Sustainable financing of AYSRH programs by local governments through the TCI model
- 1The Challenge Initiative Project, Jhpiego Kenya Country Office, Nairobi, Kenya
- 2Department of Health, County Government of Kilifi, Kilifi, Kenya
- 3Department of Health, County Government of Migori, Migori, Kenya
- 4The Challenge Initiative Project, Jhpiego Uganda Country Office, Kampala, Uganda
Introduction: Despite the existence of a legal policy framework, financing of adolescent and youth sexual and reproductive health (AYSRH) services has remained weak. External donors are the main financing agents, which has implications for the sustainability of service provision. International development partners have reduced funding for health programs from historically high levels. In Kenya, the health sector's budget allocation has remained below the 15% committed to under the Abuja declaration. With Kenya's devolved government structure, a greater proportion of financial resources are dedicated towards recurrent and structural expenses as opposed to addressing health systems gaps.
Objectives: The purpose of this manuscript is to assess the contribution of The Challenge Initiative (TCI) Business Unusual model on AYSRH services in the counties of Kilifi and Migori, as well as to examine the institutionalization of high impact interventions (HIIs) within the annual work plan, budget, and systems of the said counties. Additionally, this study aims to analyse the trend in contraceptive uptake among adolescent and young women aged 15 to 24 in Kilifi and Migori counties.
Methods: Migori and Kilifi Counties chose to partner with TCI to implement the Business Unusual model. Interested counties apply for the initiative's support and commit to contributing a portion of the funding needed to adapt and implement high impact interventions (HIIs). Based on the identified gaps, TCI supported the counties to prioritize the HIIs including integrated outreaches, youth fixed days, whole site orientation, youth champions, and youth dialogues. The program was implemented between July 2018 to June 2021 in 60 and 68 public health facilities of Kilifi and Migori Counties, respectively. The county teams identified and selected program implementation team whose key role was to coordinate, review, monitor, mobilize resources and report AYSRH program implementation progress.
Results: The results showed a 60% increase in financial commitments on AYSRH programming from 2018 to 2021 in both counties. The average expenditure for committed funds for Kilifi and Migori Counties was 116% and 41% respectively. As the counties continued to allocate and spend funds on the implementation of HIIs, there was a noticeable increase in contraceptive uptake among the young people aged 15 to 24 who visited health facilities for services. There was a 59% and 28% percentage increase in contraceptive uptake among young people (15–24 years) between 2018 and 2021. The proportion of adolescents amongst those presenting for first ANC clinic dropped from 29.4% in 2017 to 9% in 2021 in Kilifi County and from 32.2% in 2017 to 14% in 2021 in Migori County. Using the TCI's Sisi kwa Sisi coaching model of lead-assist-observe-monitor, 20 master coaches were trained. The master coaches cascaded the training to over 97 coaches. The coaches will continue to build capacity of peers in advocacy for resource mobilization and implementation of HIIs. At least nine of TCI's HIIs have been adopted in Kilifi and Migori County strategies and annual work plans, and there is financial support for their sustainability.
Discussion: The increase in adolescent contraceptive uptake might have been as a result of the system strengthening through self-financing of AYSRH programs, the institutionalization of HIIs, and the coaching. Local governments can invest in and sustain their own AYSRH programs, which will lead to an improvement in adolescent and youth access to contraceptive services and, as a result, a reduction in adolescent pregnancies, maternal mortality, and infant mortality.
Introduction
In the recent past, adolescent youth sexual reproductive health (AYSRH) needs have become a growing concern worldwide. The high number of adolescent pregnancies is attributed to inadequate access to sexual reproductive health services. This has exacerbated the vulnerability of adolescent young girls to poverty, exclusion, and exploitation (1). Adolescent pregnancy is a major health and social concern due to its association with high maternal and child morbidity and mortality (1, 2). In Kenya, 47% of young women aged 18–24 years reported sexual debut before the age of 18 years, with a teen pregnancy rate of 18% (3).
Kilifi and Migori counties are among the counties recording high rates of adolescent pregnancies in Kenya. In 2018, the proportion of adolescent pregnancy (10–19 years) among women attending first antenatal clinic (ANC) in Kilifi and Migori stood at 29.4% and 32.2% respectively, much higher than national level (4).
