
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Cardiovasc. Med. , 23 May 2018
Sec. Structural Interventional Cardiology
Volume 5 - 2018 | https://doi.org/10.3389/fcvm.2018.00040
 Micha T. Maeder1*
Micha T. Maeder1* Lukas Weber1,2
Lukas Weber1,2 Marc Buser
Marc Buser Marc Gerhard
Marc Gerhard Philipp K. Haager
Philipp K. Haager Francesco Maisano3
Francesco Maisano3 Hans Rickli1
Hans Rickli1In patients with aortic and/or mitral valve disease the presence of pulmonary hypertension (PH) indicates a decompensated state of the disease with left ventricular and left atrial dysfunction and exhausted compensatory mechanism, i.e., a state of heart failure. Pulmonary hypertension in this context is the consequence of the backwards transmission of elevated left atrial pressure. In this form of PH, pulmonary vascular resistance is initially normal (isolated post-capillary PH). Depending on the extent and chronicity of left atrial pressure elevation additional pulmonary vascular remodeling may occur (combined pre- and post-capillary PH). Mechanical interventions for the correction of valve disease often but not always reduce pulmonary pressures. However, the reduction in pulmonary pressures is often modest, and persistent PH in these patients is common and a marker of poor prognosis. In the present review we discuss the pathophysiology and clinical impact of PH in patients with aortic and mitral valve disease, the comprehensive non-invasive and invasive diagnostic approach required to define treatment of PH, and recent insights from mechanistic studies, registries and randomized studies, and we provide an outlook regarding gaps in evidence, future clinical challenges, and research opportunities in this setting.
In patients with left heart disease, the presence of pulmonary hypertension (PH) is an important feature as it represents a marker of more advanced disease and poor prognosis (1). Pulmonary hypertension due to left heart disease (group 2 PH) is the by far most common type of PH, and valve disease is the leading cause (2). Independent of symptoms the presence of PH in patients with valve disease indicates a decompensated state of the disease with left ventricular (LV) and left atrial (LA) dysfunction and exhausted compensatory mechanism, i.e., a state of chronic heart failure (HF) with a propensity for acute exacerbations, e.g., in the context of arrhythmia or volume challenges. In the present article, we review the epidemiology and pathophysiology of PH in aortic and mitral valve disease and the diagnostic and therapeutic approach in these patients, and we provide considerations regarding future clinical challenges and research opportunities in this setting.
Pulmonary hypertension in patients with left-sided valve disease is a consequence of valve disease and its impact on LV and LA function respectively and belongs to group 2 PH (3, 4). By definition this PH group is characterized by a mean pulmonary artery pressure (PAP, mPAP) ≥25 mmHg and a mean pulmonary capillary wedge pressure (mPAWP) >15 mmHg (4). In Table 1, a simplified version of the current PH classification (4) with the position of group 2 PH and in particular PH in valve disease is provided. Notably, group 2 PH is the only post-capillary form of PH. As discussed below the PH subgroups 2.1 to 2.3. cannot not be separated completely when discussing PH in the context of valve disease. As also discussed below there are patients who have two disease entities, i.e., valve disease and a form of PH not related to valve disease (i.e., non-group 2 PH).
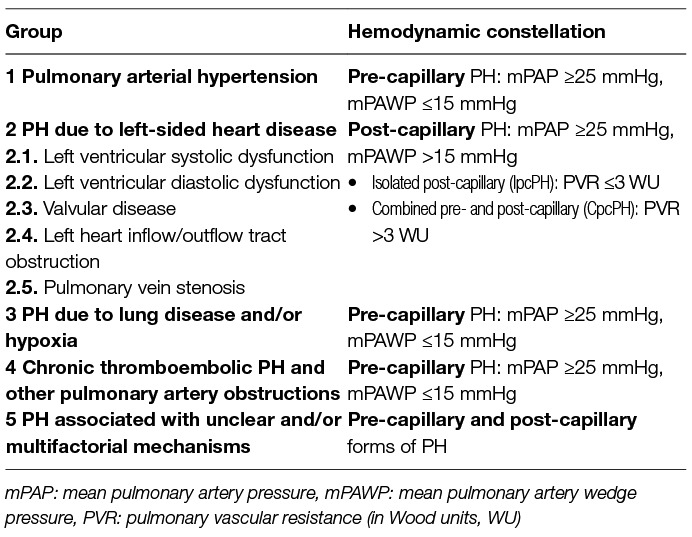
Table 1. Classification of pulmonary hypertension (PH) [according to Galie et al. (3)].
The prevalence of PH in patients with aortic and mitral valve disease depends on the type and severity of valve disease, the associated LV and LA dysfunction as well as other patient characteristics including age and cardiac rhythm and the method of PAP assessment. Direct measurement of mPAP by right heart catheterization (RHC), which is required for an exact diagnosis of PH, was performed in the minority of studies. The majority of data on the prevalence and prognostic impact of PH in valve disease are derived from echocardiographic studies where systolic PAP (sPAP) was estimated based on the peak tricuspid regurgitation velocity (TRV) using the Bernoulli equation. Many studies in the context of valve disease have defined significant PH as a sPAP ≥50 (TRV≈3.5 m/s) or ≥60 (TRV≈3.9 m/s) mmHg (Table 2). Independent of the presence or absence of additional echocardiographic signs of significant PH [such as right ventricular (RV) dilatation and/or dysfunction, D-shape of the left ventricle, shortened pulmonary acceleration time] these cut-offs are indicators of a high probability of PH and are associated with high specificity (4).
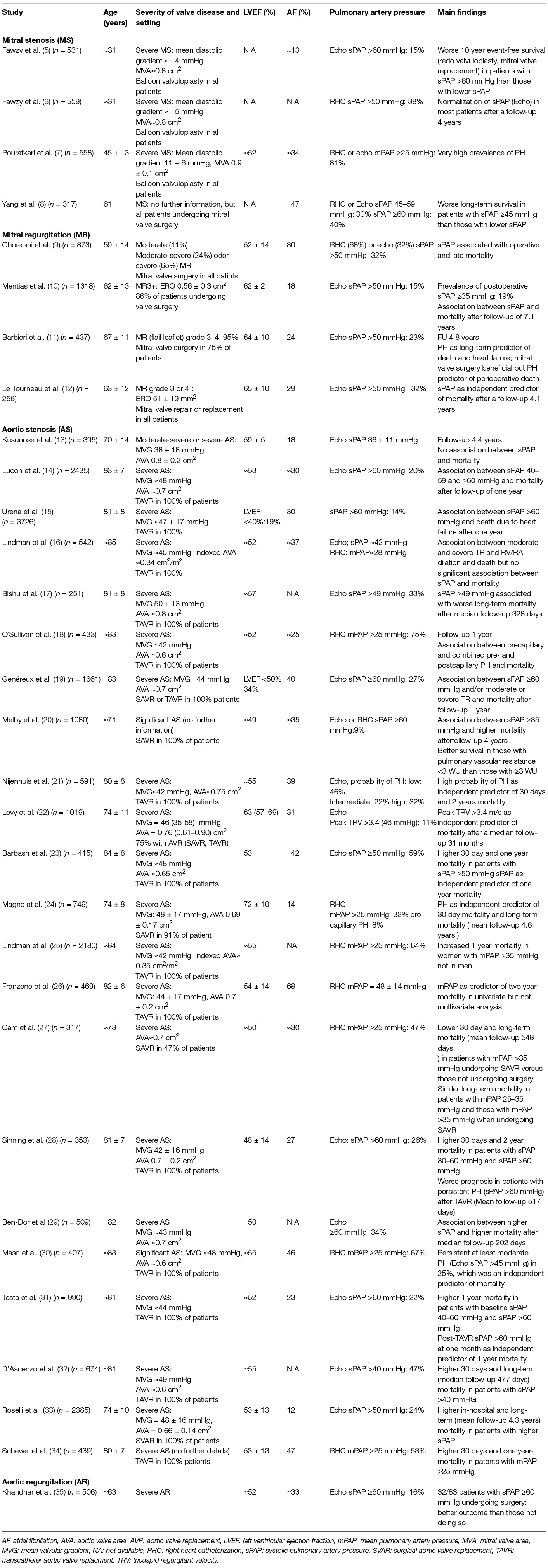
Table 2. Contemporary studies on the prevalence and prognostic impact of pulmonary hypertension (PH) in patients with aortic or mitral valve disease.
In Table 2, important contemporary studies on the prevalence of PH in aortic and mitral valve are summarized (5–35). In patients with mitral stenosis (MS), 30–40% of patients undergoing valve replacement or valvuloplasty have substantial PH (systolic PAP > 50–60 mmHg by echocardiography or mean PAP > 40 mmHg by RHC). In series of patients with moderate or severe mitral regurgitation (MR) undergoing valve surgery early after the echo or later during follow-up in the majority of cases, a prevalence of PH defined as sPAP >50 mmHg was found in 15–32% of patients. For patients with aortic regurgitation (AR) there is very little data. One study found a prevalence of 16% of PH defined as sPAP 60 ≥ mmHg in a cohort of patients with severe AR (35). In patients with AS the prevalence of PH is high, particularly in the elderly. Up to 75% of patients with severe AS undergoing TAVR were found to have PH as assessed by RHC. In echo studies, the prevalence of sPAP >60 mmHg or ≥60 mmHg varied between 9 and 34%.
With the exception of the relatively rare cases of patients with valve disease who have a second disease unrelated to valve disease and therefore do not have group 2 PH, the primary mechanism of elevated PAP in patients with left heart disease is the backward transmission of an elevated LA pressure (LAP) (3). The latter can be estimated by measurement of PAWP by RHC since direct access to the LA is not possible. It has to be realized however that there are some patients in whom PAWP does not reflect LAP: those with pulmonary veno-occlusive disease (high PAWP, normal LAP, obstruction of pulmonary venules) and those pulmonary vein stenosis (high PAWP, normal LAP). In MS and MR, valve disease has direct impact on the LA, whereas in aortic stenosis (AS) and AR the LA is affected indirectly by LV dysfunction. Many patients in whom criteria for severe AS, AR, or MR are clearly met, do not have an elevated PAWP however. The latter only occurs if the compensatory mechanism (LV and LA dilatation and function) are exhausted and/or if there is significant hypervolemia. Elevation of LAP is the result of LV systolic [reduced left ventricular ejection fraction (LVEF), reduced strain] and diastolic dysfunction (impaired relaxation and increased passive stiffness) and LA dysfunction (reduced compliance and booster function). Details of specific valve diseases are discussed below. A general principle however applies for the pathophysiology of PH in all types of left heart and left-sided valve diseases: initially PH is a purely passive phenomenon with a high LAP and PAWP but low transpulmonary gradient (difference between mPAP and mPAWP) and low pulmonary vascular resistance (quotient of transpulmonary gradient and cardiac output; isolated post-capillary PH, IpcPH). However, recurrent and chronic LAP elevation can cause alveolar stress failure and eventually pulmonary vascular remodeling with the development of a pulmonary vascular component of PH as reflected by an elevation of transpulmonary gradient and pulmonary vascular resistance respectively (combined pre-capillary and post-capillary PH, CpcPH) (1, 36, 37). Little is known about the exact mechanisms underlying this process; it is suspected that similar mechanisms and mediators play a role as in the pathobiology of pulmonary arterial hypertension (36, 37). Recent post-mortem data from well characterized patients with HF with reduced LVEF (HFrEF) and HF with preserved LVEF (HFpEF] without significant underlying or associated valve disease have revealed that pulmonary vascular remodeling is global but that the hemodynamic severity of PH is primarily related to remodeling of pulmonary venules (38). Similarly to other forms of PH valve-disease related PH can lead to RV dilatation and dysfunction and secondary tricuspid regurgitation but the clinical presentation can vary significantly (LV phenotype – the more common situation – versus RV phenotype) (36). In addition, we have to consider that the cardiac chambers and pulmonary circulation not only work in series (although we will in the following use such a schematic presentation) but that direct interactions on the ventricular and atrial level occur via septum. For instance, there is evidence from patients with MR that LV-RV interactions may play a role in the pathophysiology of RV dysfunction independently of PH (39).
In this paragraph, the general principles of the diagnostic approach are discussed, whereas the specific aspects for each valvular lesion are discussed below in the respective sections. The two basic questions in this context are the following ones: First, is PH present? Second, is the valve disease and consecutive cardiac dysfunction sufficient to explain the presence and extent of PH?
