- 1Systemomics Center, College of Pharmacy, and Genomics Research Center (State-Province Key Laboratories of Biomedicine-Pharmaceutics of China), Harbin Medical University, Harbin, China
- 2HMU-UCCSM Centre for Infection and Genomics, Harbin Medical University, Harbin, China
- 3Translational Medicine Research and Cooperation Center of Northern China, Heilongjiang Academy of Medical Sciences, Harbin, China
- 4College of Bioinformatics Science and Technology, Harbin Medical University, Harbin, China
- 5Department of Colorectal Cancer, The 2nd Affiliated Hospital of Harbin Medical University, Harbin, China
- 6Department of Epidemiology, Public Health School, Harbin Medical University, Harbin, China
- 7Department of Infectious Diseases, The First Affiliated Hospital, Harbin Medical University, Harbin, China
- 8Department of Respiration, The Third Affiliated Hospital of Harbin Medical University, Harbin, China
- 9Department of Microbiology, Immunology and Infectious Diseases, University of Calgary, Calgary, AB, Canada
Lung cancer (LC) is one of the most serious malignant tumors, which has the fastest growing morbidity and mortality worldwide. A role of the lung microbiota in LC pathogenesis has been analyzed, but a comparable role of the gut microbiota has not yet been investigated. In this study, the gut microbiota of 30 LC patients and 30 healthy controls were examined via next-generation sequencing of 16S rRNA and analyzed for diversity and biomarkers. We found that there was no decrease in significant microbial diversity (alpha diversity) in LC patients compared to controls (P observed = 0.1422), while the composition (beta diversity) differed significantly between patients and controls (phylum [stress = 0.153], class [stress = 0.16], order [stress = 0.146], family [stress = 0.153]). Controls had a higher abundance of the bacterial phylum Actinobacteria and genus Bifidobacterium, while patients with LC showed elevated levels of Enterococcus. These bacteria were found as possible biomarkers for LC. A decline of normal function of the gut microbiome in LC patients was also observed. These results provide the basic guidance for a systematic, multilayered assessment of the role of the gut microbiome in LC, which has a promising potential for early prevention and targeted intervention.
Introduction
Lung cancer (LC) is one of the deadliest malignancies, which has growing morbidity and mortality worldwide. It poses an enormous threat to the human health (Torre et al., 2015). Research on LC genetics and biology has opened opportunities for novel therapeutic strategies against the disease (Allison, 2015; Chowdhury et al., 2018; Hendriks and Besse, 2018; Herbst et al., 2018; Lissanu Deribe et al., 2018; Wei et al., 2018), but the knowledge about the etiology remains incomplete, making precision treatment or prevention a moving target. To date, the major etiological causes or risk factors facilitating the pathogenesis of cancers have been mostly focused on genetic susceptibility and carcinogenic environments (Addario, 2014; Gibbons et al., 2014; Liu et al., 2014), but people with high genetic or environmental risk factors may not develop the malignancies even at advanced ages. Conversely, in many cancer patients, clear familial or environmental risk factors are often non-traceable. These facts indicate the existence of additional major factors that influence the onset and development of cancers.
Over the past few decades, numerous discoveries have been reported regarding the gut microbiome for its roles in diseases with a particular focus on cancers (Jobin, 2012; Schwabe and Jobin, 2013; Gagliani et al., 2014). The diverse microbes in the human gut, 10-fold more than the total cells of the human host, with millions of total non-redundant genes, maintain a dynamic stable and healthy microenvironment inside the host. In cancer patients, the composition of the gut microbiota often becomes radically different from that in healthy individuals, for example, increased Porphyromonas, Enterococcus, Streptococcus, or Peptostreptococcus and decreased Roseburia or other beneficial microbes, such as butyrate-producing bacteria of the family Lachnospiraceae in cases of colorectal cancer (CRC) (Wang et al., 2012; Nakatsu et al., 2015). Meanwhile, the relative ratios and abundance of the resident microbes may also be directly associated with cancer, which have also been reported in CRC patients, such as Streptococcus bovis biotype I (Boleij et al., 2011), E. coli harboring pks (Cuevas-Ramos et al., 2010), and Bacteroides fragilis secreting DNA-damaging toxins (Toprak et al., 2006; Wu et al., 2009). Bacteria that are protective against cancer are also documented, such as Lactobacillus rhamnosus GG and Lactobacillus acidophilus (Neish, 2009; Verma and Shukla, 2013). In a recent study, we identified and characterized a large number of highly diverse anticancer bacteria from the gut of healthy individual, which had potent suppressive effects against a broad spectrum of cancer cell types in vitro and stopped the growth of tumors in a mouse model of human ovarian cancer. In this cancer model, the metastasized cancer cells were also cleared by intratumoral administration of the bacterial culture supernatant (Zhou et al., 2017). The highly effective anticancer activities of such commensal microbes have been detected in most participants of different age groups, demonstrating the existence of a strong cancer-defensive system parallel to the immune system in the human body (Zhou et al., 2017). Additionally, the high diversity of the cancer-suppressing bacteria targeting different cancer types suggests personalized anticancer microbial allies within individual hosts, which may confer different levels of resistance against or susceptibility to specific cancer types. Such speculations point to a possibility that cancers in a particular organ may have certain common features in the microbiome of the patients.
However, for LC, previous analyses focus on the relationship between LC and lung microbiome, where the microbes have direct contact with the lung tissues (Hosgood et al., 2014; Tsay et al., 2018). It is then a natural question whether there exists a dysbiosis of the gut microbiome in patients with LC. Studies of the gut microbiome composition in patients with LC and analysis of the effects of the gut microbiome on LC are urgently needed. Therefore, we tested whether LC patients differ in gut microecology when compared to healthy controls.