The high adolescent pregnancy is attributed to low contraceptive utilization among sexually active adolescents. According to Saifuddin et.al 2019, family planning programs have contributed to an increase in the contraceptive prevalence rate globally (5). Increasing use of contraceptive methods will not only result in improvements in health-related outcomes such as reduced adolescent pregnancy, reduced maternal and infant mortality, but creates an opportunity for women and girls to advance in their education and careers while improving their economic outcomes (6, 7).
During the 2019 International Conference on Population and Development (ICPD), governments agreed to enhance access to comprehensive AYSRH services and responsive information and education for all adolescents and youth (8). This will enable them to make informed decisions and choices about their sexuality and reproductive lives, to adequately protect themselves from unintended pregnancies.
Resource allocation and utilization towards AYSRH interventions enhances program improvement and sustainability. Kenya is a signatory of the Abuja Declaration, which pledges to increase African governments' spending for health to at least 15% of the total budget (9), but this commitment remains to be met (10). According to Korir et al., international NGOs and foundations have been the main financing agents in the provision of family planning (FP) services in the country and it is not sustainable (11). Continuous advocacy efforts play a key role towards funds allocation and utilization for sustained implementation of AYSRH interventions. According to Starrs et al. 2018, to sustain the gains in AYSRH service provision and reduction in adolescent pregnancies, health systems need sustainable and predictable financing. County governments must make essential sexual and reproductive health services a priority and ensure they are included in health budgets. Provision of resources towards AYSRH is critical to ensure increased uptake of contraceptives among adolescents and reduction of adolescent pregnancies (12).
Although donor assistance for AYSRH Programs in Kenya has increased over the years, the percentage of government funds devoted to AYSRH program is still low (13), and Kilifi and Migori counties are not exceptional. With devolved government structures in Kenya, counties have assumed a greater role and responsibility including allocation and expenditure of funds in the implementation of AYSRH programming. Nonetheless, a greater proportion of the financial resources are usually dedicated towards human resources, operations, and maintenance as opposed to addressing health systems and service delivery gaps (14).
The Challenge Initiative (TCI) has been working in collaboration with the county Government and other implementing partners in Kilifi and Migori counties to implement select global best practices in AYSRH under the Business Unusual Model. The Business Unusual Model helps in prioritization of finance, scale-up, and sustainability of high-impact solutions for family planning and AYSRH. The select best practices are referred to as high impact interventions (HIIs). This approach is a shift in strategy from the traditional development model, in that it is demand-driven, allowing counties to self-select, as well as determine FP and AYSRH HIIs to implement based on existing gaps. This concept has cultivated a mind-set shift towards resource allocation, increased ownership, and sustainability of AYSRH of programs. The TCI program is currently being implemented by city governments in 11 countries in Africa and Asia.
This paper aims to share experiences on how the TCI Business Unusual Model has contributed to the success of the AYSRH program in Kilifi and Migori counties leading to increased uptake of contraceptives and reduced adolescent pregnancies. Specifically, we present the contribution of TCI Business Unusual Model on the improvement of AYSRH program sustainability; and document trends in contraceptive uptake among adolescent and young women aged 15- 24; and adolescent pregnancy among 15–19-year-olds in Kilifi and Migori during the implementation period.
Methods
Program description
In 2010, the Bill & Melinda Gates Foundation launched the Urban Reproductive Health Initiative (URHI) to identify solutions to address the FP needs of the urban poor. The URHI demonstrated the effectiveness of a range of supply- and demand-side interventions in improving the accessibility, quality, and use of FP services. To catalyse the rapid adoption and scale-up of these high-impact interventions (HIIs), the foundation created TCI. Launched in 2017, TCI deploys a “business unusual” model, whereby interested local governments apply for the initiative's support and commit to contributing a portion of the funding needed to adapt and implement HIIs in their geographies. A diverse range of HIIs available to local governments include interventions to improve management of FP programming, support advocacy to increase funding for FP, improve service delivery, and generate demand. Starting in 2018, local governments could also elect to “layer” on programming to support adolescent and youth sexual and reproductive health (AYSRH). To effectively implement these interventions, local governments received a range of support, collectively called TCI-University. These include:
• Toolkits with detailed protocols, job aids and manuals to guide implementation of the HIIs;
• Coaching to build the managerial and technical capacity of local government officials, service providers, community health workers (CHWs), and other community actors;
• Access to a community of practice (CoP) to share learnings and experiences.