The estimation of PAP by echocardiography in patients with valve disease follows the usual principles as outlined in current guidelines (4): the probability of PH (i.e., mean PAP ≥ 25 mmHg) is low if peak TRV is ≤2.8 m/s and there are no indirect echocardiographic signs of PH (such as RV dilatation and/or dysfunction, D-shape of the left ventricle, shortened pulmonary acceleration time). The probability of PH is intermediate if peak TRV is ≤2.8 m/s but there are indirect signs of PH or if peak TRV is 2.9–3.4 m/s but without indirect signs of PH. The probability of PH is high if peak TRV is 2.9–3.4 m/s with indirect signs of PH or if peak TRV is ≥3.4 m/s regardless of indirect signs of PH. To be correct the central venous pressure as estimated from diameter and respiratory variability of the inferior vena cava has to be added to the transtricuspid pressure difference (as calculated from peak TRV) to calculate systolic PAP. However, this has not consistently been done in clinical studies, and even the current PH guidelines do not make absolutely clear how we should deal with this issue. An assessment of the RV and the tricuspid valve must be performed at the same time as RV function is an important prognostic predictor in various settings including left-sided valve disease (40).
If there is non-invasive evidence of PH, the underlying mechanism has to be assessed by multimodal imaging with echocardiography again being the key tool. The key question always is whether there is post-capillary or pre-capillary PH. The first step to address this is to assess the severity of the stenosis or regurgitation of the aortic and/or mitral valve. According to the current understanding of the grading of the severity of valve disease, only lesions fulfilling criteria for severe valve stenosis or regurgitation are hemodynamically significant in that they can cause LV dysfunction, LAP elevation and subsequently post-capillary PH. A description of the grading of AS/AR/MS/MR is beyond the scope of this review but can be found elsewhere(41). The next step is the assessment of LV systolic and diastolic function and semi-quantitative estimation of LVEDP and LAP (in relation to right atrial pressure) by echocardiography. If the severity of valve disease and LV dysfunction are likely to explain the presence and extent of PH, and the entire picture fits to a post-capillary form of PH, RHC can be deferred, treatment can be initiated, and a follow-up echocardiogram will help to understand whether the working hypothesis was appropriate (1, 36).
There will be situations however, where it remains unclear whether the presence and extent of PH is explained by the severity of valve disease. We will use in the following a diagram to present the various hemodynamic patterns in a simplified manner (Figure 1). The following scenarios have to be considered: a patient may have two diseases, i.e., either valve disease and non-group 2 PH (Figure 2) or valve disease and PH in the context of LV dysfunction which however is not primarily the result of valve disease (Figure 3) although valve disease can contribute to further progression of LV dysfunction. Examples for the latter include severely reduced LVEF due to non-ischemic cardiomyopathy and moderate secondary MR or moderately reduced LVEF after myocardial infarction and moderate AS. Echocardiography can help to distinguish between post-capillary (group 2 PH) and pre-capillary (non-group 2) forms of PH although this is not always reliable. A small or normal-sized left ventricle without hypertrophy, a high LV eccentricity index (i.e., a D-shaped LV), a larger right atrium than LA, and enlarged and apex-forming RV, a low peak early transmitral velocity to peak early mitral annular velocity (mitral E/e’), and a short pulmonary acceleration time are markers of pre-capillary rather than post-capillary PH (1).
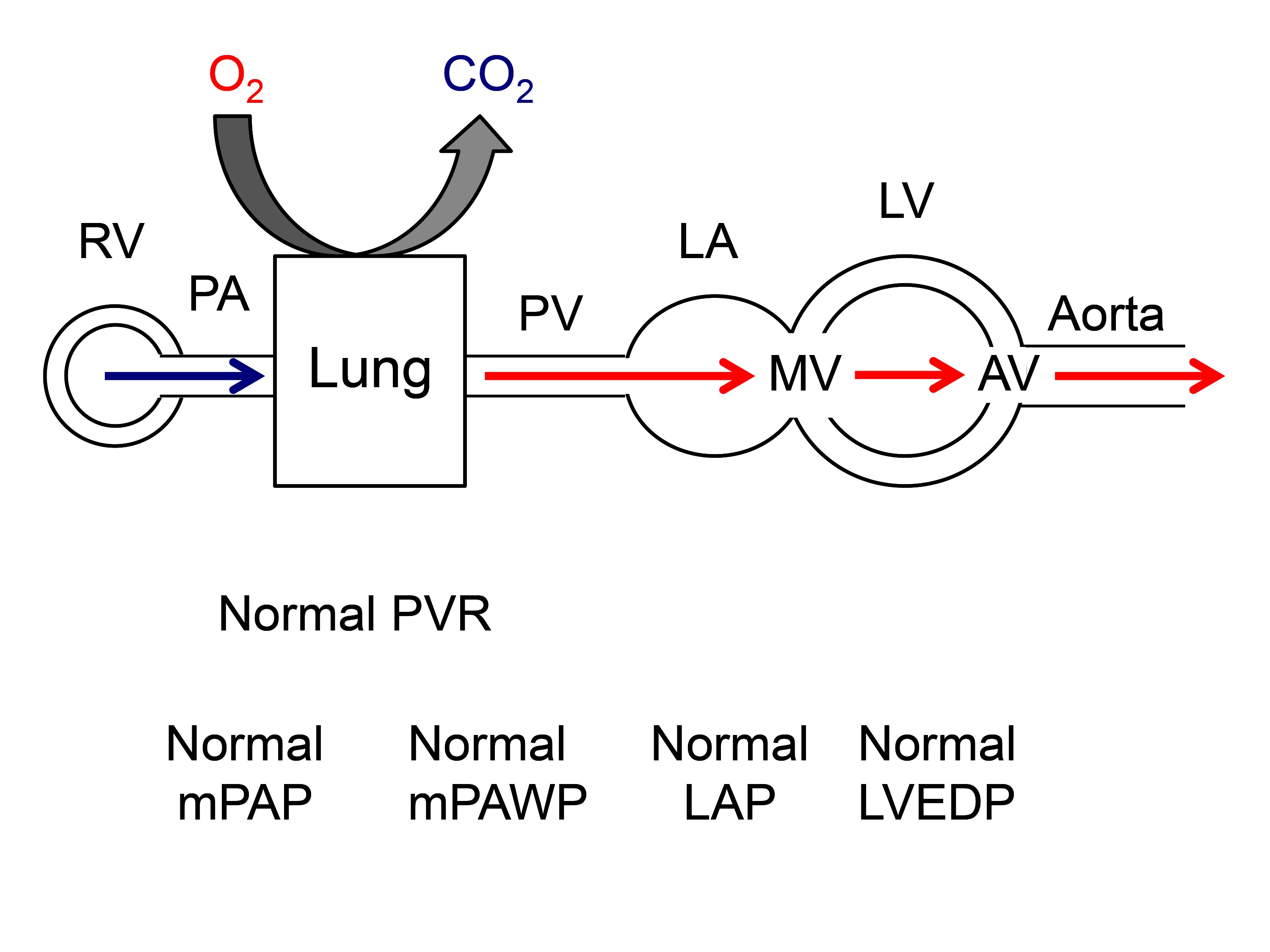
Figure 1. Normal hemodynamic situation of the circulation from the right heart across the lung and the left heart. AV: aortic valve, CO2: carbon dioxide, LA: left atrium, LAP: left atrial pressure, LV: left ventricle, LVEDP: left ventricular enddiastolic pressure, mPAP: mean pulmonary artery pressure, mPAWP: mean pulmonary artery wedge pressure, MV: mitral valve, PA: pulmonary artery, PV: pulmonary veins, PVR: pulmonary vascular resistance, O2: oxygen, RV: right ventricle.
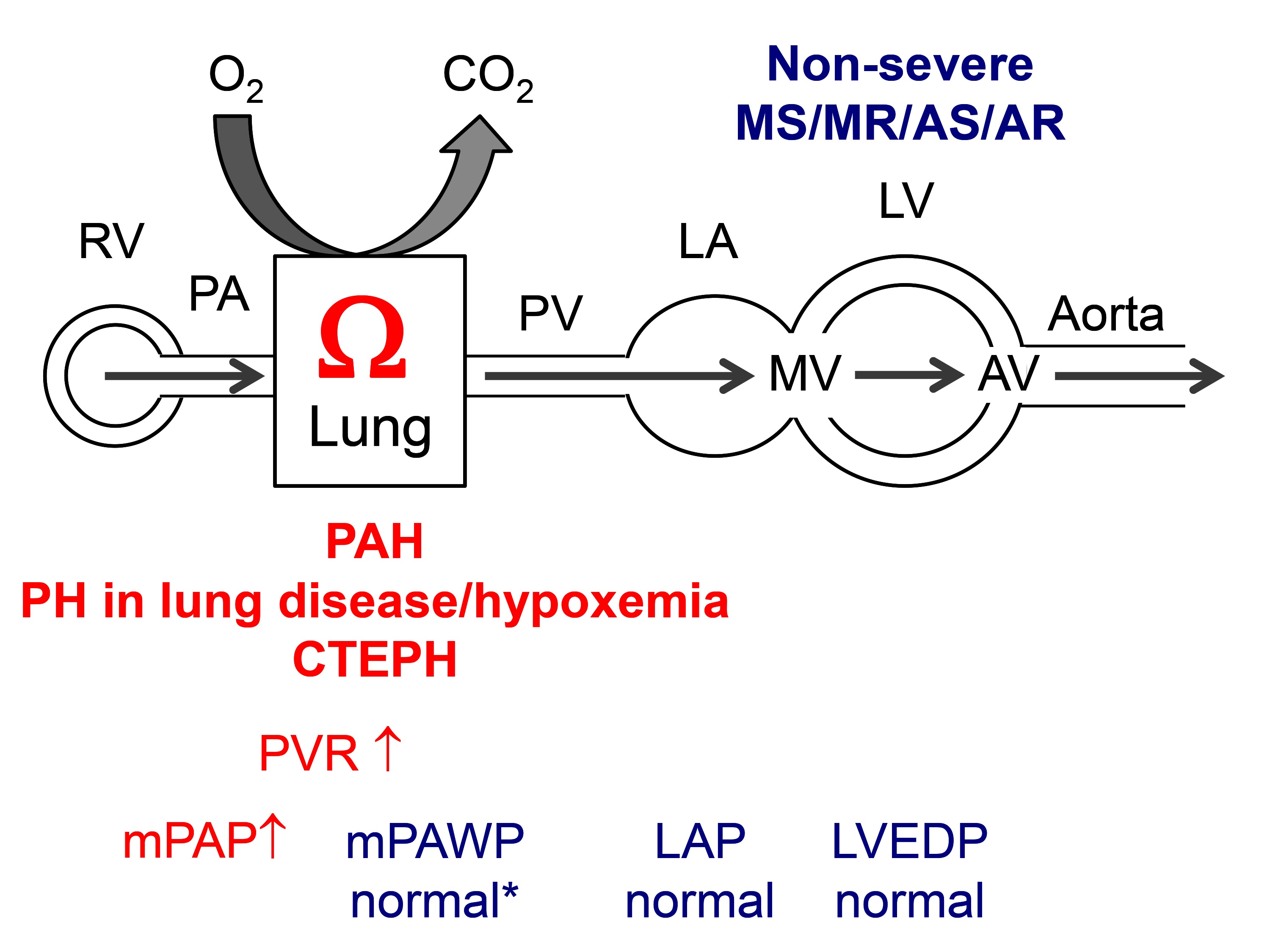
Figure 2. Hemodynamics of pulmonary hypertension (PH) other than group 2 PH in a patient with non-severe mitral stenosis (MS), mitral regurgitation (MR), aortic stenosis (AS), or aortic regurgitation (AR). PAH: pulmonary arterial hypertension, CTEPH: chronic thromboembolic PH. * typically relatively low. Other abbreviations as in Figure 1.
