
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med., 14 October 2022
Sec. Cardiovascular Epidemiology and Prevention
Volume 9 - 2022 | https://doi.org/10.3389/fcvm.2022.972683
Introduction: Cardiovascular disease (CVD) remains the leading cause of premature death globally and a major contributor to decreasing quality of life. In the present study, we investigated the contribution of social, behavioral, and physiological determinants of CVD and their different patterns among middle-aged and older adults.
Methods: We used harmonized data from 6 nationally representative individual-level longitudinal studies across 25 countries. We restricted the age to ≥50 years and defined cases as a self-reported history of CVD. The exposure variables were the demographic status (age and sex), socioeconomic position (education level, employment, and household income level), social connections (marital status and family size), behavioral factors (smoking, alcohol drinking, and frequency of moderate to vigorous physical activity), and physiological risk factors (obesity, presence of hypertension, and presence of diabetes). Mixed logistic regression models were fitted to investigate the associations, and dominance analysis was conducted to examine the relative contributions.
Results: In total, 413,203 observations were included in the final analysis, with the CVD prevalence ranging from 10.4% in Mexico to 28.8% in the United States. Physiological risk factors were the main driver of CVD prevalence with the highest dominance proportion, which was higher in developing countries (China, 57.5%; Mexico, 72.8%) than in developed regions (United States, England, 10 European countries, and South Korea). Socioeconomic position and behavioral factors also highly contributed but were less significant in developing countries than in developed regions. The relative contribution of socioeconomic position ranged from 9.4% in Mexico to 23.4% in the United States, and that of behavioral factors ranged from 5.7% in Mexico to 26.1% in England.
Conclusion: The present study demonstrated the different patterns of determinant contributions to CVD prevalence across developing and developed countries. With the challenges produced by different risk factors, the implementation of tailored prevention and control strategies will likely narrow disparities in the CVD prevalence by promoting health management and enhancing the capacity of health systems across different countries.
Cardiovascular disease (CVD) remains the leading cause of premature mortality and is a major contributor to reduced quality of life and rising healthcare costs globally (1). From 1990 to 2019, the total number of cases of CVD nearly doubled from 271 million to 523 million, and this rise was accompanied by a steady increase in deaths (2). Middle-aged and older adults are among the most vulnerable populations and have the largest CVD burden (3), which hinders the achievement of healthy aging and causes significant direct and indirect economic hardships (4).
Recent analyses have demonstrated inequalities in the CVD prevalence across countries and regions, and prior studies investigated the associations of social, behavioral, and physiological risk factors individually (5–7), but rarely in the same context. Identifying the relative contributions of different risk factors can elucidate the mechanisms underlying social and environmental gradients and inform policy-making in CVD prevention and control. Most of the currently available data are derived from developed countries, whereas findings from developing countries are conflicting (8–12). Developing countries bear more than 80% of the global burden of CVD, and the gap between developing and developed countries is widening (13). Comparison among countries with varying developmental levels is a necessary step toward understanding how different risk factors shape the patterns of the CVD prevalence, and it can provide implications for multilateral global health actors to identify opportunities to reduce health inequalities by multi-sectoral cooperative activities.
To fill these research gaps, we investigated the contributions of socioeconomic position, social connection, and behavioral and physiological factors to the CVD prevalence among middle-aged and older adults in a series of unified and standardized population-based longitudinal studies conducted across 25 countries on 3 continents—North America, Europe, and Asia. Given that social and environmental risk factors for CVD are a multidimensional construct that largely depends on the context, we demonstrated the different patterns of determinant contributions across settings.
This study included six individual-level cohorts on aging that used modules similar to that of the Health and Retirement Study (HRS) in the United States (14), with harmonized data provided to facilitate the cross-national study of aging (https://g2aging.org/) (15). The HRS family surveys draw a nationally representative sample of the country's older population and are designed as longitudinal surveys with the goal of re-interviewing the same individuals on an approximately biennial basis. To maintain a nationally representative sample over time, periodic refresher samples bring in newly age-eligible respondents, although the frequency of refresher samples varies across surveys (15).