Study setting
Migori and Kilifi Counties, located in Kenya, are among the counties that chose to partner with TCI to implement the Business Unusual model. TCI supported the counties to prioritize the HIIs based on their existing gaps. The selected HIIs included; integrated outreaches, youth fixed days, whole site orientation, youth champions, intergenerational youth dialogues and digital/media platforms. The program was implemented between July 2018 to June 2021 in 60 and 68 public health facilities of Kilifi and Migori counties, respectively. The county teams identified and selected key program implementers, referred to as program implementation team (PIT) whose key role was to coordinate, review, monitor and report AYSRH program implementation progress. The PIT also played a role in advocacy for resource mobilization, allocation, and utilization for AYSRH Programming.
Indicators
The various indicators of program progress were regularly monitored using data from the following information systems:
• Kenya Health Information System (KHIS): used to track contraceptive uptake service data among adolescents aged 15–19 and 20–24 years from all health facilities reporting into KHIS. This system also captured antenatal care (ANC) attendance from those presenting with pregnancy at first ANC visit at facility aged 15–19 years in Kilifi and Migori counties. This data was used to calculate the total number of adolescents pregnant in a given financial year.
• Program progress reports: these tracked program outputs, financial expenditure and system strengthening qualitative data. Financial data was reviewed from existing documents like annual work plans and financial commitments made by Kilifi and Migori counties for the financial year 2017 to 2021. Financial expenditure on AYSRH was tracked and reviewed against the county budgets, compared before and after intervention.
• Most Significant Change (MSC) technique was used to capture voices of the implementers, stakeholders and community members about the impacts of the AYSRH program on their lives and communities. MSC stories were also collected from targeted key decision makers at the county level and healthcare providers.
Results
Funds allocation and expenditure
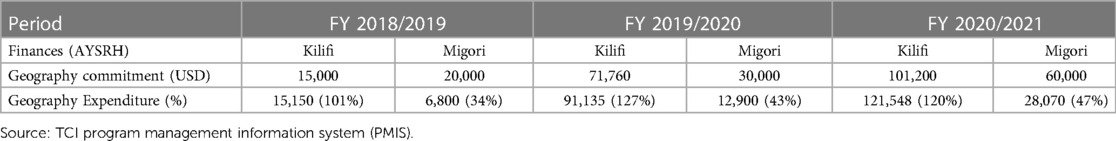
Over the years of program implementation there were increases in financial commitments and expenditure on AYSRH Program in both Kilifi and Migori Counties. Kilifi County spent more than they had initially committed which demonstrates the County's commitment to addressing adolescent health matters (see Table 1 below).
Health systems strengthening
Capacity transfer
TCI trained 20 master coaches who cascaded the training to over 97 coaches in Kilifi and Migori to ensure provision and implementation of AYSRH HIIs. The five-day standardized training curriculum broadly entailed preparing master coaches at county level to spearhead the implementation of the AYSRH program, applying transformative leadership and coordination to implement the AYSRH program, how to adapt and implement HIIs using the TCI—University toolkit, managing resources effectively and utilizing data for AYSRH program monitoring and decision making.
Some of the interventions targeting adolescents implemented included 700 AYSRH whole site orientation sessions—an approach to provide basic AYSRH knowledge to all staff (clinical & non-clinical) working in the health facility, 209 integrated youth outreaches—a health service delivery activity done outside the health facility aimed at bringing services closer to the youths, 184 youth dialogue days—a dialogue forum that bring young people together to discuss their needs and challenges, training 145 youth champions—young people who advocate for AYSRH services- trained on AYSRH, and 15 advocacy meetings in both Kilifi and Migori supporting increased expenditure and commitments for the next financial years.