Materials and Methods
Study Participants
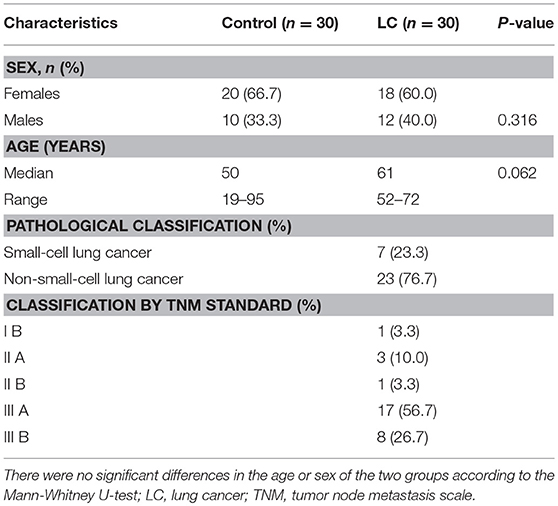
A total of 60 fecal samples were collected from 30 LC patients (median age: 61) and 30 matched healthy controls from the Department of Respiration, The Third Affiliated Hospital of Harbin Medical University (Table 1). All the LC patients were diagnosed according to their histopathological features using tumor node metastasis (TNM) scale classification of malignant tumors after surgery. The patients and healthy controls had not taken any medications in the 3 months before specimen collection. Informed consent was obtained from all participants. The fecal specimens were frozen in liquid nitrogen immediately after sampling and stored in a −80°C freezer.
DNA Extraction and PCR Amplification
Total DNA extraction from the samples was conducted according to the instructions of the OMG-soil kit (Omega Bio-tek, Norcross, GA, USA). DNA concentration and purity were determined using NanoDrop2000 (Thermo Fisher Scientific, Waltham, MA, USA), and the quality of the extracted DNA was inspected by 1% agarose gel electrophoresis. PCR amplification of the V3-V4 variable region was performed using 338F (5′-ACTCCTACGGGAGGCAGCAG-3′) and 806R (5′-GGACTACHVGGGTWTCTAAT-3′) primers by the following amplification procedure: pre-denaturation at 95°C for 3 min, 27 cycles (denaturation at 95°C for 30 s, annealing at 55°C for 30 s, extension at 72°C for 30 s), and extension at 72°C for 10 min (PCR: ABI GeneAmp® 9700). The amplification was conducted in a 20 μL volume containing 4 μL of 5 × FastPfu buffer, 2 μL of 2.5 mM dNTPs, 0.8 μL of primer (5 μM), 0.4 μL of FastPfu polymerase, and 10 ng of DNA template.
Illumina Miseq Sequencing
The PCR products were recovered using a 2% agarose gel, purified using an AxyPrep DNA Gel Extraction Kit (Axygen Biosciences, Union City, CA, USA), eluted with Tris-HCl, and detected by 2% agarose electrophoresis. Quantification was performed using QuantiFluorTM-ST (Promega, Madison, WI, USA). The purified amplified fragment was included in a library of PE 2 × 300 according to the standard operating protocol of the Illumina MiSeq platform (Illumina, San Diego, CA, USA).
The steps of library construction were as follows: (1) connecting the “Y” shaped joint, (2) removing the self-ligated fragments using magnetic beads, (3) enriching the library by PCR amplification, and (4) denaturing DNA by sodium hydroxide. Sequencing was carried out on the Illumina Miseq PE300 platform (Shanghai Meiji Biomedical Technology Co., Ltd, Shanghai, China), and the raw data were uploaded to the NCBI database.
Data Processing
The raw sequence data were handled using Trimmomatic software and spliced using the FLASH software as follows:
(1) We first set a 50-bp window. If the average quality value in the window was lower than 20, all sequences at the back end of the base were truncated from the front-end position of the window, and then the sequences having a length <50 bp after the quality control were removed.
(2) According to the base overlap, the sequences of the two ends were spliced, and the maximum mismatch rate between overlaps was set to 0.2, with a length >10 bp. All remaining sequences were abandoned.
(3) According to the barcode and primers at both ends of the sequence, a sequence was assigned to a sample. In this process, the barcode had to be precisely matched, and the primer was allowed two base mismatches.
The UPARSE software (version 7.1 http://drive5.com/uparse/) was used to perform the clustering of operational taxonomic units (OTUs) on the sequences with 97% or greater similarity of the 16S rDNA sequences and to remove single sequences and chimeras during the clustering. Each sequence was annotated with a species classification using the RDP classifier (http://rdp.cme.msu.edu/), and the alignment threshold was set to 70% compared to the Silva database (SSU123).
Alpha/Beta Diversity Analysis and Taxonomic Plots
Alpha diversity analysis was used to investigate bacterial species diversity in gut ecosystems between the LC group and healthy controls. Information, such as species abundance, was obtained by observing various index values like Chao, Shannon, Ace, and Simpson, and then a statistical t-test was used to detect whether the index value between the two groups was significantly different. Here, we selected the Shannon index as a metric to analyze the community richness and evenness between the two groups. Inter-group comparisons were performed using a Wilcoxon rank sum test of non-parametric data. A t-test was applied after the results were reflected as visual metrics using a histogram.
Beta diversity analysis represents a comparison of microbial community composition and is used here to assess differences between microbial community composition. The basic output of this comparison is a distance matrix that represents the difference between every two samples in the community. NMDS analysis (non-metric multidimensional scaling) was chosen for the sample similarity comparison between the LC group and the healthy controls. This is a method of simplifying, analyzing, and categorizing research objects (samples or quantities) in a multidimensional space into low-dimensional spaces, while retaining a method for analyzing raw relational data between objects. The basic feature is to regard the similarity or dissimilarity data between objects as a monotonic function of point distance. On the basis of maintaining the original data order relationship, the original data are replaced with new identical data columns for metric multidimensional scaling analysis. This approach simplifies the study objects (samples or quantities) in a multidimensional space into low-dimensional spaces for localization, analysis, and categorization, while preserving the original relationships between objects. The basic feature of NMDS is to regard the similarity or dissimilarity data between objects as a monotonic function of point distance and replace the original data with new identical data columns for metric multidimensional scaling analysis on the basis of maintaining the original data order.
To determine potential bacterial biomarkers that differ in abundance and occurrence between the LC group and healthy controls, LEfSe analysis in multi-level species was used (Puri et al., 2018). LEfSe is a software package for discovering high-dimensional biomarkers with inputs that include genes, metabolites, and classification. We first used the non-parametric factorial Kruskal-Wallis (KW) sum-rank test to detect specific species relating significant abundance differences in two groups. We then estimated the effect of each component (species) by LEfSe linear discriminant analysis (LDA). In order to detect the species contributing to the abundance differences in different groups of microbial communities, we carried out a test of significance differences between groups. Based on the obtained community abundance data, rigorous statistical methods were used to detect species with different richness in different groups (samples) of microbial communities, and hypothesis testing was performed to assess the significance of these observed differences.