In this study, we obtained data from six family studies: the HRS; the Survey of Health, Aging and Retirement in Europe (SHARE) for 10 European developed countries (Austria, Belgium, Czech Republic, Denmark, France, Germany, Italy, Spain, Sweden, and Switzerland); the English Longitudinal Study of Aging (ELSA) in England; the Korean Longitudinal Study of Aging (KLoSA) in South Korea; the China Health and Retirement Longitudinal Study (CHARLS) in China; and the Mexican Health and Aging Study (MHAS) in Mexico. We categorized the included countries' level of development according to the income level from the World Bank database (https://data.worldbank.org/). Specifically, we included 13 developed countries (the United States, England, Austria, Belgium, Czech Republic, Denmark, France, Germany, Italy, Spain, Sweden, Switzerland, and South Korea) and 2 developing countries (China and Mexico).
Different waves were selected from each survey for a similar time range: HRS, 2010–2018; ELSA, 2010–2018; SHARE, 2011–2017; KLoSA, 2011–2019; CHARLS, 2011–2018; and MHAS, 2012–2018. We excluded participants aged <50 years and those with missing outcomes and exposures, and we finally enrolled 93,945 participants from HRS, 35,706 participants from ELSA, 178,133 participants from SHARE, 37,503 participants from KLoSA, 35,791 participants from CHARLS, and 32,125 participants from MHAS (Supplementary Table 1).
CVD was defined as a combination of a doctor-diagnosed heart problem and doctor-diagnosed stroke, but slight differences exist in phrasing across studies. The concordance across studies is shown in Supplementary Table 2. Respondents were asked whether they had had the condition since the last interview starting in the second wave. According to their responses, imputations were made by both the team of the gateway to global aging data and our team to obtain a correct report in each wave.
Five groups of risk factors were identified in this study: demographic status (age and sex), socioeconomic position (education level, employment, and household income level), social connections (marital status and family size), behavioral factors (smoking, alcohol drinking, and frequency of moderate to vigorous physical activity), and physiological risk factors (obesity, presence of hypertension, and presence of diabetes). All the variables are categorical, and detailed scales and cutoffs are listed in Supplementary Table 3.