Institutionalization of the HIIs
The MSC stories collected demonstrated that HIIs and processes, including the establishment of AYSRH coordinators, have been institutionalized in Kilifi and Migori County health systems, budgets and annual work plans, and there is support for their scalability. Here are quotes from select key county leadership and health management teams.
“The TCI’s business model came in at the right time, and as a county, we had to adopt and adapt the interventions to start the journey in reducing our negative indicators in AY. (Adolescent and Youth)”
Political leader- Kilifi County.
“When TCI introduced the adolescent and youth program we knew we had to be part of it…. We did not even have a policy as a county to guide us on how to implement AY programs. One of the indicators to be addressed was contraceptive uptake among adolescents……, we focused on interventions that would also reach the youth. We had a starting point in that we picked interventions that had worked.”
County Health Department representative—Kilifi County.
“The establishment of the County AYSRH Coordinators’ position ensured that the program gets a differentiated share of budget allocation from the main Reproductive Maternal Newborn Child and Adolescent Health (RMNCAH) budget, it was given space in the annual work plan as a subprogram within RMNCAH. The Co-ordinator was tasked with consolidating all the partners together hence establishment of AYSRH Technical Working Group (TWG). The co-ordination mechanism also saw the development of the county AYSRH strategic plan document, which borrowed a lot from TCI-University, to guide AYSRH programming.”
County Adolescent Health Representative—Kilifi County
“The position of county AY coordinator enabled the mapping of all AY stakeholders and formation of taskforce including the development of Migori county AY multisectoral action plan which borrowed a lot of HIIs from the TCI—University. The positions were also cascaded down to all the 8 subcounties”
County Adolescent Health Representative—Migori County
Adolescent visits to health facilities for services
In both Kilifi and Migori Counties, there was an increase in contraceptive uptake among adolescents (15–24 years) with a percentage increment of 59% and 28% respectively over the period of three years. However, there was a decrease of 21% in from 2018/2019 to 2019/2020 in Kilifi County for the 15–19 years (see Table 2 below). The start of Coronavirus Disease 2019 (Covid-19) pandemic and its related restrictions could have led to the decrease in the uptake of contraceptives.
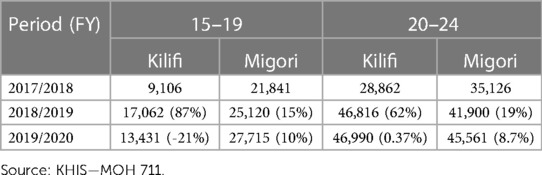
Table 2. Adolescent 15–24 years visits to health facilities for contraceptive services (Total number of adolescent visits to health facilities, percentage increase of adolescent visiting for contraceptive services for the period year).
Study limitations
The lack of age-disaggregated facility data on adolescents presenting with pregnancy and the absence of surveys hindered impact assessment on contraceptive uptake by age and measures of universal contraceptive services coverage. During the study period, data on adolescent contraceptive access from private facilities, including pharmacies and drug shops, was not obtained.
Discussion
Since 2018, both Kilifi and Migori Counties of Kenya progressively increased their financial commitments to AYSRH Program. This indicates that these counties have appreciated the importance of addressing the prevailing sexual and reproductive health related challenges which exacerbate the vulnerability of adolescents and youth to poverty, exclusion, and exploitation. These counties have assumed a greater role and responsibility of abating AYSRH challenges within their jurisdiction. This progress makes Kilifi and Migori Counties particularly exceptional in a country where the percentage of government funds devoted to AYSRH program is small despite increasing donor assistance for AYSRH Programs. The increase in financial commitments towards AYSRH by Kilifi and Migori Counties is in accordance with the treaties of the 2019 ICPD, where governments, including Kenya, agreed to enhance access to comprehensive AYSRH services and responsive information, education to all adolescents and youth (8). This development in the two counties also follows the Abuja Declaration (9).