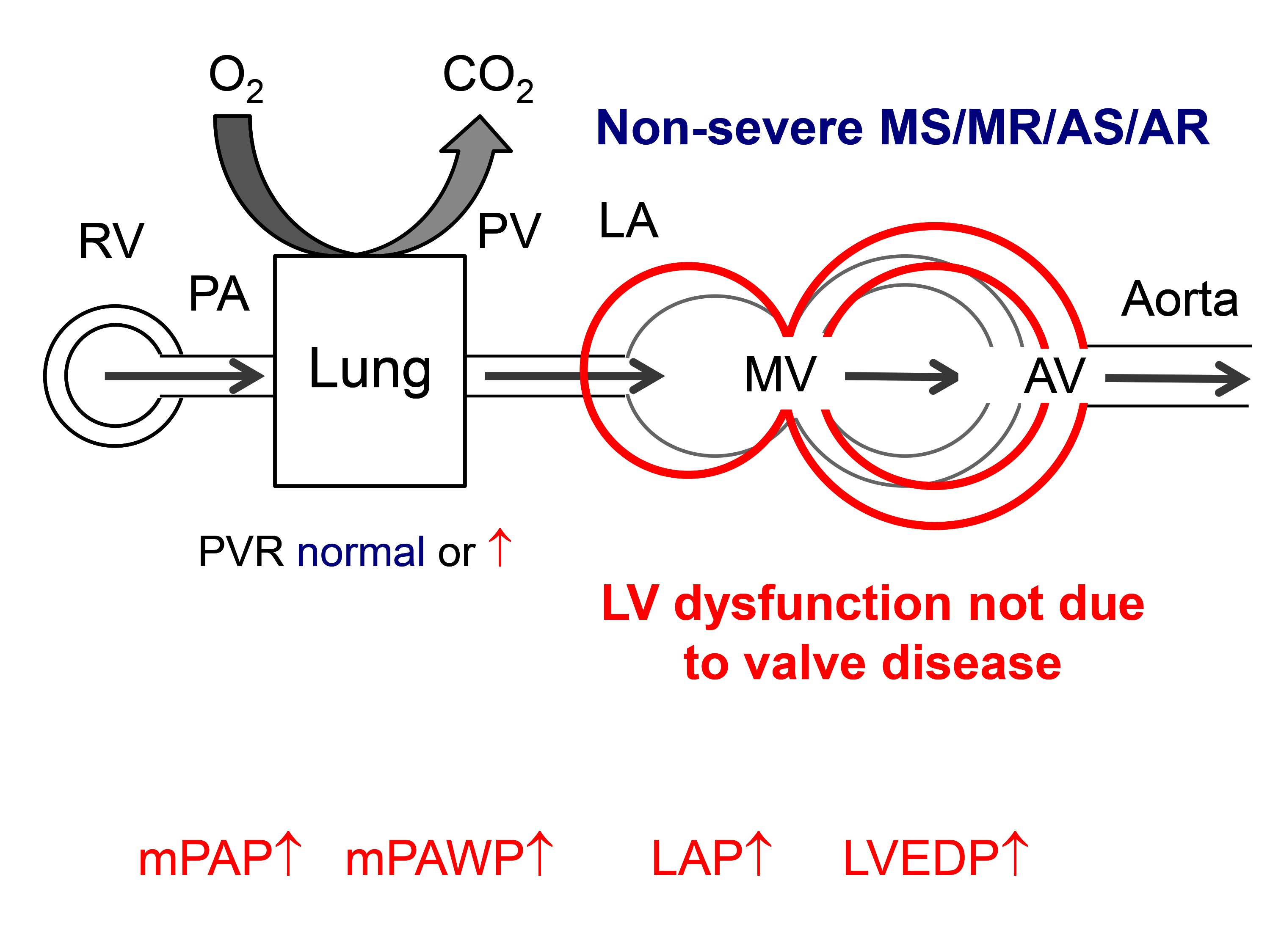
Figure 3. Hemodynamics of group 2 pulmonary hypertension due to non-valve disease related left ventricular (LV) dysfunction in a patient with non-severe mitral stenosis (MS), mitral regurgitation (MR), aortic stenosis (AS), or aortic regurgitation (AR). Other abbreviations as in Figure 1.
In Table 3, there is a summary of clinical features which should raise the suspicion of the presence of non-group 2 PH or group 2 PH which is not the result of valve disease, which should trigger a more extensive work-up.. In these situations it will often be important to perform RHC to clarify the situation. Left heart catheterization with measurement of LVEDP will sometimes be helpful or even compulsory to unequivocally define the hemodynamic pattern and to exclude rare pathologies such as veno-occlusive disease. By definition (4) if there is PH (mPAP ≥25 mmHg), mPAWP must be ≥15 mmHg, and LVEDP must be similar, if PH is the result of MR, AR or AS. If PH is the consequence significant MS, mPAWP ≥15 mmHg and a significant diastolic PAWP-LV pressure gradient must be present. If mPAP is ≥25 mmHg but mPAWP is <15 mmHg, there is a non-group 2 PH. The presence of non-group 2 PH is relatively rare in patients with severe valve disease but its recognition is of paramount importance since in such a patient a mitral or aortic valve intervention will not lower pulmonary pressures. Having said that it is also well known that in some patients with longstanding CpcPH RHC may reveal pure pre-capillary PH after aggressive reduction of filling pressures by diuretics or and/or after valve replacement, and that only a volume challenge may reveal the true hemodynamic picture (42). In patients with severe valve disease and LV dysfunction likely to explain the presence of PH but non-invasive evidence of disproportionally high PAP, RHC will be important to assess whether there is IpcPH or CpcPH as this has prognostic impact (18). The current valve disease guidelines are relatively reluctant with regards to RHC during the work-up of a patient with valve disease potentially undergoing valve surgery/valve intervention (41). However, given the previous considerations we think that in patients evaluated/planned for valve surgery/intervention RHC should be performed at the time of the coronary angiogram. In Figure 4, an algorithm for the use of RHC in the assessment of a patient with valve disease and possible PH is shown.
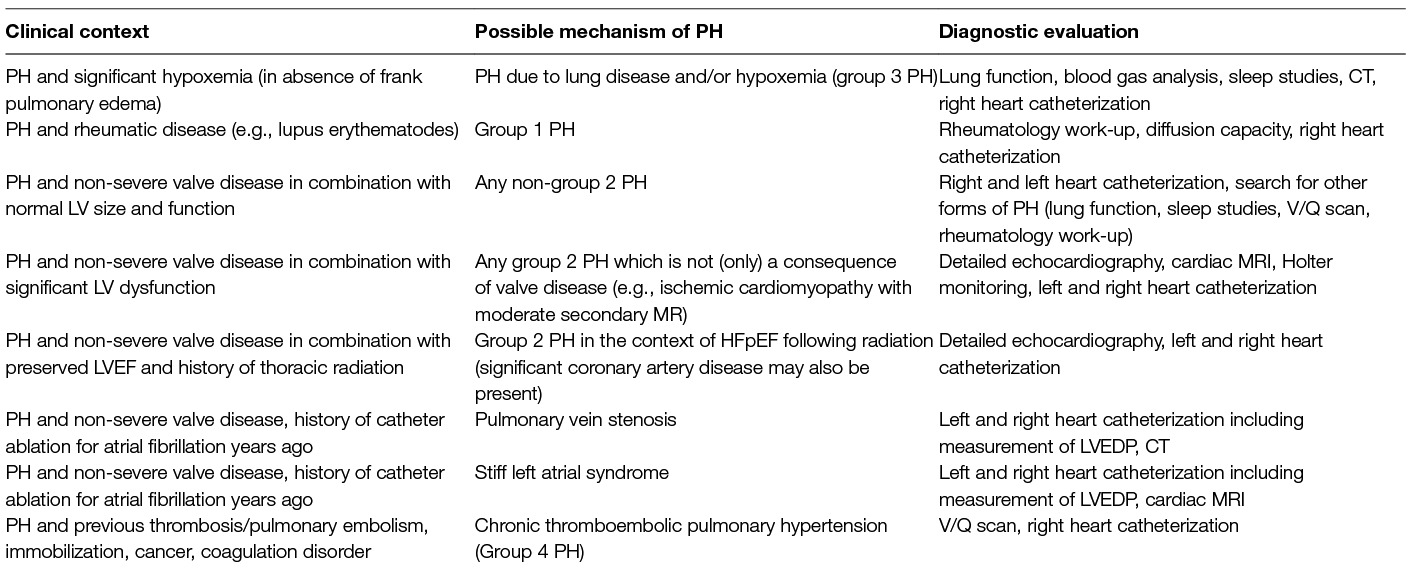
Table 3. Clinical features in patients with valve disease and pulmonary hypertension (PH) suggesting the possibility of the presence of PH with a mechanism unrelated to valve disease; these considerations are particularly relevant if valve disease does not fulfil criteria for severe stenosis/regurgitation.
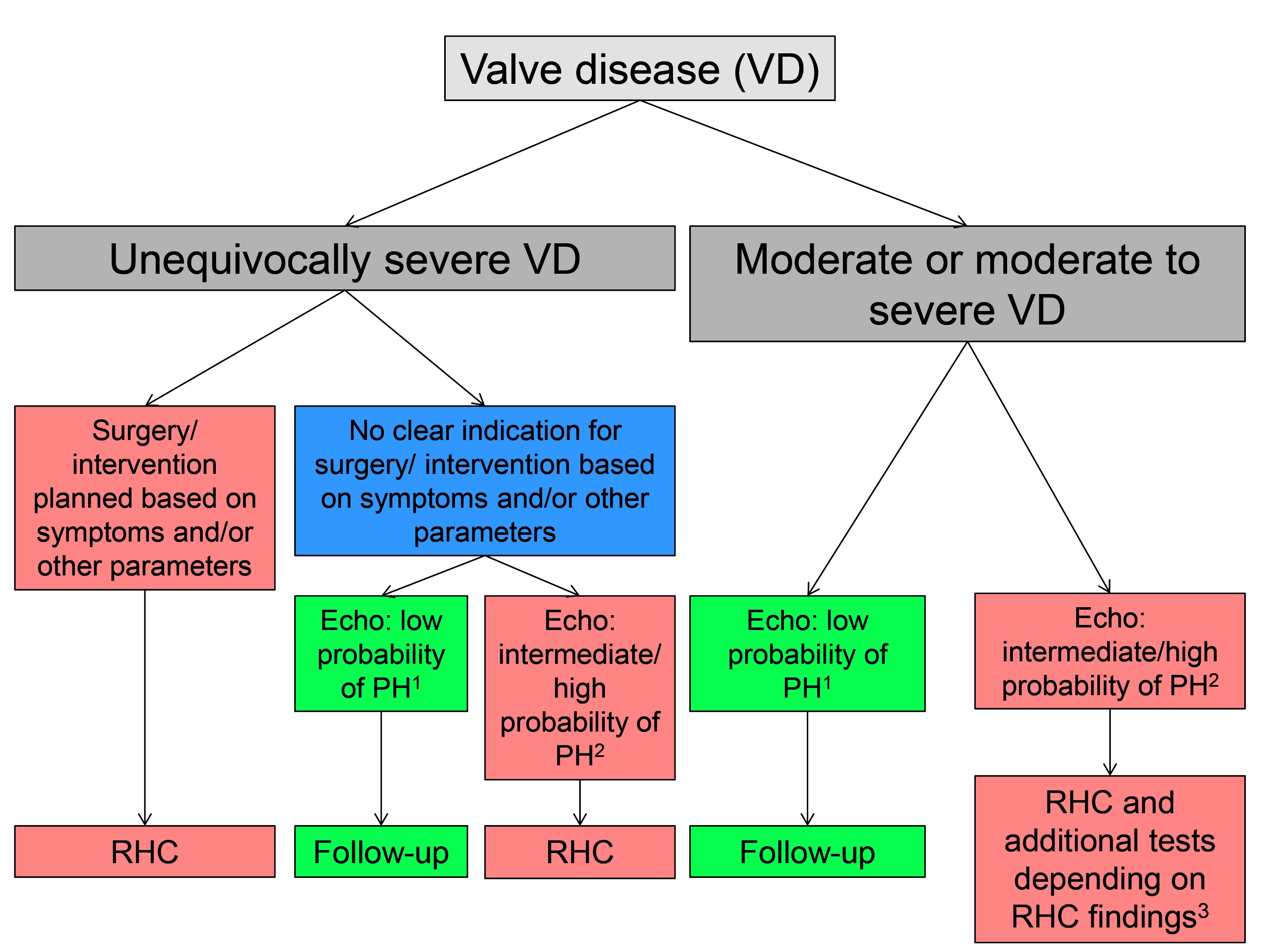
Figure 4. Suggested algorithm to detect pulmonary hypertension (PH) using echocardiography (echo) and right heart catheterization (RHC) in patients with left-sided valve disease (VD, i.e., mitral stenosis and/or regurgitation, aortic stenosis and/or regurgitation). 1low probability of PH: peak TRV ≤2.8 m/s and no indirect echocardiographic signs of PH 2intermediate probability of PH: peak TRV ≤2.8 m/s but indirect signs of PH or if peak TRV but without indirect signs of PH, high probability of PH: peak TRV 2.9–3.4 m/s with indirect signs of PH or peak TRV ≥3.4 m/s regardless of indirect signs of PH 3please see Figure 3.
Although it is appealing to study PAP on exercise to discover the clinical relevance of valve disease in ambiguous situations (3, 43), the role of exercise PH is not well defined at the moment. Stress echocardiography studies have shown that exercise PH (typically defined as systolic PAP > 60 mmHg) is associated with the future occurrence of symptoms in asymptomatic patients with at least moderate degenerative MR (44), cardiac events in patients with secondary MR (45), and cardiac events in asymptomatic patients with severe AS (46). However, exercise PAP depends on pulmonary blood flow, and an absolute exercise s PAP value has to be interpreted in the context of exercise capacity and pulmonary blood flow respectively (3). In addition, exercise sPAP has been shown to be strongly related to resting sPAP (44–46), and therefore the additional information of exercise PH is somewhat limited. Furthermore, stress echocardiography cannot reveal the exact mechanism underlying the rise in sPAP during exercise (rise in LAP versus rise in pulmonary vascular resistance). Recently, it has become clear that PH is common also in HFpEF in absence of significant valve disease (37, 47) and there may be a spectrum of hemodynamic rest/exercise profiles ranging from an isolated rise in PAWP during exercise to a CpcPH pattern with a rise in both PAWP and PVR during exercise (48). A similar diversity is likely present in patients with valve disease but data on invasive exercise hemodynamics in patients with valve disease are lacking. Thus, guidelines (41) currently do not provide recommendations for interventions based on exercise PH.