To investigate the association between risk factors and CVD prevalence, we fitted mixed logistic models with repeated observations of individuals separately in each study. Unstructured mixed logistic modeling was used due to the nominal nature of the dependent variables. To account for clustering, a multilevel approach was adopted, and repeated individuals were fitted as the random effects. Regression coefficients and prospective odds ratios (with 95% CIs) in the logistic regression were calculated. To quantify the extent to which a risk factor was associated with the CVD prevalence, we conducted a dominance analysis for decomposition by examining the relative importance of explanatory variables that contributed to the R-squared of the regressions. All analyses were conducted using Stata 14.1 (StataCorp LP, College Station, TX, USA).
Table 1 shows the characteristics of the participants in each cohort. The prevalence of CVD in the HRS, ELSA, SHARE, KLoSA, CHARLS, and MHAS was 28.77, 23.53, 20.21, 13.14, 20.57, and 10.39%, respectively.
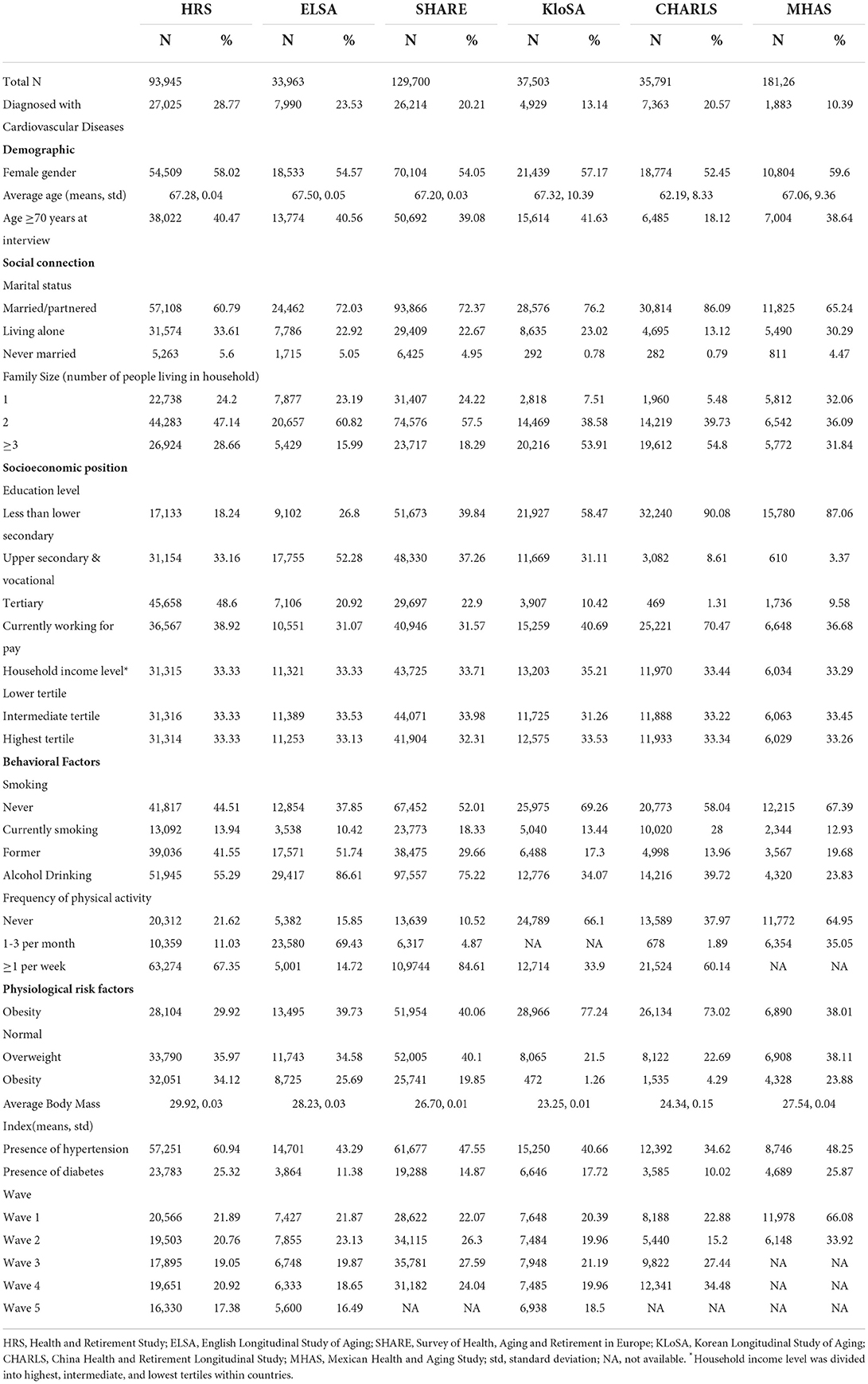
Table 1. Variables included in the present analysis with summary statistics by cohort (country/region).
The proportions of female and advanced-age patients were lowest in CHARLS (52.45 and 18.12%, respectively). The family size of the older population was larger than three in KLoSA and CHARLS, while the dominant family size was two in HRS, ELSA, and SHARE. A relatively lower education level was found in the middle-aged and older population in CHARLS and MHAS, with the proportion of tertiary education being 1.31 and 9.58%, respectively. The proportion of currently employed individuals was among the highest in CHARLS (70.47%). A relatively higher prevalence of smoking (combined prevalence of former and current smoking) was seen in HRS (55.49%) and ELSA (62.16%), and a high frequency of alcohol drinking was seen in ELSA (86.61%) and SHARE (75.22%). Individuals in KLoSA and MHAS engaged in relatively fewer physical activities than their counterparts in other cohorts, with proportions of 66.10 and 64.95% never engaging in physical activities, respectively. Obesity was less prevalent in KLoSA (1.26%) and CHARLS (4.29%).
As shown in Table 2, multiple groups of risk factors were found to be associated with the prevalence of CVD among the middle-aged and older population in all cohorts. With respect to the demographic status, female sex was negatively associated with the CVD prevalence (except for CHARLS, with the odds ratio of 1.06), whereas age was positively associated in all settings (p < 0.001 for all).
Social connection factors also mattered. Those living alone (compared with married/partnered) tended to have a higher CVD prevalence, with the ORs ranging from 1.00 in MHAS to 1.04 in SHARE. Those with a larger family size (≥3) had a significantly lower CVD prevalence in HRS (OR = 0.99) and SHARE (OR = 0.98).