The sustained increased allocation of more resources to tackle AYSRH challenges within these counties may have resulted from successful smart advocacy efforts by various partners, including TCI, which cultivated a mind-set shift towards resource allocation, increased ownership, increased adolescent contraceptive uptake and sustainability of AYSRH of programs. According to Korir et al., international NGOs and foundations have been the main financing agents in the provision of FP services in the country and it is not sustainable (11). If Kilifi and Migori continue with the same trend of financial commitment and allocation to AYSRH, then we may see sustained programs in these two counties in future. According to Starrs et al. 2018, to sustain the gains in AYSRH service provision and reduction in adolescent pregnancies, health systems need sustainable and predictable financing. County governments must make essential sexual and reproductive health services a priority and ensure they are included in health budgets. Provision of resources towards AYSRH is critical to ensure increased uptake of contraceptives among adolescents and reduction of adolescent pregnancies. Continuous advocacy efforts play a key role towards funds allocation and utilization for sustained implementation of AYSRH interventions.
The relative increase in expenditure on AYSRH Programs in both Kilifi and Migori Counties illustrate enthusiasm of the counties' structures to implement planned AYSRH interventions, which could eventually abate the prevailing AYSRH challenges, especially high rates of adolescent pregnancies. Evidence from research studies and other projects shows that effective FP interventions improve adolescent access to contraceptive services and hence reduction of adolescent pregnancies, maternal and infant mortality.
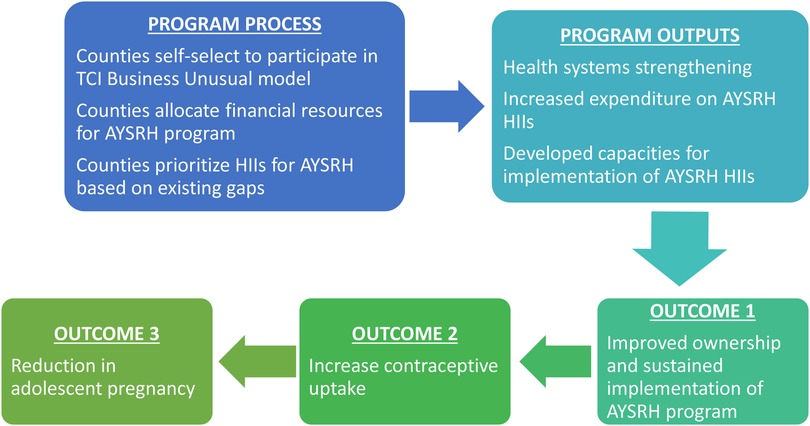
The allocated funds were spent in implementation of AYSRH Program HIIs. These HIIs have been adapted into Kilifi and Migori Counties' strategies and annual work plans, which increases the likelihood of sustained implementation. The early positive and promising results from the interventions may inspire the leadership of these two counties to sustain allocation of funds for AYSRH Program in future. The establishment of the position of AYSRH Coordinators across the two counties would strengthen coordination, accountability, management, and implementation quality of the AYSRH HIIs and ensure use of evidence for action. The conceptual framework, depicted in Figure 1, outlines the processes, outputs, and expected outcomes of the TCI program to ensure sustainable financing for AYSRH programs. The framework can be adapted by other implementers to achieve the same goals.
Conclusions and recommendations
Local governments can invest and sustain their own AYSRH programs contributing to improved adolescent and youth access to contraceptive services and hence reduction of adolescent pregnancies, maternal and infant mortality. This would also create an opportunity for women and girls to advance in their education and careers while improving their economic outcomes. To meet the needs and fulfill the rights of adolescents and youth, local governments should allocate funds and ensure their utilization for AYSRH interventions. Galvanization of political will and commitment for AYSRH at county leadership will ensure prioritization of adolescent health interventions. Continuous advocacy will ensure allocation and release of funds for health programs by empowering local community-based organizations, civil society organizations and youth groups to hold the leaders accountable on their promises. Local governments should embrace public private partnerships to leverage on resources in expanding FP commodities and services availability.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The John Hopkins IRB declared that ethical review and approval was not required for this study in accordance with the local legislation and institutional requirements. Written informed consent was not required for this study in accordance with the local legislation and institutional requirements.