In patients with MS, the LV is not affected by the valvular problem although in rheumatic heart disease LV dysfunction can occur independently of valve disease. The obstruction at the level of the mitral valve leads to increased LAP which is directly backwards transmitted to the pulmonary veins (Figure 5) (3). The transmitral gradient is a strong but not the only determinant of PAP (49). Lower net atrioventricular compliance, a composite measure of LA and LV compliance, has been shown to be a predictor of sPAP independent of mitral valve area and mean diastolic pressure gradient (49). Notably, net atrioventricular compliance and mitral valve area have also been identified as independent predictors of valve intervention or death in patients with MS (49). The LA in severe MS is often significantly enlarged, and LA function is impaired due to fibrosis. This in turn can lead to atrial fibrillation which can further aggravate LA dilation and dysfunction.
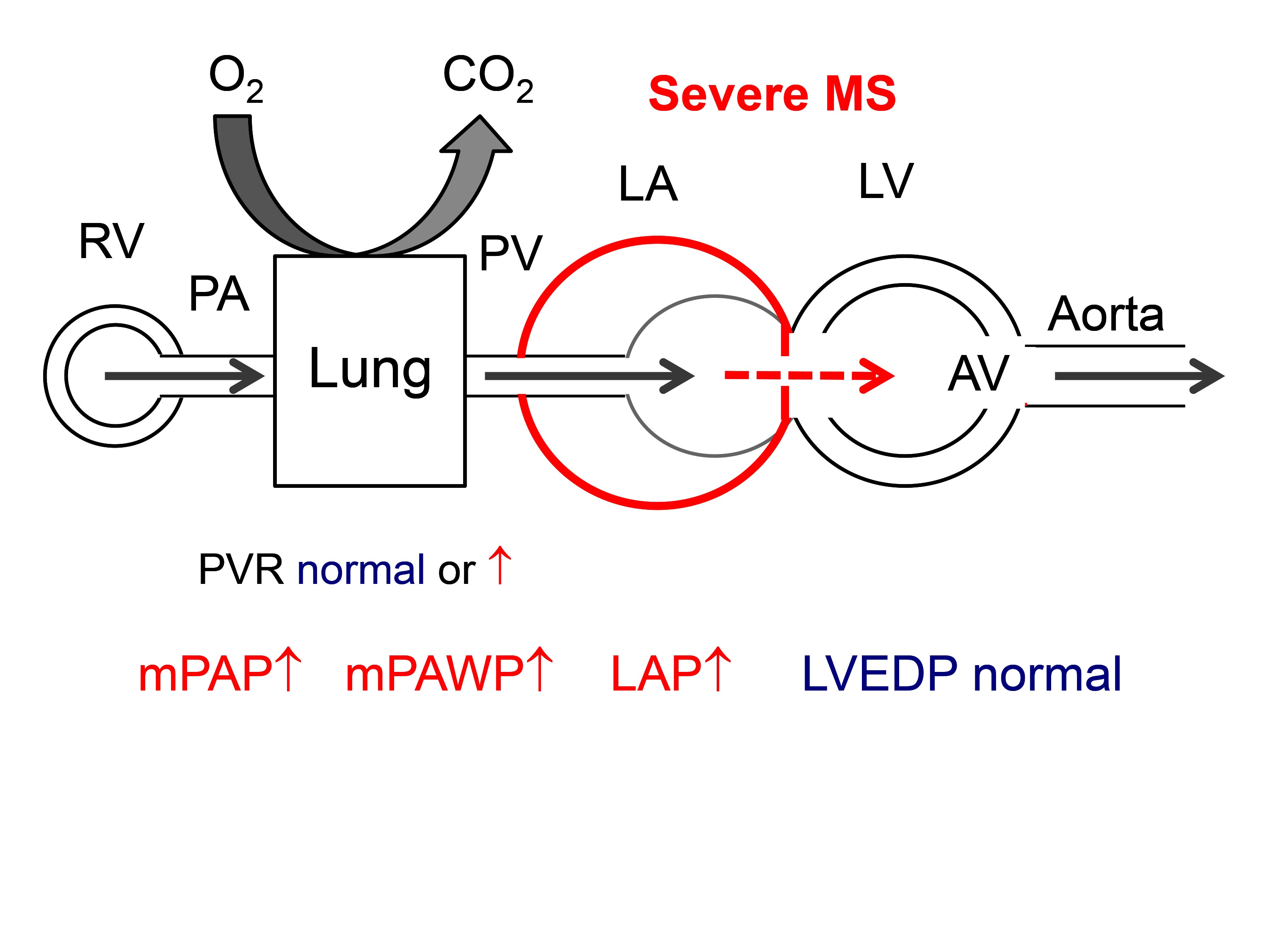
Figure 5. Hemodynamics of severe mitral stenosis (MS). It should be noted that the LV is not affected by the valvular problem, and LVEDP is normal. A significant diastolic gradient between LVEDP and PAWP is characteristic. Abbreviations as in Figure 1.
Chronic LAP elevation can lead to pulmonary vascular remodeling and additional pre-capillary PH, and patients with long-standing severe MS often have substantial CpcPH. In a large study using RHC (n = 599), 38% of patients with severe MS undergoing percutaneous mitral commissurotomy had sPAP ≥50 mmHg. Many of these patients had CpcPH [mean PVR 329 dyn*sec*cm−5 (4.1 WU) and 857 dyn*sec*cm−5 (10.7 WU) in patients with sPAP 50–79 and ≥80 mmHg respectively] (6). This increase in RV afterload can lead to RV dilatation and dysfunction with secondary tricuspid regurgitation which can be further aggravated by structural alterations of the tricuspid valve in rheumatic heart disease. Studies have shown that significant pre-intervention PH is a predictor of poor long-term prognosis in patients with severe MS undergoing valve replacement or percutaneous mitral commissurotomy (5, 8). Isolated post-capillary PH usually resolves quickly after successful mitral valve intervention, whereas in patients with CpcPH, PH can persist despite normalization of LAP and PAWP, and paradoxically hemodynamics in such patients may reveal pure pre-capillary PH years after mitral valve intervention. Thus, incomplete resolution of PH with persistence of pre-capillary PH and RV dysfunction in patients with long-standing PH are the most likely mechanism underlying the prognostic value of PH in MS although one study has shown normalization of PH in all patients with PH even in those with baseline systolic PAP > 80 mmHg (6). The current ESC guidelines acknowledge the role of PH as a marker of more advanced disease and give a IIa recommendation for percutaneous mitral commissurotomy in patients with significant MS (valve area <1.5 cm2), no/little symptoms but a systolic PAP > 50 mmHg (41).
The LV volume overload in chronic severe degenerative MR leads to progressive LV dilatation and eccentric hypertrophy and eventually systolic and diastolic dysfunction. This together with the direct effect of the systolic backflow into the LA under LV pressure can lead to LAP elevation with large V waves and PAWP elevation (Figure 6). The LV in severe primary MS is that of a special form of heart failure with preserved, midrange, or reduced LVEF. The ventricle is dilated, and as soon as LVEF is <60% there is systolic dysfunction which however is masked by the high preload (50). Any LVEF less than 60% in patients with degenerative MR is associated with reduced survival under medical therapy (51). Systolic LV dysfunction in MR is accompanied by increased LV stiffness, i.e., diastolic dysfunction. Left atrial enlargement is the result of LV dysfunction and volume overload and favors the occurrence of atrial fibrillation (52). Larger LA size in severe MR is associated with higher PAP and worse outcome (53). Independent predictors of higher sPAP in three studies included higher age (11), female sex (10), larger LA size (10–12), larger LV end-systolic dimensions (10), higher medial E/e’ (12), shorter mitral deceleration time (12) chronic lung disease (10), dialysis (10), previous myocardial infarction (10), and higher body mass index (10). In all large contemporary series of patients with MR with the majority undergoing surgery, baseline sPAP as assessed by echocardiography (3 studies) or RHC or echocardiography (one study) was a strong predictor of mortality (9–12).
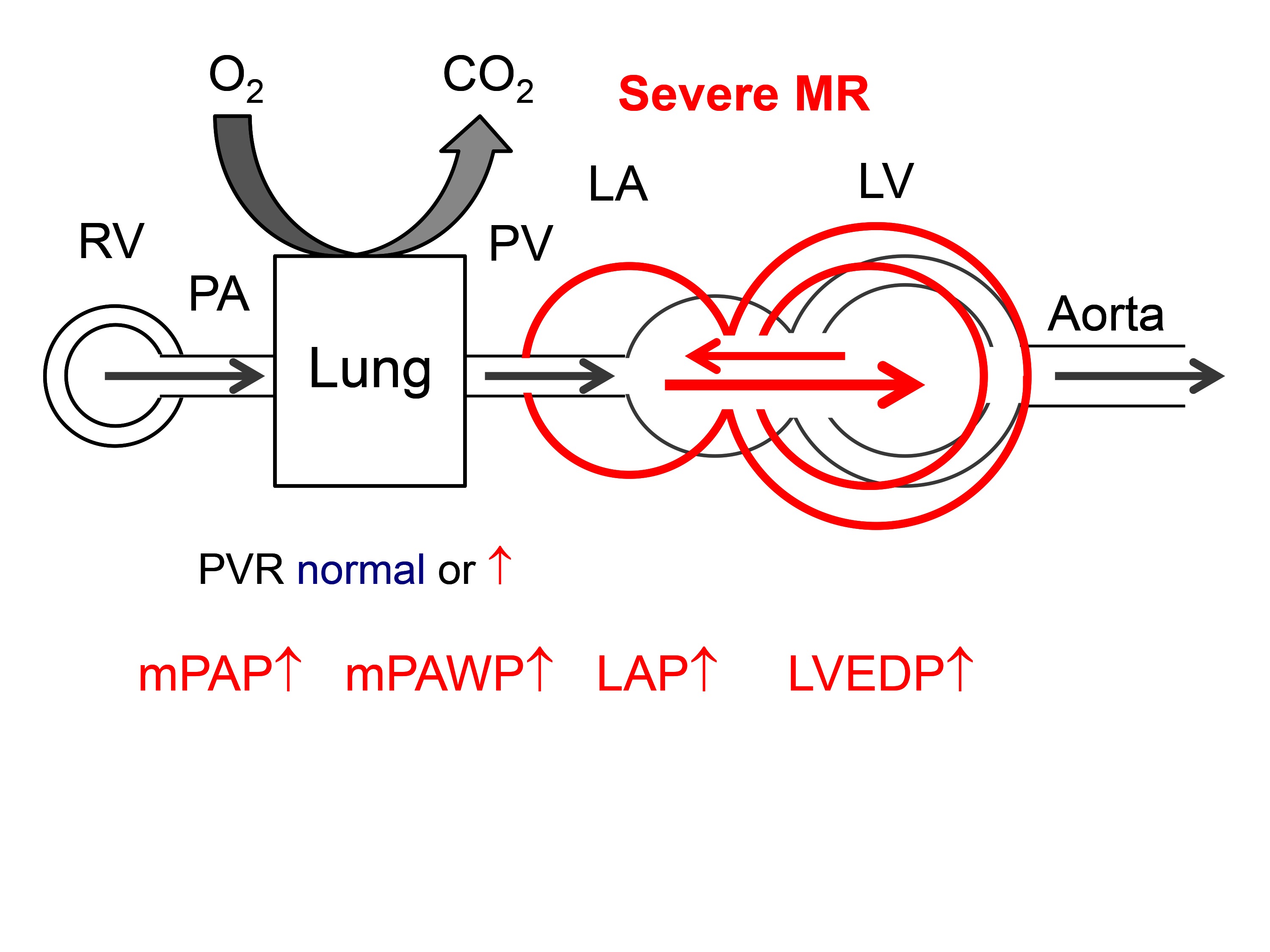
Figure 6. Hemodynamics of severe primary mitral regurgitation (MR). There is volume overload and dilatation of the both LV and LA. Abbreviations as in Figure 1.