16S Function Prediction Analysis
“16S function prediction analysis” was implemented to obtain functional information of the gut microbiome between LC patients and healthy controls (Ravi et al., 2018). We normalized the OTU abundance table by using PICRUSt (the PICRUSt software stores the COG (Clusters of Orthologous Groups of proteins) letter KO (KEGG Ontology) information corresponding to the greengene id) (Douglas et al., 2018), i.e., to remove the effect of the number of copies of the 16S marker gene in the species group. The COG family information corresponding to the OTU was obtained by using the GreenGene ID corresponding to each OTU. The abundance of each COG was calculated. According to the COG database information, the description information of each COG and its work information was parsed from the eggNOG database to obtain a functional abundance spectrum (Huerta-Cepas et al., 2016).
The functional abundance spectrum reflected different levels of expression of related functional proteins or specific metabolic capacity of microbiome. By combining the distribution of the research objects in various functional categories, we had the opportunity to make a conclusion for the role of gut microbiota in the development of LC.
Implementation of Statistical Analysis
All statistical calculations were performed in R 3.4.3. The correction of the P-value is responsible for the false discovery rate (FDR).
Results
Raw Data Management
After curation of the sequences, a total of 2,682,019 sequence fragments were obtained from the 60 samples, with an average length of 433 bp. To facilitate the storage and sharing of high-throughput sequencing data generated in this work, we uploaded the original sequence file of 1,162,191,785 bp to the NCBI large-capacity database SRA (Sequence Read Archive, http://www.ncbi.nlm.nih.gov/Traces/sra Accession: PRJNA507734).
OTU Clustering and Evaluation
We obtained 740 OTUs by statistical analysis of the 16S rDNA sequences at a 97% similarity level. The community composition of each sample was statistically analyzed at the taxonomical ranks of phylum, class, order, family, genus, and species (i.e., OTU here). We constructed a rarefaction curve based on the number of sequences drawn. The Shannon-Wiener curve tended to be flat, indicating that the sequencing depth was sufficient to reflect the microbial diversity in the sample (Figure S1).
No significant difference was observed in alpha diversity between LC patients and healthy controls.
The results of alpha diversity analysis were quantified by the Shannon index, which relates both the evenness and richness of a total of 740 OTUs obtained from the LC group and healthy controls. Figure 1 reflected the alpha diversity measurements for LC patients vs. healthy controls. The Shannon index of OTU level of healthy controls and LC patients were 3.28 and 3.09, respectively. Statistical testing using Welch's t-test showed no significant difference for Shannon diversity for the observed species (P observed = 0.1422).

Figure 1. The abscissa is the group name, and the ordinate is the exponential average of each group (0.01 < P ≤ 0.05 marked as *, 0.001 < P ≤ 0.01 marked as **P ≤ 0.001 marked as***). LC: lung cancer.
LC Patients and Controls Differ in Gut Microbial Composition
As a dimensionality reduction-based approach, NMDS (Non-metric multidimensional scaling) analysis was applied for dissimilarities in the microbial composition between LC patients and healthy controls (Noval Rivas et al., 2013). Results from NMDS are displayed in Figure 2. Patients with LC (blue dots) showed a shift to the left, which indicated compositional differences, and is measured by the NMDS intensity index (stress = 0.153 on phylum level). The separation intensity in other levels were as follows: class (stress = 0.16), order (stress = 0.146), family (0.153), and genus (0.21, unexplanatory meaning), the graphics of which are summarized in Figure S2.
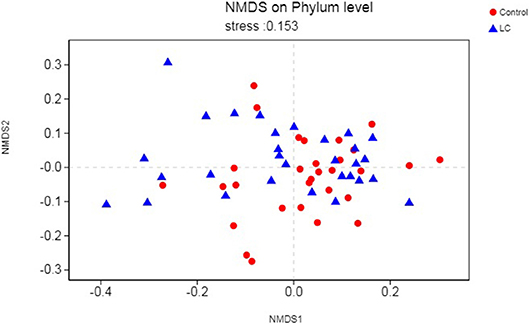
Figure 2. Points of blue colors or shapes represent LC samples; red colors or shapes represent samples of control. The closer the two sample points are, the more similar the composition of the two sample species is. The horizontal and vertical coordinates represent relative distances and have no practical significance. It is generally considered that stress <0.2 can be expressed by the two-dimensional dot pattern of NMDS, and its graph has a certain explanatory meaning. LC, lung cancer.
Specific Species in Multi-Level Tests
The multi-level LEfSe analysis for biomarkers was used to find significantly imbalanced species between LC patients and healthy controls, which showed substantially differentiated the two groups. LEfSe results illustrated 47 bacterial taxonomic clades having statistically significant differences (33 increased and 14 decreased) in LC patients. At the phylum level, increased Actinobacteria was detected as the strongest marker in healthy controls (Figure 3). Analysis at the class level also showed elevated levels of Actinobacteria in healthy individuals (Figure 3). At the order level, Bifidobacteriales showed a greater abundance in healthy controls (Figure 3). At the family level, increased bacteria such as Bifidobacteriaceae and Coriobacteriaceae were detected as markers in the control group and Enterococcaceae in the LC group (Figure 3). Numerous differential bacterial biomarkers were found at the genus level (Figure 3). Again, a multi-level Wilcoxon rank-sum test bar plot confirmed the above findings. A difference significance test between the two groups was based on the obtained community abundance data for hypothesis testing, and the significance of the difference was observed (Table 2, Figure S3). Combined with the results of the LEfSe test, the differences in species composition were judged mainly from Actinobacteria (P = 0.041), Bifidobacterium (P = 0.012) and Enterococcus (P = 0.018; Table 2).