Author contributions
LO, PK, NA and AM conceived the idea presented. LO, and KO developed the theory and performed the computations. PK and DS verified the analytical methods. KM and LN implemented the project and contributed to the interpretation of the results. PN encouraged LO to investigate the utilization of counties’ allocated resources on AYSRH and supervised the findings of this work. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Bill & Melinda Gates Foundation (OPP1145051). Bayer AG [JHU (Johns Hopkins University) Grant No. 123709], Comic Relief (JHU Grant No. 4581036). Bayer AG was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Morris JL, Rushwan H. Adolescent sexual and reproductive health: the global challenges. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. (2015) 131(Suppl 1):S40–42. doi: 10.1016/j.ijgo.2015.02.006
2. Touré C, Diallo M, Coulibaly B, Assama EA, Traore D, Bijou S, et al. Assessing application of WHO global standards for adolescent sexual and reproductive health services in five West African Countries (2021).
3. Kenya National Bureau of Statistics (NBS). 2019 Kenya Population and Housing Census Volume II: Distribution of Population by Administrative Units. (cited 2023 Feb 27). Available at: https://www.knbs.or.ke/download/2019-kenya-population-and-housing-census-volume-ii-distribution-of-population-by-administrative-units/#.
4. African Institute for Development Policy (AFIDEP). Adolescents (age 10–19) Presenting with Pregnancy at Health Facilities. African Institute for Development Policy—AFIDEP. (cited 2023 Feb 27). Available at: https://www.afidep.org/publication/adolescents-age-10-19-presenting-with-pregnancy-at-health-facilities/.
5. Ahmed S, Choi Y, Rimon JG, Alzouma S, Gichangi P, Guiella G, et al. Trends in contraceptive prevalence rates in sub-saharan Africa since the 2012 London summit on family planning: results from repeated cross-sectional surveys. Lancet Glob Health. (2019) 7(7):e904–11. doi: 10.1016/S2214-109X(19)30200-1
6. Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. Elsevier B.V. (2012) 380:165–71. doi: 10.1016/S0140-6736(12)60827-7
7. Joshi S, Schultz TP. Family planning and women's and children’s health: Long-term consequences of an outreach program in Matlab. Bangladesh; Available at: http://read.dukeupress.edu/demography/article-pdf/50/1/149/882040/149joshi.pdf.
8. UNFPA. Nairobi statement on ICPD25: accelerating the promise. p. 10. Available at: http://www.nairobisummiticpd.org/content/icpd25-commitments (2019).
9. World Health Organization. The Abuja declaration: ten years on. World Health Organization; (cited 2023 Feb 27). Report No.: WHO/HSS/HSF/2010.01. Available at: https://apps.who.int/iris/handle/10665/341162 (2010).
10. Ministry of Health Kenya M. Health sector working group report. (cited 2023 Feb 1). Available at: https://www.treasury.go.ke/wp-content/uploads/2021/05/HEALTH-REPORT-SWG-16.11.18-FINAL.pdf (2020).
12. Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, et al. Accelerate progress-sexual and reproductive health and rights for all: report of the guttmacher-lancet commission. Lancet Lond Engl. (2018) 391(10140):2642–92. doi: 10.1016/S0140-6736(18)30293-9
Keywords: adolescent, sexual, reproductive, health, program, financing, sustainable, local government
Citation: Otondi L, Aloo N, Kagwe P, Matekwa A, Miriti K, Njoki L, Sama DJ, Owino K and Nyachae P (2023) Sustainable financing of AYSRH programs by local governments through the TCI model. Front. Glob. Womens Health 4:1060857. doi: 10.3389/fgwh.2023.1060857
Received: 3 October 2022; Accepted: 28 February 2023;
Published: 30 March 2023.
Edited by:
Ilene S. Speizer, University of North Carolina at Chapel Hill, United StatesReviewed by:
Sydney Sauter, Tulane University School of Public Health and Tropical Medicine, United StatesCaroline Kabiru, African Population and Health Research Center (APHRC), Kenya
© 2023 Otondi, Aloo, Kagwe, Matekwa, Miriti, Njoki, Sama, Owino and Nyachae. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Levis Otondi Levis.Onsase@Jhpiego.org
Specialty Section: This article was submitted to Contraception and Family Planning, a section of the journal Frontiers in Global Women's Health
 Levis Otondi
Levis Otondi Nancy Aloo
Nancy Aloo Peter Kagwe1
Peter Kagwe1  Assumpta Matekwa
Assumpta Matekwa Paul Nyachae
Paul Nyachae