In terms of socioeconomic position, we found that a higher education level, higher household income, and being employed were associated with a lower CVD prevalence in middle-aged and older individuals, although there were some exceptions as follows. Higher household income was significantly associated with a higher CVD prevalence in SHARE (OR = 1.01 in intermediate tertile and 1.01 in highest tertile), and a higher education level was associated with a higher CVD prevalence in CHARLS (OR = 1.03 in upper secondary and vocational education group and 1.05 in tertiary education group). There were also several non-significant associations with the education level in MHAS and the household income level in ELSA and MHAS.
Behavioral risk factors also played roles in the CVD prevalence. Current or former smoking, never drinking alcohol, and never engaging in moderate to vigorous physical activities were positively associated with the CVD prevalence. The significant ORs of current smoking, former smoking, alcohol drinking, engaging in physical activities one to three times per month, and engaging in physical activities more than once per week ranged from 0.98 in ELSA to 1.02 in HRS, from 1.02 in MHAS to 1.07 in HRS, from 0.94 in KLoSA to 0.99 in CHARLS, from 0.95 in ELSA to 0.99 in KLoSA, and from 0.93 in SHARE to 0.98 in CHARLS, respectively.
In terms of physiological risk factors, having been diagnosed with hypertension or diabetes was positively associated with the CVD prevalence in the full models, with ORs of 1.10 and 1.04 in HRS, 1.09 and 1.06 in ELSA, 1.08 and 1.08 in SHARE, 1.07 and 1.03 in KLoSA, 1.13 and 1.12 in CHARLS, and 1.10 and 1.02 in MHAS, respectively. A conflicting impact of obesity was observed among the different cohorts. Both overweight and obesity were associated with a higher CVD prevalence in CHARLS, with ORs of 1.01 and 1.05, respectively; however, they were associated with a lower CVD prevalence in HRS, with coefficients of 0.99 and 0.98, respectively.
Table 3 shows the results of the dominance analyses. Physiological factors were the main driver of the CVD prevalence in the middle-aged and older population. In developing countries and regions, physiological factors accounted for a high share of the predicted variance (as high as 72.8% in MHAS and 57.5% in CHARLS). In Western developed countries and regions, the relative contributions were much lower (dominance of 27.5% in HRS, 27.7% in ELSA, and 29.8% in SHARE). In the KLoSA cohort, the dominance of physiological factors was 37.3%.
The set of behavioral factors was one of the top drivers of the CVD prevalence, with opposite rankings across cohorts. In Western developed countries and regions, behavioral factors highly contributed to the CVD prevalence (as high as 17.7% in HRS, 26.1% in ELSA, and 17.7% in SHARE). The proportions were lower in cohorts in developing regions, including CHARLS (13.6%) and MHAS (5.7%). The dominance of behavioral factors in KLoSA was 14.9%.
Socioeconomic position was highly associated with the CVD prevalence in the middle-aged and older population of all cohorts, with dominance of 23.4% in HRS, 15.5% in ELSA, 15.5% in SHARE, 20.0% in KLoSA, 18.4% in CHARLS, and 9.4% in MHAS. Age also accounted for a high share of predicted variance, with dominance proportions of 23.4% in HRS, 21.8% in ELSA, 25.5% in SHARE, 18.8% in KLoSA, 4.9% in CHARLS, and 10.4% in MHAS.
The comparison of risk factor contribution patterns is shown in Figure 1. Although physiological factors were the major contributor to the CVD prevalence in the middle-aged and older population in all cohorts, the contributions were much higher in developing countries (CHARLS and MHAS). In Western developed countries and regions (HRS, ELSA, and SHARE), behavioral factors had very high contributions to the CVD prevalence. In the KLoSA cohort, where the level of economic development fell in the middle among all cohorts, the dominance proportion of the physiological factors and behavioral factors also showed a transitional trend between the two levels mentioned above.