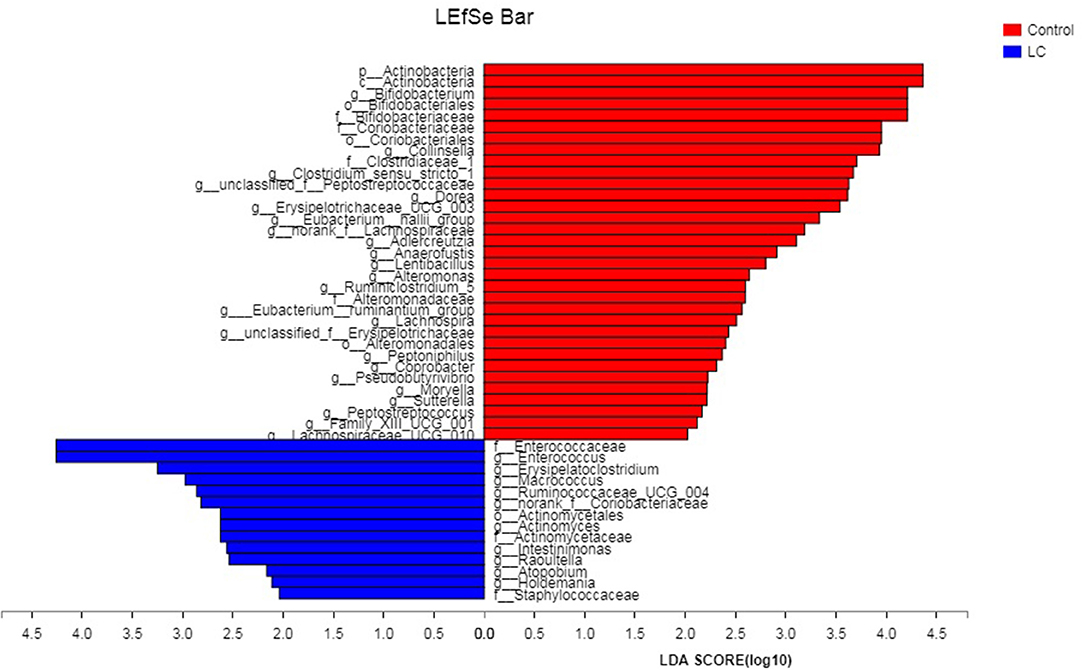
Figure 3. The LDA score obtained by linear regression analysis (LDA), the larger the LDA score, the greater the influence of species abundance on the difference effect. LC, lung cancer.
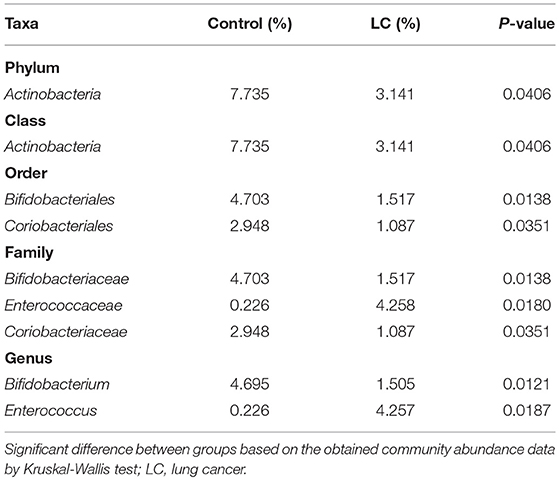
Table 2. Taxa differentially represented in the gut microbiomes of LC patients and healthy controls.
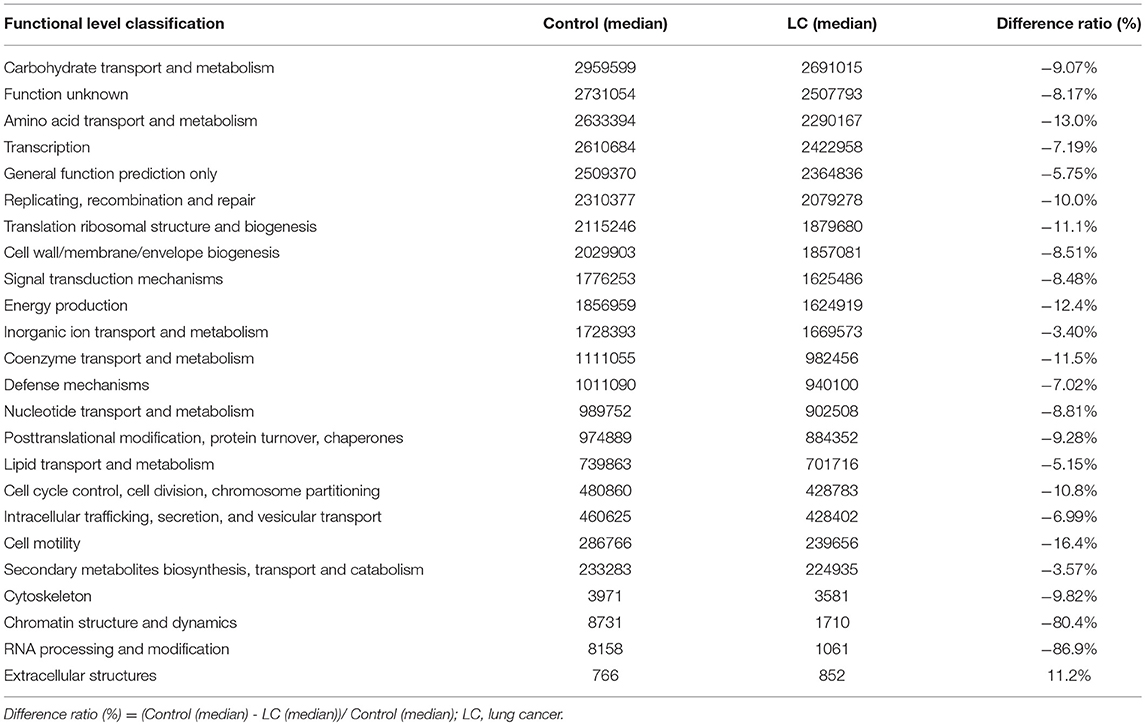
Differential Microbiome Functional Abundance Spectrum in the Lung Cancer Group
We implemented a 16S functional predictive analysis by COG (Cluster of Ortholog Genes) functional annotation, where the description information of each COG and its functional information was parsed from the eggNOG database. Compared to the healthy controls, results showed a significant decline in the functional abundance spectrum including 24 gut microbiota metabolic pathways in LC patients (Table 3). Among them, the expression of functional proteins involved in chromatin structure and dynamics and RNA processing and modification both decreased by more than 80%. At the same time, the only up-regulated was the extracellular structures related metabolic functions, which rose more than 10% in protein expression level (Table 3). The legends are shown in Figure S4.