Notably, despite successful mitral valve surgery, PH may persist. In a series of 1318 patients with degenerative MR with 86% undergoing mitral valve surgery, postoperative sPAP >35 mmHg was observed in 19% of patients and was predicted by older age and higher preoperative sPAP (10). In another large series (n = 873) of patients undergoing surgery for MR the sPAP in the entire population decreased from 43 mmHg before surgery to 39 mmHg early after surgery and remained unchanged after two years (9).
Both the 2017 ESC guidelines (41) and the 2017 update of the US guidelines (54) give a class IIa indication for surgery for asymptomatic patients with LVEF >60%, and LVESD <45 mm (i.e., no indication for surgery based on LV remodeling) but the presence of PH defined as sPAP >50 mmHg. Guidelines explicitly mentioned that an sPAP >50 mmHg should be confirmed by RHC if this represents the sole criterion for surgery (41).
In contrast to primary MR the mitral valve in secondary (or functional) MR is initially structurally normal, and LV dysfunction is initially the result of a process unrelated to the mitral valve (e.g., myocardial infarction with LV remodeling) which then leads to MR. Thus, PAWP elevation and post-capillary PH in patients with secondary MR may be result of LV dysfunction per se, MR, and the secondary effects of MR on the ventricle (MR begets MR). In patients with LV dysfunction (LVEF <50%), the severity of secondary MR was identified as an independent predictor of higher sPAP (55). However, a more recent study showed similar mPAP and mPAWP in patients with advanced HFrEF (median LVEF 27%) with no/mild, moderate, or severe secondary MR (56) clearly indicating that MR in this setting is not the only driver of PH. On the other hand, the presence of PH (defined as sPAP ≥45 mmHg by echocardiography) has been shown to be a predictor of death in patients with LVEF ≤40%, but this association between PH and mortality was independent of LVEF, LV diastolic function, and functional MR (57) suggesting a complex pathophysiology of PH in this setting. Although detailed RHC data from a larger population of patients with secondary MR is not available, it is likely that many HFrEF patients with moderate or severe secondary MR and PH have CpcPH rather than simply IpcPH, and that the presence of a pre-capillary component of PH is the mediator of a poor prognosis and the incomplete response or absence of response to a mechanical intervention for MR. This assumption is supported by an important study by Dupont et al. (58) who demonstrated that in patients with HF [n = 724, mainly HFrEF (LVEF 19–9%)], low (inframedian) pulmonary capacitance (i.e., a parameter reflecting both high PAWP and high PVR) was associated with poor outcomes. Among the patients with low pulmonary capacitance (n = 362, mPAP = 37 ± 9 mmHg, mPAWP = 25 ± 7 mmHg), the prevalence of MR ≥3 + was 43% indicating that there were many patients with secondary MR and CpcPH (58).
A variety of cardiac diseases can be associated with secondary MR. The pathophysiology is therefore variable and can include only moderately dilated LV’s with distorted geometry after an infarct in the territory of right or circumflex artery with tethering of one leaflet and eccentric MR or severely dilated LVs in the context of non-ischemic cardiomyopathy with severe annulus dilatation and tethering of the valve leaflets. As a consequence the mitral valve is not the primary target for therapy in patients with secondary MR and PH. The general approach in these patients is to treat the underlying cardiac disease in an optimal manner.Surgery or interventions for the correction of MR remain an option only for patients remaining symptomatic despite optimal medical and device therapy (41). Percutaneous mitral valve repair in secondary MR has been show to lead to an acute reduction in LAP, mPAWP, and mPAP. However, the baseline mPAP in that study was only mildly elevated (mPAP 29 mmHg), and the reduction of mPAP was relatively modest (- 3 mmHg) (59). In patients with more severe PH (sPAP >50 mmHg) in the context of secondary MR, percutaneous mitral valve repair has been shown to lead to a reduction in sPAP, but sPAP remained higher than in patients without baseline PH, and patients with pre-existing PH had a nearly four-fold higher mortality than patients without (60). In the German Transcatheter Mitral Valve Intervention registry (with two thirds of patients having secondary MR), percutaneous mitral valve repair was associated with a reduction in sPAP from pre-intervention to hospital discharge in patients with sPAP 37–50 mmHg (from 44 to 40 mmHg) and those with sPAP >50 mmHg (from 60 to 51 mmHg) (61). However, there was obviously persisting PH in many patients, and mortality in these two PH groups after percutaneous mitral valve repair was still higher than in those without PH (sPAP ≤36 mmHg) (61). Registry data suggest that there is also some reverse LV and LA remodeling after percutaneous mitral valve repair in patients with secondary MR (62). However, the impact of this phenomenon on PH is unknown.
Given the various determinants of PH in patients with secondary MR and lack of data from controlled studies on the prognostic impact of mitral valve interventions in these patients, current guidelines (41) do not give recommendation regarding valve interventions based on the presence of PH in these patients.
In severe AS, pressure overload leads to compensatory concentric LV hypertrophy. According to the Laplace equation (LV wall stress ~LV pressure * LV radius/LV wall thickness) an increase in wall thickness in presence of increased LV pressure helps to normalize wall stress. By this mechanism, many patients with severe AS can preserve their stroke volume, i.e., they have a stroke volume index >35 ml/m2 and a mean transvalvular gradient >40 mmHg, i.e., high gradient severe AS. However, the process of the development of LV hypertrophy is maladaptive as it is associated with myocardial fibrosis and LV diastolic dysfunction with an increase in LVEDP to achieve a normal LV end-diastolic volume and finally an increase in LAP to ensure LV filling (Figure 7) (63). Thus, in AS with preserved LVEF which represents the vast majority of patients (Table 2), we are faced with a phenotype of HF which is very similar to that seen in patients with HFpEF in whom longstanding hypertension leads to concentric LV remodeling/hypertrophy, diastolic and systolic dysfunction as well as LA dysfunction (64, 65) resulting in a rise in PAWP and PAP already at rest (66) or on exercise (67). Similarly to HFpEF, patients with severe AS can have a spectrum of abnormalities in LV systolic function despite LVEF >50%, and in subset of patients with severe AS and LVEF >50%, stroke volume index is less than 35 ml/m2 due to impaired filling and contractility, an entity referred to as paradoxical low flow-low gradient severe AS (68).
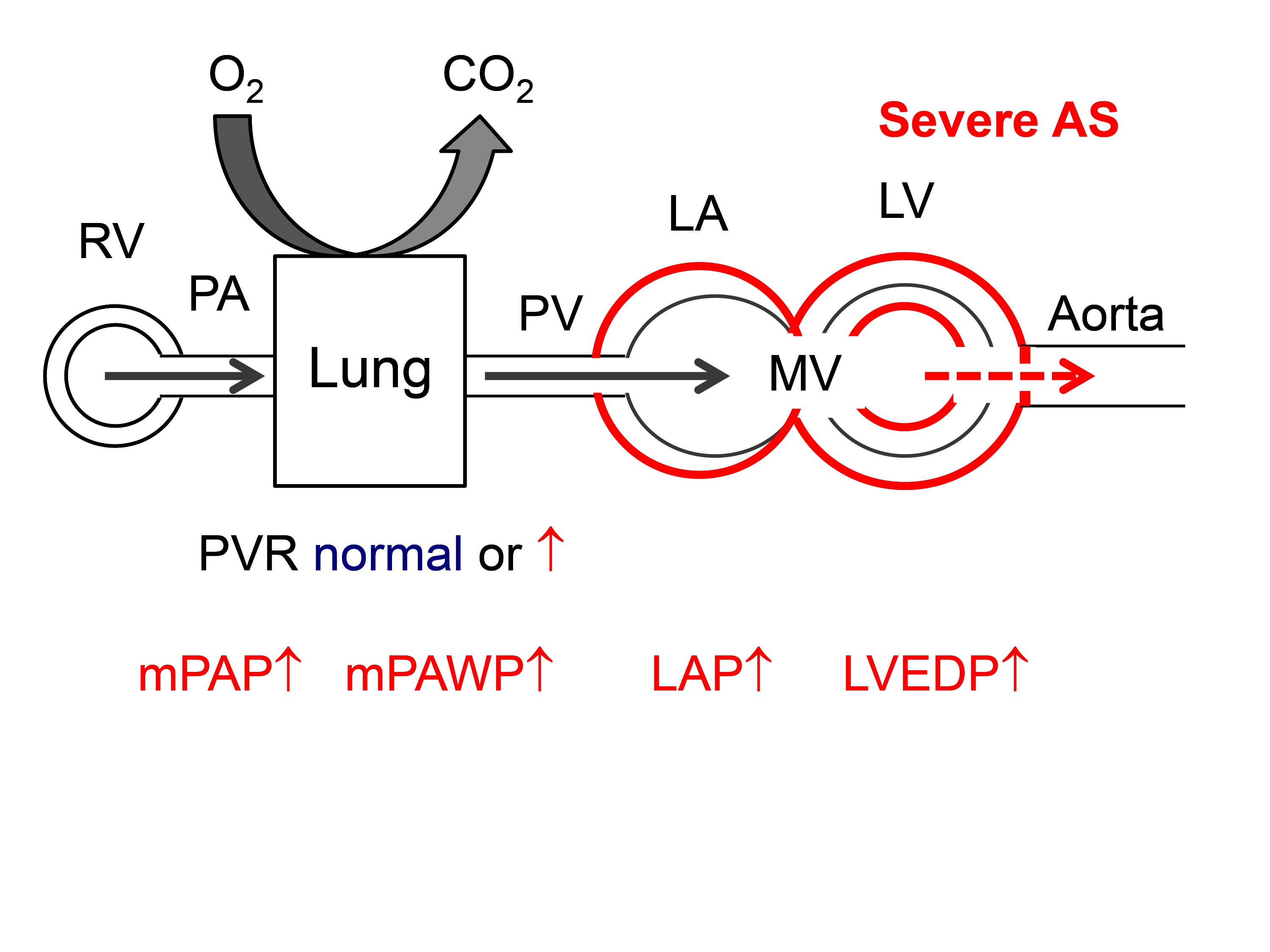
Figure 7. Hemodynamics of severe aortic stenosis (AS). There is pressure overload of the LV with concentric hypertrophy. The LA is secondarily affected by diastolic and systolic LV dysfunction. Abbreviations as in Figure 1.
As shown in Table 2, PH is common in patients with severe AS. In general there is an association between higher sPAP and more severe AS as expressed by lower aortic valve area (AVA) (14, 28) and lower LVEF (14, 28, 35). However, PH is common also in patients with normal or only mildly reduced LVEF, where LV diastolic dysfunction (17), LA dilatation (23, 28, 35) and dysfunction (69), atrial fibrillation (14), concomitant MR (14, 23) and comorbidities including lung disease (17), obesity (27), anemia (27), and renal failure (27) are key determinants of PH. The majority of studies used echocardiography to assess the presence of PH, and thus the exact hemodynamics c remain unknown. In an interesting RHC study, O’Sullivan et al. (18) found that PH (invasive mPAP ≥25 mmHg) was present in 75% of elderly patients undergoing TAVR, 17% of whom had pre-capillary PH and 83% had post-capillary PH (LVEDP >15 mmHg versus ≤15 mmHg was used for the definition since PAWP was not measured systematically). In the post-capillary PH group, 82% had IpcPH and 18% had CpcPH. Patients with CpCPH had the smallest AVA, the lowest LVEF and the most severe MR.
As shown in Table 2, the vast majority of studies among patients with severe AS undergoing surgical aortic valve replacement (AVR, SAVR) or transcatheter AVR (TAVR) concur that the presence of pre-AVR PH is a predictor of death. A meta-analysis summarizing the data from 16 TAVR studies showed an increased 30 day, 1 year, and 2 year mortality in patients with PH before TAVR (70). The analysis by O’Sullivan et al. (18) revealed that pre-capillary and CpcPH but not IpcPH PH were associated with increased 1 year mortality.
Studies concur that SAVR and TAVR reduced PAP in many but not all patients (18, 20, 28, 29, 31), and that the reduction in PAP is overall relatively modest. In the study by O’Sullivan (18), a reduction in sPAP (measured by echocardiography pre- and post-TAVR) following TAVR was observed in patients with IpcPH (50 to 45 mmHg) and CpcPH (58 to 50 mmHg) PH but not in those with pre-capillary PH (49 to 52 mmHg). The latter is not surprising, and the former is not unexpected either, because PH is the result of the maladaptive changes of the LV and LA in response to pressure overload and only in part due to AS per se, and removal of the outflow tract obstruction will not cure the LV disease immediately. A further reduction in PAP over time due regression of LV hypertrophy, LV dysfunction and LA dysfunction following relief of pressure overload may be expected. However, in one study sPAP remained unchanged from one week to one year after TAVR (27), and the same has been shown for patients after SVAR. Similarly, Sinning at al. (26) found a significant but limited reduction in sPAP three months after TVR in patients with baseline sPAP 30–60 mmHg (from 39 to 34 mmHg) and those with baseline sPAP ≥60 mmHg (from 66 to 50 mmHg). The extent of PAP reduction after SAVR/TAVR is clinically important since several studies have shown that persistent PH after TAVR determines prognosis, and that the impact of post-TAVR sPAP is even more important than that of pre-TAVR systolic PAP (14, 28). In the study by Masri et al. (28), 67% of a cohort of 407 patients with severe AS undergoing TAVR had PH at baseline (mPAP ≥25 mmHg on RHC), and 25% of the entire cohort had post-TAVR sPAP >45 mmHg on echocardiography, and these patients had a two-fold higher 2 year mortality than patients without baseline PH and those with baseline PH but post-TAVR sPAP <45 mmHg. Baseline determinants of post-TAVR sPAP >45 mmHg included at least moderate MR, atrial fibrillation/flutter, more advanced LV diastolic dysfunction, and larger LA volume index.