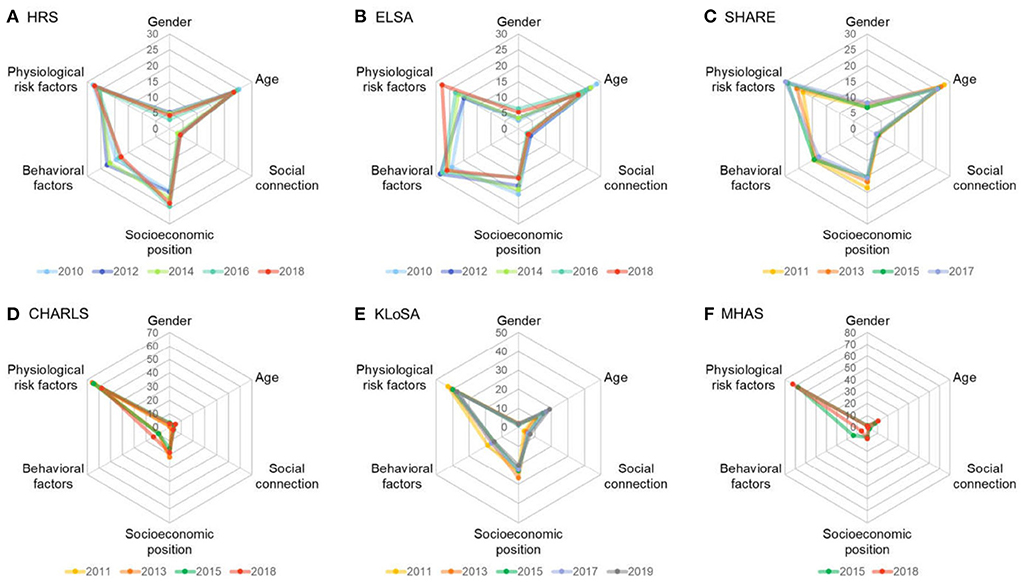
Figure 1. Contributions of the cardiovascular disease determinants by cohort. Data are presented as standardized dominance statistic (%). HRS, Health and Retirement Study; ELSA, English Longitudinal Study of Aging; SHARE, Survey of Health, Aging and Retirement in Europe; KLoSA, Korean Longitudinal Study of Aging; CHARLS, China Health and Retirement Longitudinal Study; MHAS, Mexican Health and Aging Study.
To the best of our knowledge, this is the first study to investigate the contributions of social, behavioral, and physiological determinants to the CVD prevalence in the middle-aged and older population. Although several determinants of CVD were well documented in prior studies, little research has been conducted on the contribution of each determinant in the same setting. With the growing burden of CVD and its widening disparities across countries and regions during the past decade, social determinants of health have been systematically considered to capitalize on CVD prevention and control strategies. However, different settings are faced with challenges introduced by different risk factors, the contributions of which can vary across developed and developing countries. By taking advantage of multi-country population-based cohorts, we were able to demonstrate the different patterns of determinant contributions across different countries and regions, highlighting the importance of national context in the CVD prevalence.
In the middle-aged and older population of our harmonized cohorts, we found that the prevalence of CVD was similar to that in previous studies of sample countries (16–18) but slightly lower than the national estimated prevalence (19). Nevertheless, we focused on confirming that five specific groups of risk factors (demographic characteristics, social connection, socioeconomic position, behavioral factors, and physiological risk factors) had significant impacts on the CVD prevalence in the middle-aged and older population, as indicated by prior studies (20). The association between demographic factors and the CVD prevalence is well documented. Age dominates the CVD risk factors (21–23), mainly because of the summed effects of prolonged exposure to other modifiable risk factors (24). Social connection is also important (especially the marital status as shown by a recent systematic review and meta-analysis (25)) through the mechanisms of spousal support (26), stress (27, 28), and selection theories (29). The impact of socioeconomic position on the risk of CVD has also been validated, although the context is important (8, 10, 30). Education has long been cited as a risk factor for CVD (7, 31). Behavioral factors are undoubtedly essential to the CVD prevalence, with the main drivers being an unhealthy diet, physical inactivity, tobacco use, and harmful use of alcohol (32–34). In terms of physiological risk factors, hypertension and diabetes are among the most important risk factors for CVD (33, 35), whereas obesity contributes both directly and indirectly to the CVD risk (36). Understanding the links of multiple groups of risk factors with the CVD prevalence can help to design public health interventions and policies for the neediest countries and regions.