Discussion
In this study, we found that patients with LC had no difference in gut microbial alpha diversity but showed significant differences in microbial composition compared to healthy controls (Figures 1, 2; Table 2). At the phylum level, we found that these differences were mainly caused by Actinobacteria (Table 2). At the genus level, Bifidobacterium and Enterococcus were found to be the highest potential biomarkers for lung carcinogenesis (Table 2). We also observed a differential microbiome function abundance by 16S function prediction between these two groups (Table 3, Figure S4).
These results are consistent with the growing body of evidence for a bidirectional relationship between the gut microbiome and malignancies (Eun et al., 2014; Flemer et al., 2017; Allali et al., 2018). Meanwhile, human studies have concluded that the metabolic processes and products of the gut microbiome regulate human health and disease, including the development of immune function, incidence of obesity or anorexia nervosa, various types of cancer (Kluyver, 1932; Belcheva et al., 2015; Takiishi et al., 2017; Zhou and Fang, 2018). At the level of the phylum, we found drastically reduced Actinobacteria sp. as a possible LC-associated biomarker. This phylum contains a large proportion of commensal species, which are part of the healthy human microflora (Kundu et al., 2017). Although our method does not allow the identification of specific species within Actinobacteria, the abundance reduction in this phylum may be involved in the pathogenesis of LC. If there is a causal role in LC, then cancer suppression of malignant cells by secondary metabolites of the gut actinomycetes might be of interest (Rangan and Hang, 2017). A study has recently obtained initial evidence to support this hypothesis: an isolated Actinobacteria sp. from healthy children had potent cancer-suppressing activities due to its secondary metabolites (Zhou et al., 2017). Ravikumar et al. found anticancer properties of sediment actinomycetes against MCF-7 and MDA-MB-231 cell lines (Ravikumar et al., 2012). Thus, anticancer compounds produced by specific Actinobacteria sp. had a direct killing effect on malignant cells, which might explain the observed overrepresentation of this genus in healthy samples. The LEfSe analysis and difference significance test both showed that the genus Bifidobacterium was significantly more abundant in controls, while the LC patients showed elevated levels of Enterococcus. Members of Bifidobacterium have a variety of probiotic functions, such as improving inflammatory bowel disease, ulcerative colitis, Crohn's disease, and colonic pouchitis (van den Broek et al., 2008; Wang et al., 2014; Klemenak et al., 2015; Liang et al., 2018). At the same time, Bifidobacterium can inhibit the growth of spoilage bacteria and decompose carcinogens to achieve anti-cancer effects and reduce the inflammation caused by TNF-α and lipopolysaccharide (Boesten et al., 2011; Klemenak et al., 2015; Lim and Kim, 2017). Recently, researchers such as Shang et al. have confirmed that TNF-α promotes metastasis of lung cancer by inducing epithelial–mesenchymal transition (Shang et al., 2017). If there is a causal relationship, the decrease in genus Bifidobacterium we find in LC patients may reflect the bacterial community involved in a progression of lung cancer. However, compared with Bifidobacterium, Enterococcus can produce many harmful chemicals that lead to increased DNA mismatch rate, which, in turn, causes genetic activity that promotes rectal cancer (Strickertsson et al., 2013; Amarnani and Rapose, 2017). In previous studies, Enterococcus faecalis infections have been confirmed to lead to NF-κB inflammatory responses and DNA damage. At the same time, the superoxide secreted by Enterococcus spp. sent a strong signal to macrophages, changed the growth and division of intestinal parasitic cells, and enhanced the activity of oncogenes (Strickertsson et al., 2013; Wang et al., 2015; Amarnani and Rapose, 2017). Although the underlying mechanisms of an inflammatory response-associated severity of lung carcinogenesis are not understood, the overrepresentation of Enterococcus has been suspected as being a missing link.
Using the 16s functional predictive analysis, significant differences in microbiome functional abundance between the two groups were observed. The healthy controls had a significantly higher microbiome functional spectrum, while the LC patients showed elevated levels only in expression of extracellular structures functional proteins. The various metabolic abilities of the gut microbiome are being reduced during the disease (Table 3). In the gut micro-ecology of LC patients, expressions of functional proteins involved in amino acid transport and metabolism, coenzyme transport and metabolism, cell cycle control, and cell division all decreased by more than 10%, which directly negatively impacted the reproduction of, and colonization by, gut bacteria. The gut microbiome is not only an important participant in the digestive function of the human body, but also plays a substantial role in maintaining the gut—the largest immune organ (Kau et al., 2011; Hwang et al., 2012; Zitvogel et al., 2017). A team led by Dr. Laurence Zitvogel of the Gustave Roussy Cancer Center showed that some cancer treatments rely on the gut microbiota to activate the immune system (Gopalakrishnan et al., 2018; Zitvogel et al., 2018). A large body of evidence confirms that the host and the enteric microbiome complement each other, and the disorder of the gut microecology is exacerbated during the disease state, which greatly impairs its beneficial functions (Kelly et al., 2015; Ringel, 2017). Undoubtedly, changes in microbial-associated molecular patterns and microbiome functions caused by bacterial dysbiosis are key pathways for the progression of LC.
The importance of the human gut microbiome is being increasingly recognized. As an important “organ” that has long been neglected, how to maintain a healthy gut microbiome is increasingly becoming a focus. However, due to the limitations in technical conditions and a lack of sufficient clinical data, the specific mechanisms of microbial-associated molecular patterns and bacterial metabolites driving cancer have not been fully elucidated. In the future, we will review in detail therapeutic modalities and discuss clinical settings in which targeting the “gut-microbiota–lung axis” for the prevention of LC seems promising. In addition, since the main research object of gut microbial diversity analysis is gut bacteria, the whole process of the experiment was carried out using bacterial universal primers for the amplification of bacterial marker genes, the virus and mycoplasma present in a small part were not analyzed. It is necessary to design a completion plan for this limitation in the future study.
In conclusion, compared to previous analyses of the relationship between LC and the lung microbiome, this is the first study of LC in connection with the gut microbiome (Hosgood et al., 2014; Kosikowska et al., 2016). Our findings support the hypothesis of LC-specific microbiota. We suggest that the reduced levels of Actinobacteria sp. and Bifidobacterium sp. and elevated levels of Enterococcus sp. are associated with LC. At the same time, we have further revealed that the damage of the normal function of the gut microbiome is associated with the progression of LC. the progress of LC. We hope that the results herein can provide some guidance for using gut microbes as biomarkers to assess the progression of lung cancer, or lead to interventional targets to control the development of the disease.