Some studies have shown an early improvement of LV relaxation (71, 72) and LA reservoir and conduit function (72) after TAVR, and at least one study has revealed an improvement in peak atrial longitudinal strain and a reduction in LA volumes three months after TAVR (73). However, data on the effect of TAVR on LV relaxation (mediating the early and active phase of mitral inflow; e’) are controversial (72, 73), and even more importantly the process of recovery of LV stiffness (mediating the late and passive phase of mitral inflow) following AVR is very slow and often incomplete [recently summarized by Kampaktsis et a. (63)]. The presence of myocardial fibrosis is the probably key driver of increased LV stiffness and increased LAP and PH, which may explain the persistence of PH in many patients after AVR. Recent research has shown that the presence of any late gadolinium enhancement (marker of fibrosis) in cardiac MRI predicts mortality after AVR (74). Importantly, myocardial fibrosis in patients with AS is not uniform (75), and the pattern of myocardial fibrosis (extracellular volume expansion versus replacement fibrosis) is clinically relevant (76).
The 2017 ESC guidelines give a IIa indication for AVR in asymptomatic patients with severe AS without another indication for surgery but sPAP >60 mmHg (41). The guidelines state that PH should be confirmed by RHC if PH represents to only indication for surgery (41). Notably, this represents a very advanced stage of the disease with significantly worse prognosis than severe AS without PH (19) and low likelihood of complete recovery of LV diastolic and resolution of PH.
Aortic regurgitation imposes combined volume and pressure overload (as indicated by an increased systolic wall stress) (77) to the LV resulting in LV dilatation, eccentric LV hypertrophy, and eventually LV dysfunction. In advanced stages, systolic and diastolic LV dysfunction, LA dysfunction, and secondary MR can lead to increased LAP and post-capillary PH (Figure 8). Markers of this remodeling process (LV end-systolic volume index >25 mm/m2, LVEF <50%) are traditionally used as indications for surgery in asymptomatic patients (41). In contrast to patients with AS, there is little information on the prevalence and prognostic role of PH in patients with AR.
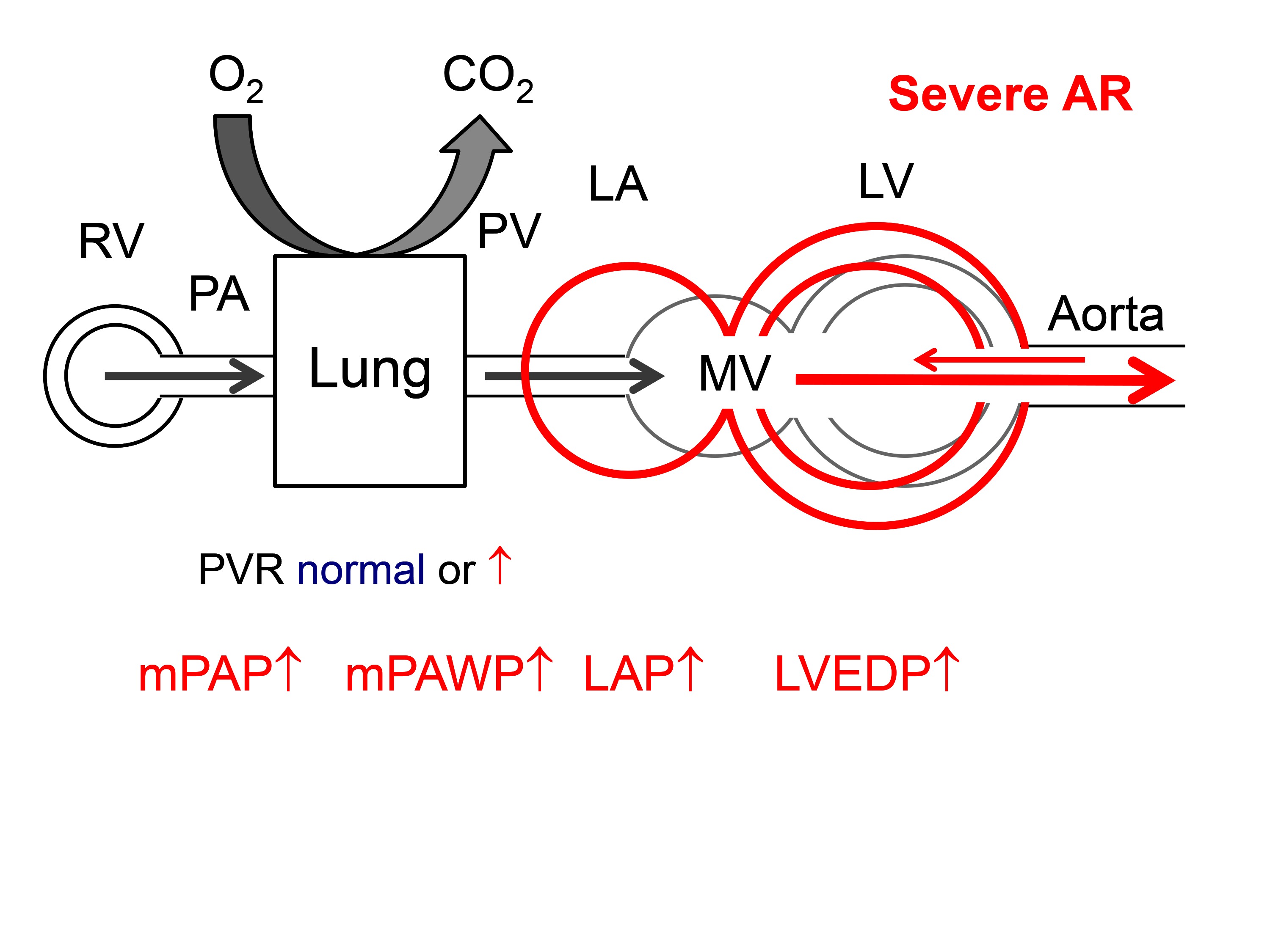
Figure 8. Hemodynamics of severe aortic regurgitation (AS). There is volume overload and dilatation of the LV. The LA is secondarily affected by diastolic and systolic LV dysfunction. Abbreviations as in Figure 1.
In one large contemporary series, 16% of patients with severe AR had sPAP ≥60 mmHg. These patients had larger LV dimensions, lower LVEF, and more severe MR than those with sPAP <60 mmHg (33). Magne et al. (3) reported mild PH (mPAP 26–35 mmHg) in 23%, moderate PH (mPAP 36–45 mmHg) in 9%, and severe PH (mPAP >45 mmHg) in 5% of patients with various degrees of AR (no details published). In current guidelines (41), the presence of PH is not listed as a criterion for valve replacement in AR given the relative paucity of data on the subject.
The combination of several valve lesion is not uncommon the most typical combination being that of AS and MR. The assessment of the severity of AS and MR in this situation is notoriously difficult because MR may lead to a reduction in forward stroke volume and thereby a low flow-low gradient AS situation with all its diagnostic challenges. On the other hand the increased LV afterload due to AS may lead to a reduction of forward stroke volume and an increase in MR respectively. In this context MR is often secondary but primary MR is also possible. Given the detailed discussion above the presence of PH is likely to be common in patients with both relevant AS and relevant MR, and pulmonary pressure may vary depending on filling status, ischemia and dynamic exacerbation of secondary MR, and cardiac rhythm (paroxysmal atrial fibrillation). A detailed discussion of combined valve disease is beyond the scope of the present article. To illustrate the complexity of PH in the context of combined valve disease we just want to mention the study by Toggweiler et al. (78) who have shown that in patients with severe AS undergoing TAVR, concomitant moderate or severe MR at baseline improved in 55% of patients. Predictors of MR improvement included the presence of secondary MR, absence of atrial fibrillation, and absence of PH (defined as systolic PAP > 60 mmHg as assessed by echocardiography or RHC). Thus, PH is clinically highly relevant also in this context although the mechanism underlying this observation is not easy to understand. It may be speculated that RV-LV interactions in presence of significant PH prevent improvements in LV geometry and MR.
The presence of PH is common in valve disease, and most often the mechanism is IpcPH or CpcPH. Thus, PH in valve disease is a marker of HF highlighting that PH is indeed a very important parameter during the assessment and follow-up of patients with valve disease. As discussed above PH is the result of maladaptive changes to the LV, LA, and finally pulmonary vasculature and even the right heart, and these changes may persist fully or in a reduced form after valve intervention resulting in persistent PH with serious prognostic implications. As discussed above the hemodynamic results of valve interventions have mainly been observed by echocardiography. Given the complexity of the hemodynamic pattern and the importance of CpcPH in these patients, systematic RHC early and late after valve interventions may help to better understand their full effects. For instance, we know that aggressive left ventricular unloading by assist device implantation in patients with severe HF and severe CpcPH can reduce not only PAWP but also pulmonary vascular resistance (79).
The replacement or reconstruction of the valve is only one part of the therapy, and a potential residual cardiac dysfunction has to be treated as well. However, the latter aspect of has not been in the focus of research and clinical work in the last years but is only now being recognized. In the patients with a HFrEF phenotype after valve reconstruction or replacement it is relatively evident that standard HFrEF therapies (80) should be established, i.e., angiotensin converting enzyme inhibitors/angiotensin receptor blockers, betablockers, mineralocorticoid receptor blockers, sacubitril/valsartan, ivabradine, and cardiac resynchronization although the effectiveness of these treatments in this context has not explicitly been proven. In patients with a HFpEF phenotype treatment is unknown (80). Given the similarities between HFpEF in the true sense and post-AVR HFpEF spironolactone may be the most attractive drug (81, 82) although this is not proven either. In a substantial number of patients a pre-capillary component of PH may persist after valve replacement although systematic invasive studies in this particular setting are not available. Intense research in the field of PH in the context of HFrEF and HFpEF has revealed that a variety of complex mechanisms are involved in the pathogenesis of CpcPH in these patients, and that specific therapies with proven benefit in group 1 PH may not be efficient in these patients (1). Very recently, the first randomized trial assessing the effect of the 5-phosphodiesterase inhibitor sildenafil on symptoms and cardiac events in patients with persistent PH several months after valve replacement/repair has been published (mPAP ≥30 mmHg required for inclusion; median mean PAP 39 mmHg, median mPAWP 23 mmHg, median pulmonary vascular resistance 3.4 WU) (83). Interestingly, sildenafil therapy was associated with worse clinical outcomes (death, hospital admission, worsening functional class, global symptom burden) than placebo without differences between patient with normal or elevated pulmonary vascular resistance potentially indicating that specific PAH therapies may not be useful for the treatment post-valve replacement IpcPH and CpcPH. This result is very similar to than seen for sildenafil for the treatment of PH (IpcPH and CpcPH) in the context of HFpEF (66).
Given that an exponentially rising number of procedures for valve disease are now being performed also in very sick patients which will improve their symptoms and overall cardiac dysfunction to a certain degree and prevent death due to progressive pump failure, we will be faced with an increasing population of old and sick patients with post-valve replacement/reconstruction heart failure and PH. Thus, intense research in the pathophysiology and the device and medical management of these patients is urgently needed.
MTM searched the literature, wrote the manuscript, and finalized the manuscript based on the input from the co-authors. All the co-authors critically revised the manuscript for important intellectual content.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The great help of Irene Schneider in research projects related to the topic of this review is very much appreciated.