Among all the determinants in the present study, physiological factors contributed the most in all cohorts, but the relative contribution was higher in the developing countries. In the developed countries, although the prevalence of obesity, hypertension, and diabetes was higher among the older population, the contribution of these factors to individual CVD variances was relatively low. This phenomenon may be largely due to the fact that chronic conditions were mostly under control by the well-functioning healthcare systems in developed countries (37), in which healthcare services such as pharmacological treatments, behavioral intervention, and environment support for chronic disease management are of high quality and homogeneity. In developed settings, the CVD mortality rate is relatively lower although the prevalence is higher than that in less-developed countries, and the national capacity of non-communicable disease control is reportedly an important reason for this (38). Most healthcare services for CVD prevention and control are included in universal health coverage packages in these countries, especially for the middle-aged and older population. Thus, these chronic conditions can be controlled more effectively with lifestyle interventions and more frequent use of proven pharmacologic therapies and revascularization (39), through which the incidence of secondary diseases such as CVD can be reduced, and the difference among populations is relatively small. Age, behavioral factors, and other risk factors may therefore have a relatively higher contributions in developed countries and regions, as shown by our results. In South Korea, which is undergoing both societal and epidemiological changes, we observed a relatively larger contribution of socioeconomic position and a smaller contribution of behavioral factors. Additionally, in line with recent studies, we recognized the potential coexistence of multiple chronic diseases/conditions among the older population, which may shift our current knowledge on single chronic diseases. Therefore, further studies must focus on the prevalence and cluster patterns of multiple chronic diseases to help better explain the roles of physiological factors.
We explored the potential mechanisms underlying the relatively high contribution of the socioeconomic position and behavioral factors to the CVD prevalence in the middle-aged and older population. The important roles of the health system may explain why the contribution of socioeconomic factors was higher in developing than developed countries because these factors hugely influence health literacy and access to healthcare services (40, 41). Intensive interactions between patients with chronic conditions and their care managers were reported in developed regions (42); this is a good example of improved management of chronic conditions under generally higher-quality healthcare systems and reduced disparity caused by individual socioeconomic factors. Global disparities in access to CVD care have resulted in an obvious hypertension and diabetes care cascade in developing countries. A study in 2017 showed that nearly half of Chinese adults aged 35 to 75 years had hypertension, but fewer than one-third were being treated and fewer than 1 in 12 had well-controlled blood pressure (43). Compared with China, the proportion of control in the United States (43.5%) was much higher (44). The situation was similar for patients with diabetes (45). The importance of behavioral factors is evident in Mexico, where access and quality of care are relatively low (46). Strengthening primary healthcare has been proven to be a cost-effective approach to address the cascade, but progress has stalled because of the complexity of horizontal interventions.
Considering ethnic, cultural, and context-related matters in determining the risk factors for disease as well as the comparative effectiveness of interventions (47), actions aiming to prevent and control the global CVD burden may need to tailor their approaches to different countries. In developed countries, reducing individual risk behaviors may be more effective in lowering the CVD burden, while in developing countries, strengthening the healthcare system may have higher priority. Moreover, joint international projects may help bridge the communication between developing and developed countries, which will facilitate sharing not only theoretical but also practical experiences of enhancing the capacity of healthcare systems.
This study had several limitations. First, the observational nature of our study limited our ability to investigate the causal relationship between risk factors and the CVD prevalence. Rather, the longitudinal associations found in the present study underscore the need for research to capitalize on the mechanistic basis behind the observed link between several social and environmental risk factors and inequalities in the CVD prevalence. Second, because of limitations in data availability, some other contributory factors (such as dietary factors) may have been excluded from this analysis, and these factors may vary across counties. Further studies will need to focus on dietary factors and their effects on the CVD prevalence among countries. Third, we attempted to identify differences in risk factors for CVD among different countries and regions with different social contexts. It was difficult to establish the parameters of the research. However, the methods for statistical analysis of data inherent in this study still contributed to the establishment of correlations between risk factors and the CVD prevalence in comparative studies and helped to provide implications for reducing the inequalities in the CVD prevalence by tacking with different risk factors in different settings.
The present study demonstrated the different patterns of determinant contributions across settings, highlighting the importance of national context in the CVD prevalence. Faced with the challenges produced by different risk factors, the implementation of tailored CVD prevention and control strategies may help to narrow disparities in the CVD prevalence by promoting health management and enhancing the capacity of healthcare systems across different countries.