Ethics Statement
Fecal samples were collected in this research without any medical expense or suffering by the subjects, and the results were used for scientific research purposes. We declare that none of the authors have any conflicts of interest or financial ties to disclose. This study was carried out in accordance with the recommendations of Ethical Guidelines for Biomedical Research, Harbin Medical University Ethics Review Committee (an affiliated department of Harbin Medical University). The protocol was approved by the Harbin Medical University Ethics Review Committee. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The subjects' rights were adequately protected, and there was no potential risk to the subjects.
Author Contributions
HZ, YW, LC, and Y-KZ are responsible for sequencing, article writing. M-FZ, G-DL, M-CZ, Y-GL, J-BZ, and Y-NG are responsible for the collection and processing of clinical samples. Y-JZ and S-LL are responsible for the experimental design.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank LetPub (https://www.letpub.com.cn/) for its linguistic assistance during the preparation of this manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcimb.2019.00112/full#supplementary-material
Figure S1. The abscissa is the amount of sequencing data randomly selected; the ordinate is the number of species observed.
Figure S2. Points of blue colors or shapes represent LC samples; red colors or shapes represent samples of control. The closer the two sample points are, the more similar the composition of the two sample species is. The horizontal and vertical coordinates represent relative distances and have no practical significance. It is generally considered that stress <0.2 can be expressed by the two-dimensional dot pattern of NMDS, and its graph has a certain explanatory meaning. LC, lung cancer.
Figure S3. The axis represents the taxa name at a given classification level, and the column length corresponding to the species indicates the average relative abundance of the species in each sample group. The different colors indicate different groupings. The rightmost side is the P-value from Kruskal–Wallis test, * 0.01 < P ≤ 0.05, ** 0.001 < P ≤ 0.01, *** P ≤ 0.001. LC, lung cancer.
Figure S4. The abscissa is the first-level classification of COG function. LC, lung cancer.
References
Addario, B. J. (2014). Larger studies of multiple families will help us better understand inherited risk of lung cancer. J. Thorac. Oncol. 9, e65–66. doi: 10.1097/JTO.0000000000000223
Allali, I., Boukhatem, N., Bouguenouch, L., Hardi, H., Boudouaya, H. A., Cadenas, M. B., et al. (2018). Gut microbiome of moroccan colorectal cancer patients. Med. Microbiol. Immunol. 207, 211–225. doi: 10.1007/s00430-018-0542-5
Allison, J. P. (2015). Immune checkpoint blockade in cancer therapy: the 2015 lasker-debakey clinical medical research award. J. Am. Med. Assoc. 314, 1113–1114. doi: 10.1001/jama.2015.11929
Amarnani, R., and Rapose, A. (2017). Colon cancer and enterococcus bacteremia co-affection: a dangerous alliance. J. Infect. Public. Health. 10, 681–684. doi: 10.1016/j.jiph.2016.09.009
Belcheva, A., Irrazabal, T., and Martin, A. (2015). Gut microbial metabolism and colon cancer: can manipulations of the microbiota be useful in the management of gastrointestinal health? Bioessays 37, 403–412. doi: 10.1002/bies.201400204
Boesten, R. J., Schuren, F. H., Willemsen, L. E., Vriesema, A., Knol, J., and De Vos, W. M. (2011). Bifidobacterium breve - HT-29 cell line interaction: modulation of TNF-alpha induced gene expression. Benef. Microbes 2, 115–128. doi: 10.3920/BM2011.0005
Boleij, A., van Gelder, M. M., Swinkels, D. W., and Tjalsma, H. (2011). Clinical Importance of Streptococcus gallolyticus infection among colorectal cancer patients: systematic review and meta-analysis. Clin. Infect. Dis. 53, 870–878. doi: 10.1093/cid/cir609
Chowdhury, P. S., Chamoto, K., and Honjo, T. (2018). Combination therapy strategies for improving PD-1 blockade efficacy: a new era in cancer immunotherapy. J. Intern. Med. 283, 110–120. doi: 10.1111/joim.12708
Cuevas-Ramos, G., Petit, C. R., Marcq, I., Boury, M., Oswald, E., and Nougayrède, J. P. (2010). Escherichia coli induces DNA damage in vivo and triggers genomic instability in mammalian cells. Proc. Natl. Acad. Sci. U. S. A. 107, 11537–11542. doi: 10.1073/pnas.1001261107
Douglas, G. M., Beiko, R. G., and Langille, M. G. I. (2018). Predicting the functional potential of the microbiome from marker genes using PICRUSt. Methods Mol. Biol. 1849, 169–177. doi: 10.1007/978-1-4939-8728-3_11
Eun, C. S., Kim, B. K., Han, D. S., Kim, S. Y., Kim, K. M., Choi, B. Y., et al. (2014). Differences in gastric mucosal microbiota profiling in patients with chronic gastritis, intestinal metaplasia, and gastric cancer using pyrosequencing methods. Helicobacter 19, 407–416. doi: 10.1111/hel.12145
Flemer, B., Lynch, D. B., Brown, J. M., Jeffery, I. B., Ryan, F. J., Claesson, M. J., et al. (2017). Tumour-associated and non-tumour-associated microbiota in colorectal cancer. Gut 66, 633–643. doi: 10.1136/gutjnl-2015-309595
Gagliani, N., Palm, N. W., de Zoete, M. R., and Flavell, R. A. (2014). Inflammasomes and intestinal homeostasis: regulating and connecting infection, inflammation and the microbiota. Int. Immunol. 26, 495–499. doi: 10.1093/intimm/dxu066