1. Maeder MT, Schoch OD, Kleiner R, Joerg L, Weilenmann D, Swiss Society For Pulmonary Hypertension. Pulmonary hypertension associated with left-sided heart disease. Swiss Med Wkly (2017) 147:w14395. doi: 10.4414/smw.2017.14395
2. Weitsman T, Weisz G, Farkash R, Klutstein M, Butnaru A, Rosenmann D, et al. Pulmonary hypertension with left heart disease: prevalence, temporal shifts in etiologies and outcome. Am J Med (2017) 130(11):1272–9. doi: 10.1016/j.amjmed.2017.05.003
3. Magne J, Pibarot P, Sengupta PP, Donal E, Rosenhek R, Lancellotti P. Pulmonary hypertension in valvular disease: a comprehensive review on pathophysiology to therapy from the HAVEC Group. JACC Cardiovasc Imaging (2015) 8(1):83–99. doi: 10.1016/j.jcmg.2014.12.003
4. Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J (2016) 37(1):67–119. doi: 10.1093/eurheartj/ehv317
5. Fawzy ME, Osman A, Nambiar V, Nowayhed O, El DA, Badr A, et al. Immediate and long-term results of mitral balloon valvuloplasty in patients with severe pulmonary hypertension. J Heart Valve Dis (2008) 17(5):485–91.
6. Fawzy ME, Hassan W, Stefadouros M, Moursi M, El Shaer F, Chaudhary MA. Prevalence and fate of severe pulmonary hypertension in 559 consecutive patients with severe rheumatic mitral stenosis undergoing mitral balloon valvotomy. J Heart Valve Dis (2004) 13(6):942–7.
7. Pourafkari L, Ghaffari S, Ahmadi M, Tajlil A, Aslanabadi N, Nader ND. Pulmonary hypertension in rheumatic mitral stenosis revisited. Herz (2017) 42(8):746–51. doi: 10.1007/s00059-016-4509-2
8. Yang B, Debenedictus C, Watt T, Farley S, Salita A, Hornsby W, et al. The impact of concomitant pulmonary hypertension on early and late outcomes following surgery for mitral stenosis. J Thorac Cardiovasc Surg (2016) 152(2):394–400. doi: 10.1016/j.jtcvs.2016.02.038
9. Ghoreishi M, Evans CF, Defilippi CR, Hobbs G, Young CA, Griffith BP, et al. Pulmonary hypertension adversely affects short- and long-term survival after mitral valve operation for mitral regurgitation: implications for timing of surgery. J Thorac Cardiovasc Surg (2011) 142(6):1439–52. doi: 10.1016/j.jtcvs.2011.08.030
10. Mentias A, Patel K, Patel H, Gillinov AM, Sabik JF, Mihaljevic T, et al. Effect of pulmonary vascular pressures on long-term outcome in patients with primary mitral regurgitation. J Am Coll Cardiol (2016) 67(25):2952–61. doi: 10.1016/j.jacc.2016.03.589
11. Barbieri A, Bursi F, Grigioni F, Tribouilloy C, Avierinos JF, Michelena HI, et al. Prognostic and therapeutic implications of pulmonary hypertension complicating degenerative mitral regurgitation due to flail leaflet: a multicenter long-term international study. Eur Heart J (2011) 32(6):751–9. doi: 10.1093/eurheartj/ehq294
12. Le Tourneau T, Richardson M, Juthier F, Modine T, Fayad G, Polge AS, et al. Echocardiography predictors and prognostic value of pulmonary artery systolic pressure in chronic organic mitral regurgitation. Heart (2010) 96(16):1311–7. doi: 10.1136/hrt.2009.186486
13. Kusunose K, Goodman A, Parikh R, Barr T, Agarwal S, Popovic ZB, et al. Incremental prognostic value of left ventricular global longitudinal strain in patients with aortic stenosis and preserved ejection fraction. Circ Cardiovasc Imaging (2014) 7(6):938–45. doi: 10.1161/CIRCIMAGING.114.002041
14. Luçon A, Oger E, Bedossa M, Boulmier D, Verhoye JP, Eltchaninoff H, et al. Prognostic implications of pulmonary hypertension in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation: study from the FRANCE 2 Registry. Circ Cardiovasc Interv (2014) 7(2):240–7. doi: 10.1161/CIRCINTERVENTIONS.113.000482
15. Urena M, Webb JG, Eltchaninoff H, Muñoz-García AJ, Bouleti C, Tamburino C, et al. Late cardiac death in patients undergoing transcatheter aortic valve replacement: incidence and predictors of advanced heart failure and sudden cardiac death. J Am Coll Cardiol (2015) 65(5):437–48. doi: 10.1016/j.jacc.2014.11.027
16. Lindman BR, Maniar HS, Jaber WA, Lerakis S, Mack MJ, Suri RM, et al. Effect of tricuspid regurgitation and the right heart on survival after transcatheter aortic valve replacement: insights from the placement of aortic transcatheter valves II inoperable cohort. Circ Cardiovasc Interv (2015) 8(4):e002073. doi: 10.1161/CIRCINTERVENTIONS.114.002073
17. Bishu K, Suri RM, Nkomo VT, Kane GC, Greason KL, Reeder GS, et al. Prognostic impact of pulmonary artery systolic pressure in patients undergoing transcatheter aortic valve replacement for aortic stenosis. Am J Cardiol (2014) 114(10):1562–7. doi: 10.1016/j.amjcard.2014.08.019
18. O'Sullivan CJ, Wenaweser P, Ceylan O, Rat-Wirtzler J, Stortecky S, Heg D, et al. Effect of pulmonary hypertension hemodynamic presentation on clinical outcomes in patients with severe symptomatic aortic valve stenosis undergoing transcatheter aortic valve implantation: insights from the new proposed pulmonary hypertension classification. Circ Cardiovasc Interv (2015) 8(7):e002358. doi: 10.1161/CIRCINTERVENTIONS.114.002358
19. Généreux P, Pibarot P, Redfors B, Mack MJ, Makkar RR, Jaber WA, et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur Heart J (2017) 38(45):3351–8. doi: 10.1093/eurheartj/ehx381
20. Melby SJ, Moon MR, Lindman BR, Bailey MS, Hill LL, Damiano RJ. Impact of pulmonary hypertension on outcomes after aortic valve replacement for aortic valve stenosis. J Thorac Cardiovasc Surg (2011) 141(6):1424–30. doi: 10.1016/j.jtcvs.2011.02.028
21. Nijenhuis VJ, Huitema MP, Vorselaars VM, Swaans MJ, de Kroon T, van der Heyden JA, et al. Echocardiographic pulmonary hypertension probability is associated with clinical outcomes after transcatheter aortic valve implantation. Int J Cardiol (2016) 225:218–25. doi: 10.1016/j.ijcard.2016.10.010
22. Levy F, Bohbot Y, Sanhadji K, Rusinaru D, Ringle A, Delpierre Q, et al. Impact of pulmonary hypertension on long-term outcome in patients with severe aortic stenosis. Eur Heart J Cardiovasc Imaging (2017) 9. doi: 10.1093/ehjci/jex166
23. Barbash IM, Escarcega RO, Minha S, Ben-Dor I, Torguson R, Goldstein SA, et al. Prevalence and impact of pulmonary hypertension on patients with aortic stenosis who underwent transcatheter aortic valve replacement. Am J Cardiol (2015) 115(10):1435–42. doi: 10.1016/j.amjcard.2015.02.022
24. Magne J, Mohty D, Piccardo A, Boulogne C, Deltreuil M, Petitalot V, et al. Impact of pulmonary hypertension on outcome in patients with severe aortic stenosis and preserved left ventricular ejection fraction. Clin Res Cardiol (2017) 106(7):542–50. doi: 10.1007/s00392-017-1085-2
25. Lindman BR, Zajarias A, Maniar HS, Miller DC, Suri RM, Arnold SV, et al. Risk stratification in patients with pulmonary hypertension undergoing transcatheter aortic valve replacement. Heart (2015) 101(20):1656–64. doi: 10.1136/heartjnl-2015-308001
26. Franzone A, O'Sullivan CJ, Stortecky S, Heg D, Lanz J, Vollenbroich R, et al. Prognostic impact of invasive haemodynamic measurements in combination with clinical and echocardiographic characteristics on two-year clinical outcomes of patients undergoing transcatheter aortic valve implantation. EuroIntervention (2017) 12(18):e2186–e2193. doi: 10.4244/EIJ-D-16-00790
27. Cam A, Goel SS, Agarwal S, Menon V, Svensson LG, Tuzcu EM, et al. Prognostic implications of pulmonary hypertension in patients with severe aortic stenosis. J Thorac Cardiovasc Surg (2011) 142(4):800–8. doi: 10.1016/j.jtcvs.2010.12.024
28. Sinning JM, Hammerstingl C, Chin D, Ghanem A, Schueler R, Sedaghat A, et al. Decrease of pulmonary hypertension impacts on prognosis after transcatheter aortic valve replacement. EuroIntervention (2014) 9(9):1042–9. doi: 10.4244/EIJV9I9A177
29. Ben-Dor I, Goldstein SA, Pichard AD, Satler LF, Maluenda G, Li Y, et al. Clinical profile, prognostic implication, and response to treatment of pulmonary hypertension in patients with severe aortic stenosis. Am J Cardiol (2011) 107(7):1046–51. doi: 10.1016/j.amjcard.2010.11.031
30. Masri A, Abdelkarim I, Sharbaugh MS, Althouse AD, Xu J, Han W, et al. Outcomes of persistent pulmonary hypertension following transcatheter aortic valve replacement. Heart (2017):heartjnl-2017-311978. doi: 10.1136/heartjnl-2017-311978
31. Testa L, Latib A, de Marco F, de Carlo M, Fiorina C, Montone R, et al. Persistence of severe pulmonary hypertension after transcatheter aortic valve replacement: incidence and prognostic impact. Circ Cardiovasc Interv (2016) 9(6). doi: 10.1161/CIRCINTERVENTIONS.115.003563
32. D'Ascenzo F, Conrotto F, Salizzoni S, Rossi ML, Nijhoff F, Gasparetto V, et al. Incidence, predictors, and impact on prognosis of systolic pulmonary artery pressure and its improvement after transcatheter aortic valve implantation: a multicenter registry. J Invasive Cardiol (2015) 27(2):114–9.