Publicly available datasets were analyzed in this study. This data can be found here: https://g2aging.org/.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
JZ conceived the study, analyzed the data, and interpreted the results. YF interpreted the results and drafted the manuscript. YY, YZ, DY, and MS contributed to the study design and results interpretation. YJ and Z-JZ conceived and supervised the study. All authors critically reviewed the manuscript and approved it.
This paper was supported by the National Natural Science Foundation of China (No. 71904004), the Clinical Medicine Plus X - Young Scholars Project, Peking University, and the Fundamental Research Funds for the Central Universities (No. PKU2022LCXQ008).
We thank Angela Morben, DVM, ELS, from Liwen Bianji (Edanz) (www.liwenbianji.cn), for editing the English text of a draft of this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.972683/full#supplementary-material
1. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-92
2. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update From the GBD 2019 study. J Am Coll Cardiol. (2020) 76:2982–3021. doi: 10.1016/j.jacc.2020.11.010
3. Nanayakkara, S, Marwick TH, Kaye DM. The ageing heart: the systemic and coronary circulation. Heart. (2018) 104:370–6. doi: 10.1136/heartjnl-2017-312114
4. Afilalo J, Karunananthan S, Eisenberg EJ, Alexander KP, Bergman H. Role of frailty in patients with cardiovascular disease. Am J Cardiol. (2009) 103:1616–21. doi: 10.1016/j.amjcard.2009.01.375
5. Goyal A, Bhatt DL, Steg PG, Gersh BJ, Alberts MJ, Ohman EM, et al. Attained educational level and incident atherothrombotic events in low- and middle-income compared with high-income countries. Circulation. (2010) 122:1167–75. doi: 10.1161/CIRCULATIONAHA.109.919274
6. Mackenbach JP, Cavelaars AE, Kunst AE, Groenhof F. Socioeconomic inequalities in cardiovascular disease mortality; an international study. Eur Heart J. (2000) 21:1141–51. doi: 10.1053/euhj.1999.1990
7. Rosengren A, Smyth A, Rangarajan S, Ramasundarahettige C, Bangdiwala SI, AlHabib KF, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Glob Health. (2019) 7:e748–60. doi: 10.1016/S2214-109X(19)30045-2
8. Clark AM, DesMeules M, Luo W, Duncan AS, Wielgozs A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. (2009) 6:712–22. doi: 10.1038/nrcardio.2009.163
9. Harper S, Lynch J, Smith GD. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu Rev Public Health. (2011) 32:39–69. doi: 10.1146/annurev-publhealth-031210-101234
10. Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. (1993) 88:1973–98. doi: 10.1161/01.CIR.88.4.1973
11. Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart J. (2004) 148:7–15. doi: 10.1016/j.ahj.2003.11.027
12. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. (2018) 137:2166–78. doi: 10.1161/CIRCULATIONAHA.117.029652
13. Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. (2015) 132:1667–78. doi: 10.1161/CIRCULATIONAHA.114.008720
14. Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, Weir DR. Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol. (2014) 43:576–85. doi: 10.1093/ije/dyu067
15. Lee J, Phillips D, Wilkens J, Gateway to Global Aging Data Team. Gateway to Global Aging Data: Resources for Cross-NationaComparisons of Family, Social Environment, and Healthy Aging. J Gerontol B Psychol Sci Soc Sci. (2021) 76:S5–S16.16. doi: 10.1093/geronb/gbab050
16. Vintimilla R, Reyes M, Johnson L, Hall J, O'Bryant S. Cardiovascular risk factors in Mexico and the United States: a comparative cross-sectional study between the HABLE and MHAS participants. Gac Med Mex. (2020) 156:17–21. doi: 10.24875/GMM.M19000316
17. Han KT, Kim S. Regional prevalence of dyslipidemia, healthcare utilization, and cardiovascular disease risk in South Korean: a retrospective cohort study. Int J Environ Res Public Health. (2021) 18:538. doi: 10.3390/ijerph18020538
18. Lu Y, Wang P, Zhou T, Lu J, Spatz ES, Nasir K, et al. Comparison of Prevalence, Awareness, Treatment, and Control of Cardiovascular Risk Factors in China and the United States. J Am Heart Assoc. (2018) 7:e007462. doi: 10.1161/JAHA.117.007462
19. Institute for Health Metrics Evaluation. Global Burden of Disease Study 2019 results tool. (2021). Available online at: http://ghdx.healthdata.org/gbd-results-tool (accessed May 28, 2022).