Gibbons, D. L., Byers, L. A., and Kurie, J. M. (2014). Smoking, p53 mutation, and lung cancer. Mol. Cancer Res. 12, 3–13. doi: 10.1158/1541-7786.MCR-13-0539
Gopalakrishnan, V., Spencer, C. N., Nezi, L., Reuben, A., Andrews, M. C., Karpinets, T. V., et al. (2018). Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 359, 97–103. doi: 10.1126/science.aan4236
Hendriks, L., and Besse, B. (2018). New windows open for immunotherapy in lung cancer. Nature 558, 376–377. doi: 10.1038/d41586-018-05312-9
Herbst, R. S., Morgensztern, D., and Boshoff, C. (2018). The biology and management of non-small cell lung cancer. Nature 553, 446–454. doi: 10.1038/nature25183
Hosgood, H. D., Sapkota, A. R., Rothman, N., Rohan, T., Hu, W., Xu, J., et al. (2014). The potential role of lung microbiota in lung cancer attributed to household coal burning exposures. Environ. Mol. Mutagen. 55, 643–651. doi: 10.1002/em.21878
Huerta-Cepas, J., Szklarczyk, D., Forslund, K., Cook, H., Heller, D., Walter, M. C., et al. (2016). eggNOG 4.5: a hierarchical orthology framework with improved functional annotations for eukaryotic, prokaryotic and viral sequences. Nucleic Acids Res. 44, D286–293. doi: 10.1093/nar/gkv1248
Hwang, J. S., Im, C. R., and Im, S. H. (2012). Immune disorders and its correlation with gut microbiome. Immune Netw. 12, 129–138. doi: 10.4110/in.2012.12.4.129
Jobin, C. (2012). Colorectal cancer: CRC–all about microbial products and barrier function? Nat Rev. Gastroenterol. Hepatol. 9, 694–696. doi: 10.1038/nrgastro.2012.220
Kau, A. L., Ahern, P. P., Griffin, N. W., Goodman, A. L., and Gordon, J. I. (2011). Human nutrition, the gut microbiome and the immune system. Nature 474, 327–336. doi: 10.1038/nature10213
Kelly, J. R., Kennedy, P. J., Cryan, J. F., Dinan, T. G., Clarke, G., and Hyland, N. P. (2015). Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front. Cell. Neurosci. 9:392. doi: 10.3389/fncel.2015.00392
Klemenak, M., Dolinšek, J., Langerholc, T., Di Gioia, D., and Mičetić-Turk, D. (2015). Administration of bifidobacterium breve decreases the production of TNF-alpha in children with celiac disease. Dig. Dis. Sci. 60, 3386–3392. doi: 10.1007/s10620-015-3769-7
Kluyver, A. J. (1932). Microbial metabolism and its bearing on the cancer problem. Science 76, 527–532. doi: 10.1126/science.76.1980.527
Kosikowska, U., Biernasiuk, A., Rybojad, P., Los, R., and Malm, A. (2016). Haemophilus parainfluenzae as a marker of the upper respiratory tract microbiota changes under the influence of preoperative prophylaxis with or without postoperative treatment in patients with lung cancer. BMC Microbiol. 16:62. doi: 10.1186/s12866-016-0679-6
Kundu, P., Blacher, E., Elinav, E., and Pettersson, S. (2017). Our gut microbiome: the evolving inner self. Cell. 171, 1481–1493. doi: 10.1016/j.cell.2017.11.024
Liang, Y., Lin, C., Zhang, Y., Deng, Y., Liu, C., and Yang, Q. (2018). Probiotic mixture of Lactobacillus and Bifidobacterium alleviates systemic adiposity and inflammation in non-alcoholic fatty liver disease rats through Gpr109a and the commensal metabolite butyrate. Inflammopharmacology 26, 1051–1055. doi: 10.1007/s10787-018-0479-8
Lim, S. M., and Kim, D. H. (2017). Bifidobacterium adolescentis IM38 ameliorates high-fat diet-induced colitis in mice by inhibiting NF-kappaB activation and lipopolysaccharide production by gut microbiota. Nutr. Res. 41, 86–96. doi: 10.1016/j.nutres.2017.04.003
Lissanu Deribe, Y., Sun, Y., Terranova, C., Khan, F., Martinez-Ledesma, J., et al. (2018). Mutations in the SWI/SNF complex induce a targetable dependence on oxidative phosphorylation in lung cancer. Nat. Med. 24, 1047–1057. doi: 10.1038/s41591-018-0019-5
Liu, X., Lin, X. J., Wang, C. P., Yan, K. K., Zhao, L. Y., An, W. X., et al. (2014). Association between smoking and p53 mutation in lung cancer: a meta-analysis. Clin. Oncol. 26, 18–24. doi: 10.1016/j.clon.2013.09.003
Nakatsu, G., Li, X., Zhou, H., Sheng, J., Wong, S. H., Wu, W. K., et al. (2015). Gut mucosal microbiome across stages of colorectal carcinogenesis. Nat. Commun. 6:8727. doi: 10.1038/ncomms9727
Neish, A. S. (2009). Microbes in gastrointestinal health and disease. Gastroenterology 136, 65–80. doi: 10.1053/j.gastro.2008.10.080
Noval Rivas, M., Burton, O. T., Wise, P., Zhang, Y. Q., Hobson, S. A., Garcia Lloret, M., et al. (2013). A microbiota signature associated with experimental food allergy promotes allergic sensitization and anaphylaxis. J. Allerg. Clin. Immunol. 131, 201–212. doi: 10.1016/j.jaci.2012.10.026
Puri, P., Liangpunsakul, S., Christensen, J. E., Shah, V. H., Kamath, P. S., Gores, G. J.Puri, P., Liangpunsakul, S., Christensen, J. E., Shah, V. H., et al. (2018). The circulating microbiome signature and inferred functional metagenomics in alcoholic Hepatitis 67, 1284–1302. doi: 10.1002/hep.29623
Rangan, K. J., and Hang, H. C. (2017). Biochemical Mechanisms of Pathogen Restriction by Intestinal Bacteria. Trends Biochem. Sci. 42, 887–898. doi: 10.1016/j.tibs.2017.08.005
Ravi, R. K., Walton, K., and Khosroheidari, M. (2018). MiSeq, a next generation sequencing platform for genomic analysis. Methods Mol. Biol. 1706, 223–232. doi: 10.1007/978-1-4939-7471-9_12
Ravikumar, S., Fredimoses, M., and Gnanadesigan, M. (2012). Anticancer property of sediment actinomycetes against MCF-7 and MDA-MB-231 cell lines. Asian. Pac. J. Trop. Biomed. 2, 92–96. doi: 10.1016/S2221-1691(11)60199-8