33. Roselli EE, Abdel Azim A, Houghtaling PL, Jaber WA, Blackstone EH. Pulmonary hypertension is associated with worse early and late outcomes after aortic valve replacement: implications for transcatheter aortic valve replacement. J Thorac Cardiovasc Surg (2012) 144(5):1067–74. doi: 10.1016/j.jtcvs.2012.08.029
34. Schewel D, Schewel J, Martin J, Voigtländer L, Frerker C, Wohlmuth P, et al. Impact of transcatheter aortic valve implantation (TAVI) on pulmonary hyper-tension and clinical outcome in patients with severe aortic valvular stenosis. Clin Res Cardiol (2015) 104(2):164–74. doi: 10.1007/s00392-014-0772-5
35. Khandhar S, Varadarajan P, Turk R, Sampat U, Patel R, Kamath A, et al. Survival benefit of aortic valve replacement in patients with severe aortic regurgitation and pulmonary hypertension. Ann Thorac Surg (2009) 88(3):752–6. doi: 10.1016/j.athoracsur.2009.05.025
36. Rosenkranz S, Gibbs JS, Wachter R, de Marco T, Vonk-Noordegraaf A, Vachiéry JL. Left ventricular heart failure and pulmonary hypertension. Eur Heart J (2016) 37(12):942–54. doi: 10.1093/eurheartj/ehv512
37. Hoeper MM, Lam CSP, Vachiery JL, Bauersachs J, Gerges C, Lang IM, et al. Pulmonary hypertension in heart failure with preserved ejection fraction: a plea for proper phenotyping and further research. Eur Heart J (2017) 38(38):2869–73. doi: 10.1093/eurheartj/ehw597
38. Fayyaz AU, Edwards WD, Maleszewski JJ, Konik EA, Dubrock HM, Borlaug BA, et al. Global pulmonary vascular remodeling in pulmonary hypertension associated with heart failure and preserved or reduced ejection fraction. Circulation (2018) 137(17):CIRCULATIONAHA.117.031608. doi: 10.1161/CIRCULATIONAHA.117.031608
39. Le Tourneau T, Deswarte G, Lamblin N, Foucher-Hossein C, Fayad G, Richardson M, et al. Right ventricular systolic function in organic mitral regurgitation: impact of biventricular impairment. Circulation (2013) 127(15):1597–608. doi: 10.1161/CIRCULATIONAHA.112.000999
40. Kammerlander AA, Marzluf BA, Graf A, Bachmann A, Kocher A, Bonderman D, et al. Right ventricular dysfunction, but not tricuspid regurgitation, is associated with outcome late after left heart valve procedure. J Am Coll Cardiol (2014) 64(24):2633–42. doi: 10.1016/j.jacc.2014.09.062
41. Baumgartner H, Falk V, Bax JJ, de Bonis M, Hamm C, Holm PJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J (2017) 38(36):2739–91. doi: 10.1093/eurheartj/ehx391
42. Robbins IM, Hemnes AR, Pugh ME, Brittain EL, Zhao DX, Piana RN, et al. High prevalence of occult pulmonary venous hypertension revealed by fluid challenge in pulmonary hypertension. Circ Heart Fail (2014) 7(1):116–22. doi: 10.1161/CIRCHEARTFAILURE.113.000468
43. Magne J, Lancellotti P, Piérard LA. Exercise pulmonary hypertension in asymptomatic degenerative mitral regurgitation. Circulation (2010) 122(1):33–41. doi: 10.1161/CIRCULATIONAHA.110.938241
44. Magne J, Lancellotti P, Pierard LA. Stress echocardiography and mitral valvular heart disease. Cardiol Clin (2013) 31(2):311–21. doi: 10.1016/j.ccl.2013.03.008
45. Lancellotti P, Magne J, Dulgheru R, Ancion A, Martinez C, Piérard LA. Clinical significance of exercise pulmonary hypertension in secondary mitral regurgitation. Am J Cardiol (2015) 115(10):1454–61. doi: 10.1016/j.amjcard.2015.02.028
46. Lancellotti P, Magne J, Donal E, O'Connor K, Dulgheru R, Rosca M, et al. Determinants and prognostic significance of exercise pulmonary hypertension in asymptomatic severe aortic stenosis. Circulation (2012) 126(7):851–9. doi: 10.1161/CIRCULATIONAHA.111.088427
47. Lam CS, Roger VL, Rodeheffer RJ, Borlaug BA, Enders FT, Redfield MM. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol (2009) 53(13):1119–26. doi: 10.1016/j.jacc.2008.11.051
48. Borlaug BA, Obokata M. Is it time to recognize a new phenotype? Heart failure with preserved ejection fraction with pulmonary vascular disease. Eur Heart J (2017) 38(38):2874–8. doi: 10.1093/eurheartj/ehx184
49. Nunes MC, Hung J, Barbosa MM, Esteves WA, Carvalho VT, Lodi-Junqueira L, et al. Impact of net atrioventricular compliance on clinical outcome in mitral stenosis. Circ Cardiovasc Imaging (2013) 6(6):1001–8. doi: 10.1161/CIRCIMAGING.112.000328
50. Enriquez-Sarano M, Tajik AJ, Schaff HV, Orszulak TA, Mcgoon MD, Bailey KR, et al. Echocardiographic prediction of left ventricular function after correction of mitral regurgitation: results and clinical implications. J Am Coll Cardiol (1994) 24(6):1536–43. doi: 10.1016/0735-1097(94)90151-1
51. Tribouilloy C, Rusinaru D, Grigioni F, Michelena HI, Vanoverschelde JL, Avierinos JF, et al. Long-term mortality associated with left ventricular dysfunction in mitral regurgitation due to flail leaflets: a multicenter analysis. Circ Cardiovasc Imaging (2014) 7(2):363–70. doi: 10.1161/CIRCIMAGING.113.001251
52. Messika-Zeitoun D, Bellamy M, Avierinos JF, Breen J, Eusemann C, Rossi A, et al. Left atrial remodelling in mitral regurgitation--methodologic approach, physiological determinants, and outcome implications: a prospective quantitative Doppler-echocardiographic and electron beam-computed tomographic study. Eur Heart J (2007) 28(14):1773–81. doi: 10.1093/eurheartj/ehm199
53. Rusinaru D, Tribouilloy C, Grigioni F, Avierinos JF, Suri RM, Barbieri A, et al. Left atrial size is a potent predictor of mortality in mitral regurgitation due to flail leaflets: results from a large international multicenter study. Circ Cardiovasc Imaging (2011) 4(5):473–81. doi: 10.1161/CIRCIMAGING.110.961011
54. Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Fleisher LA, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation (2017) 135(25):e1159–95. doi: 10.1161/CIR.0000000000000503
55. Enriquez-Sarano M, Rossi A, Seward JB, Bailey KR, Tajik AJ. Determinants of pulmonary hypertension in left ventricular dysfunction. J Am Coll Cardiol (1997) 29(1):153–9. doi: 10.1016/S0735-1097(96)00436-6
56. Goliasch G, Bartko PE, Neuhold S, Pavo N, Wurm R, Mascherbauer J, et al. P3543Refining the prognostic impact of functional mitral regurgitation in chronic heart failure. Eur Heart J (2017) 38(suppl 1). doi: 10.1093/eurheartj/ehx504.P3543
57. Miller WL, Mahoney DW, Enriquez-Sarano M. Quantitative Doppler-echocardiographic imaging and clinical outcomes with left ventricular systolic dysfunction: independent effect of pulmonary hypertension. Circ Cardiovasc Imaging (2014) 7(2):330–6. doi: 10.1161/CIRCIMAGING.113.001184
58. Dupont M, Mullens W, Skouri HN, Abrahams Z, Wu Y, Taylor DO, et al. Prognostic role of pulmonary arterial capacitance in advanced heart failure. Circ Heart Fail (2012) 5(6):778–85. doi: 10.1161/CIRCHEARTFAILURE.112.968511
59. Gaemperli O, Biaggi P, Gugelmann R, Osranek M, Schreuder JJ, Bühler I, et al. Real-time left ventricular pressure-volume loops during percutaneous mitral valve repair with the MitraClip system. Circulation (2013) 127(9):1018–27. doi: 10.1161/CIRCULATIONAHA.112.135061
60. Matsumoto T, Nakamura M, Yeow WL, Hussaini A, Ram V, Makar M, et al. Impact of pulmonary hypertension on outcomes in patients with functional mitral regurgitation undergoing percutaneous edge-to-edge repair. Am J Cardiol (2014) 114(11):1735–9. doi: 10.1016/j.amjcard.2014.08.044
61. Grayburn PA, Foster E, Sangli C, Weissman NJ, Massaro J, Glower DG, et al. Relationship between the magnitude of reduction in mitral regurgitation severity and left ventricular and left atrial reverse remodeling after MitraClip therapy. Circulation (2013) 128(15):1667–74. doi: 10.1161/CIRCULATIONAHA.112.001039
62. Geis NA, Puls M, Lubos E, Zuern CS, Franke J, Schueler R, et al. Safety and efficacy of MitraClip™ therapy in patients with severely impaired left ventricular ejection fraction: results from the German transcatheter mitral valve interventions (TRAMI) registry. Eur J Heart Fail (2018) 20(3):598-608. doi: 10.1002/ejhf.910
63. Kampaktsis PN, Kokkinidis DG, Wong SC, Vavuranakis M, Skubas NJ, Devereux RB. The role and clinical implications of diastolic dysfunction in aortic stenosis. Heart (2017) 103(19):1481–7. doi: 10.1136/heartjnl-2017-311506
64. Melenovsky V, Hwang SJ, Redfield MM, Zakeri R, Lin G, Borlaug BA. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail (2015) 8(2):295–303. doi: 10.1161/CIRCHEARTFAILURE.114.001667
65. Borlaug BA. The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol (2014) 11(9):507–15. doi: 10.1038/nrcardio.2014.83
66. Hoendermis ES, Liu LC, Hummel YM, van der Meer P, de Boer RA, Berger RM, et al. Effects of sildenafil on invasive haemodynamics and exercise capacity in heart failure patients with preserved ejection fraction and pulmonary hypertension: a randomized controlled trial. Eur Heart J (2015) 36(38):2565–73. doi: 10.1093/eurheartj/ehv336
67. Maeder MT, Thompson BR, Brunner-La Rocca HP, Kaye DM. Hemodynamic basis of exercise limitation in patients with heart failure and normal ejection fraction. J Am Coll Cardiol (2010) 56(11):855–63. doi: 10.1016/j.jacc.2010.04.040
68. Clavel MA, Magne J, Pibarot P. Low-gradient aortic stenosis. Eur Heart J (2016) 37(34):2645–57. doi: 10.1093/eurheartj/ehw096
69. Calin A, Mateescu AD, Rosca M, Beladan CC, Enache R, Botezatu S, et al. Left atrial dysfunction as a determinant of pulmonary hypertension in patients with severe aortic stenosis and preserved left ventricular ejection fraction. Int J Cardiovasc Imaging (2017) 33(12):1939–47. doi: 10.1007/s10554-017-1211-2
70. Tang M, Liu X, Lin C, He Y, Cai X, Xu Q, et al. Meta-analysis of outcomes and evolution of pulmonary hypertension before and after transcatheter aortic valve implantation. Am J Cardiol (2017) 119(1):91–9. doi: 10.1016/j.amjcard.2016.09.015
71. Gonçalves A, Marcos-Alberca P, Almeria C, Feltes G, Rodríguez E, Hernández-Antolín RA, et al. Acute left ventricle diastolic function improvement after transcatheter aortic valve implantation. Eur J Echocardiogr (2011) 12(10):790–7. doi: 10.1093/ejechocard/jer147
72. Spethmann S, Dreger H, Baldenhofer G, Stüer K, Saghabalyan D, Müller E, et al. Short-term effects of transcatheter aortic valve implantation on left atrial mechanics and left ventricular diastolic function. J Am Soc Echocardiogr (2013) 26(1):64–71. doi: 10.1016/j.echo.2012.10.002
73. D'Ascenzi F, Cameli M, Henein M, Iadanza A, Reccia R, Lisi M, et al. Left atrial remodelling in patients undergoing transcatheter aortic valve implantation: a speckle-tracking prospective, longitudinal study. Int J Cardiovasc Imaging (2013) 29(8):1717–24. doi: 10.1007/s10554-013-0265-z
74. Barone-Rochette G, Piérard S, de Meester de Ravenstein C, Seldrum S, Melchior J, Maes F, et al. Prognostic significance of LGE by CMR in aortic stenosis patients undergoing valve replacement. J Am Coll Cardiol (2014) 64(2):144–54. doi: 10.1016/j.jacc.2014.02.612
75. Treibel TA, López B, González A, Menacho K, Schofield RS, Ravassa S, et al. Reappraising myocardial fibrosis in severe aortic stenosis: an invasive and non-invasive study in 133 patients. Eur Heart J (2018) 39(8):699–709. doi: 10.1093/eurheartj/ehx353
76. Chin CWL, Everett RJ, Kwiecinski J, Vesey AT, Yeung E, Esson G, et al. Myocardial fibrosis and cardiac decompensation in aortic stenosis. JACC Cardiovasc Imaging (2017) 10(11):1320–33. doi: 10.1016/j.jcmg.2016.10.007
77. Carabello BA. Aortic regurgitation. A lesion with similarities to both aortic stenosis and mitral regurgitation. Circulation (1990) 82(3):1051–3. doi: 10.1161/01.CIR.82.3.1051
78. Toggweiler S, Boone RH, Rodés-Cabau J, Humphries KH, Lee M, Nombela-Franco L, et al. Transcatheter aortic valve replacement: outcomes of patients with moderate or severe mitral regurgitation. J Am Coll Cardiol (2012) 59(23):2068–74. doi: 10.1016/j.jacc.2012.02.020
79. Zimpfer D, Zrunek P, Roethy W, Czerny M, Schima H, Huber L, et al. Left ventricular assist devices decrease fixed pulmonary hypertension in cardiac transplant candidates. J Thorac Cardiovasc Surg (2007) 133(3):689–95. doi: 10.1016/j.jtcvs.2006.08.104
80. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J (2016) 37(27):2129–200. doi: 10.1093/eurheartj/ehw128
81. Pfeffer MA, Claggett B, Assmann SF, Boineau R, Anand IS, Clausell N, et al. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation (2015) 131(1):34–42. doi: 10.1161/CIRCULATIONAHA.114.013255
82. de Denus S, O'Meara E, Desai AS, Claggett B, Lewis EF, Leclair G, et al. Spironolactone Metabolites in TOPCAT - New Insights into Regional Variation. N Engl J Med (2017) 376(17):1690–2. doi: 10.1056/NEJMc1612601
83. Bermejo J, Yotti R, García-Orta R, Sánchez-Fernández PL, Castaño M, Segovia-Cubero J, et al. Sildenafil for improving outcomes in patients with corrected valvular heart disease and persistent pulmonary hypertension: a multicenter, double-blind, randomized clinical trial. Eur Heart J (2017). doi: 10.1093/eurheartj/ehx700
Keywords: pulmonary hypertension, post-capillary, pre-capillary, combined pre- and post-capillary, valve disease, aortic stenosis, mitral regurgitation
Citation: Maeder MT, Weber L, Buser M, Gerhard M, Haager PK, Maisano F and Rickli H (2018). Pulmonary Hypertension in Aortic and Mitral Valve Disease. Front. Cardiovasc. Med. 5:40. doi: 10.3389/fcvm.2018.00040
Received: 12 February 2018; Accepted: 13 April 2018;
Published: 23 May 2018
Reviewed by:
Moritz Seiffert, University Heart Center Hamburg GmbH, GermanyCopyright © 2018 Maeder, Weber, Buser, Gerhard, Haager, Maisano and Rickli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Micha T. Maeder, micha.maeder@kssg.ch
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.