Kishore G, Sasidharan S. Medication adherence and associated barriers in hypertension management in India. CVD Prev Control. (2011) 6:9–13. doi: 10.1016/j.cvdpc.2010.11.001
38. Meng XJ, Dong GH, Wang D, Liu MM, Lin Q, Tian S, et al. Prevalence, awareness, treatment, control, and risk factors associated with hypertension in urban adults from 33 communities of China: the CHPSNE study. J Hypertens. (2011) 29:1303–10. doi: 10.1097/HJH.0b013e328347f79e
39. Ekman B. Community-based health insurance in low-income countries: a systematic review of the evidence. Health Policy Plann. (2004) 19:249–70. doi: 10.1093/heapol/czh031
40. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. (2017) 71:1269–324. doi: 10.1161/HYP.0000000000000066
Keywords: Ngaoundere, Cameroon, hypertension, prevalence, awareness, treatment, control
Citation: Mbouemboue OP and Ngoufack TJO (2019) High Blood Pressure Prevalence, Awareness, Control, and Associated Factors in a Low-Resource African Setting. Front. Cardiovasc. Med. 6:119. doi: 10.3389/fcvm.2019.00119
Received: 29 April 2019; Accepted: 05 August 2019;
Published: 30 August 2019.
Edited by:
Elsayed Z. Soliman, Wake Forest School of Medicine, United StatesReviewed by:
Mohamed Faher Almahmoud, Medical University of South Carolina, United StatesMuhammadImtiaz Ahmad, Wake Forest Baptist Medical Center, United States
Copyright © 2019 Mbouemboue and Ngoufack. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tsougmo Jacques Olivier Ngoufack, bmdvdWZhY2t0c291Z21vQHlhaG9vLmZy; Olivier Pancha Mbouemboue, b2xpdmllcl9wYW5jaGFAeWFob28uZnI=
 Olivier Pancha Mbouemboue
Olivier Pancha Mbouemboue Tsougmo Jacques Olivier Ngoufack
Tsougmo Jacques Olivier Ngoufack