Ringel, Y. (2017). the gut microbiome in irritable bowel syndrome and other functional bowel disorders. Gastroenterol. Clin. North. Am. 46, 91–101. doi: 10.1016/j.gtc.2016.09.014
Schwabe, R. F., and Jobin, C. (2013). The microbiome and cancer. Nat. Rev. Cancer 13, 800–812. doi: 10.1038/nrc3610
Shang, G. S., Liu, L., and Qin, Y. W. (2017). IL-6 and TNF-alpha promote metastasis of lung cancer by inducing epithelial-mesenchymal transition. Oncol. Lett. 13, 4657–4660. doi: 10.3892/ol.2017.6048
Strickertsson, J. A., Desler, C., Martin-Bertelsen, T., Machado, A. M., Wadstrøm, T., Winther, O., et al. (2013). Enterococcus faecalis infection causes inflammation, intracellular oxphos-independent ROS production, and DNA damage in human gastric cancer cells. PLoS ONE 8:e63147. doi: 10.1371/journal.pone.0063147
Takiishi, T., Fenero, C. I. M., and Câmara, N. O. S. (2017). Intestinal barrier and gut microbiota: Shaping our immune responses throughout life. Tissue Barriers. 5:e1373208. doi: 10.1080/21688370.2017.1373208
Toprak, N. U., Yagci, A., Gulluoglu, B. M., Akin, M. L., Demirkalem, P., Celenk, T., et al. (2006). A possible role of Bacteroides fragilis enterotoxin in the aetiology of colorectal cancer. Clin. Microbiol. Infect. 12, 782–786. doi: 10.1111/j.1469-0691.2006.01494.x
Torre, L. A., Bray, F., Siegel, R. L., Ferlay, J., Lortet-Tieulent, J., and Jemal, A. (2015). Global cancer statistics, 2012. CA Cancer. J. Clin. 65, 87–108. doi: 10.3322/caac.21262
Tsay, J. J., Wu, B. G., Badri, M. H., Clemente, J. C., Shen, N., Meyn, P., et al. (2018). Airway microbiota is associated with upregulation of the PI3K pathway in lung Cancer. 198, 1188–1198. doi: 10.1164/rccm.201710-2118OC
van den Broek, L. A., Hinz, S. W., Beldman, G., Vincken, J. P., and Voragen, A. G. (2008). Bifidobacterium carbohydrases-their role in breakdown and synthesis of (potential) prebiotics. Mol. Nutr. Food. Res. 52, 146–163. doi: 10.1002/mnfr.200700121
Verma, A., and Shukla, G. (2013). Probiotics Lactobacillus rhamnosus GG, Lactobacillus acidophilus suppresses DMH-induced procarcinogenic fecal enzymes and preneoplastic aberrant crypt foci in early colon carcinogenesis in Sprague Dawley rats. Nutr. Cancer 65, 84–91. doi: 10.1080/01635581.2013.741746
Wang, S., Liu, K., Seneviratne, C. J., Li, X., Cheung, G. S., Jin, L., et al. (2015). Lipoteichoic acid from an Enterococcus faecalis clinical strain promotes TNF-alpha expression through the NF-kappaB and p38 MAPK signaling pathways in differentiated THP-1 macrophages. Biomed. Rep. 3, 697–702. doi: 10.3892/br.2015.495
Wang, T., Cai, G., Qiu, Y., Fei, N., Zhang, M., Pang, X., et al. (2012). Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. ISME J. 6, 320–329. doi: 10.1038/ismej.2011.109
Wang, W., Chen, L., Zhou, R., Wang, X., Song, L., Huang, S., et al. (2014). Increased proportions of Bifidobacterium and the Lactobacillus group and loss of butyrate-producing bacteria in inflammatory bowel disease. J. Clin. Microbiol. 52, 398–406. doi: 10.1128/JCM.01500-13
Wei, S. C., Duffy, C. R., and Allison, J. P. (2018). Fundamental mechanisms of immune checkpoint blockade therapy. Cancer Discov. 8, 1069–1086. doi: 10.1158/2159-8290.CD-18-0367
Wu, S., Rhee, K. J., Albesiano, E., Rabizadeh, S., Wu, X., Yen, H. R., et al. (2009). A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat. Med. 15, 1016–1022. doi: 10.1038/nm.2015
Zhou, C. B., and Fang, J. Y. (2018). The regulation of host cellular and gut microbial metabolism in the development and prevention of colorectal cancer. Crit. Rev. Microbiol. 44, 436–454. doi: 10.1080/1040841X.2018.1425671
Zhou, Y. J., Zhao, D. D., Liu, H., Chen, H. T., Li, J. J., Mu, X. Q., et al. (2017). Cancer killers in the human gut microbiota: diverse phylogeny and broad spectra. Oncotarget 8, 49574–49591. doi: 10.18632/oncotarget.17319
Zitvogel, L., Daillère, R., Roberti, M. P., Routy, B., and Kroemer, G. (2017). Anticancer effects of the microbiome and its products. Nat. Rev. Microbiol. 15, 465–478. doi: 10.1038/nrmicro.2017.44
Keywords: lung cancer, gut microbiota, next generation sequencing, 16S rRNA, microbial diversity, biomarkers
Citation: Zhuang H, Cheng L, Wang Y, Zhang Y-K, Zhao M-F, Liang G-D, Zhang M-C, Li Y-G, Zhao J-B, Gao Y-N, Zhou Y-J and Liu S-L (2019) Dysbiosis of the Gut Microbiome in Lung Cancer. Front. Cell. Infect. Microbiol. 9:112. doi: 10.3389/fcimb.2019.00112
Received: 20 December 2018; Accepted: 01 April 2019;
Published: 18 April 2019.
Edited by:
Yongqun He, University of Michigan Health System, United StatesReviewed by:
Nagendra Singh, Medical College of Georgia, Augusta University, United StatesCésar López-Camarillo, Universidad Autónoma de la Ciudad de México, Mexico
Copyright © 2019 Zhuang, Cheng, Wang, Zhang, Zhao, Liang, Zhang, Li, Zhao, Gao, Zhou and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shu-Lin Liu, c2xsaXVAaHJibXUuZWR1LmNu
Yu-Jie Zhou, eWp6aG91QGNjbXUuZWR1LmNu
Yi-Na Gao, Z2FveWluYV9ITVVAMTYzLmNvbQ==
†These authors have contributed equally to this work
‡Present Address: Yu-Jie Zhou, Department of Immunology, Capital Medical University, Beijing, China
 He Zhuang
He Zhuang Liang Cheng1,4†
Liang Cheng1,4† Yu-Jie Zhou
Yu-Jie Zhou Shu-Lin Liu
Shu-Lin Liu