20. Reshetnyak E, Ntamatungiro M, Pinheiro LC, Howard VJ, Carson AP, Martin KD, et al. Impact of multiple social determinants of health on incident stroke. Stroke. (2020) 51:2445–53. doi: 10.1161/STROKEAHA.120.028530
21. Paneni F, Diaz Cañestro C, Libby P, Lüscher TF, Camici GG. The aging cardiovascular system: Understanding it at the cellular and clinical levels. J Am Coll Cardiol. (2017) 69:1952–67. doi: 10.1016/j.jacc.2017.01.064
22. North BJ, Sinclair DA. The intersection between aging and cardiovascular disease. Circ Res. (2012) 110:1097–108. doi: 10.1161/CIRCRESAHA.111.246876
23. Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. (2011) 123:933–44. doi: 10.1161/CIR.0b013e31820a55f5
24. Kovacic JC, Moreno P, Hachinski V, Nabel EG, Fuster V. Cellular senescence, vascular disease, and aging: Part 1 of a 2-part review. Circulation. (2011) 123:1650–60. doi: 10.1161/CIRCULATIONAHA.110.007021
25. Wong CW, Kwok CS, Narain A, Gulati M, Mihalidou AS, Wu P, et al. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart. (2018) 104:1937–48. doi: 10.1136/heartjnl-2018-313005
26. Austin D, Yan AT, Spratt JC, Kunadian V, Edwards RJ, Egred M, et al. Patient characteristics associated with self-presentation, treatment delay and survival following primary percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care. (2014) 3:214–22. doi: 10.1177/2048872614527011
27. Kriegbaum M, Christensen U, Lund R, Prescott E, Osler M. Job loss and broken partnerships: do the number of stressful life events influence the risk of ischemic heart disease in men? Ann Epidemiol. (2008) 18:743–5. doi: 10.1016/j.annepidem.2008.04.010
28. Vujcic I, Vlajinac H, Dubljanin E, Vasiljevic Z, Matanovic D, Maksimovic J, et al. Long-term prognostic significance of living alone and other risk factors in patients with acute myocardial infarction. Ir J Med Sci. (2015) 184:153–8. doi: 10.1007/s11845-014-1079-2
29. Floud S, Balkwill A, Canoy D, Wright FL, Reeves GK, Green J, et al. Marital status and ischemic heart disease incidence and mortality in women: a large prospective study. BMC Med. (2014) 12:42. doi: 10.1186/1741-7015-12-42
30. Hawkins NM, Jhund PS, McMurray JJV, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail. (2012) 14:138–46. doi: 10.1093/eurjhf/hfr168
31. Tousoulis D, Oikonomou E, Vogiatzi G, Vardas P. Cardiovascular disease and socioeconomic status. Eur Heart J. (2020) 41:3213–4. doi: 10.1093/eurheartj/ehaa405
32. Frieden TR, Cobb LK, Leidig RC, Mehta S, Kass D. Reducing premature mortality from cardiovascular and other non-communicable diseases by one third: achieving sustainable development goal indicator 341. Glob Heart. (2020) 15:50. doi: 10.5334/gh.531
33. Joseph P, Leong D, McKee M, Anand SS, Schwalm J-D, Teo K, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circ Res. (2017) 121:677–94. doi: 10.1161/CIRCRESAHA.117.308903
34. Leong DP, Joseph PG, McKee M, Anand SS, Teo KK, Schwalm J-D, et al. Reducing the global burden of cardiovascular disease, part 2: prevention and treatment of cardiovascular disease. Circ Res. (2017) 121:695–710. doi: 10.1161/CIRCRESAHA.117.311849
35. Resnick HE. and Howard BV. Diabetes and cardiovascular disease. Annu Rev Med. (2002) 53:245–67. doi: 10.1146/annurev.med.53.082901.103904
36. Powell-Wiley TM, Poirier P, Burke LE, Després J-P, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. (2021) 143:e984–e1010. doi: 10.1161/CIR.0000000000000973
37. GBD 2016 Healthcare Access and Quality Collaborators. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. (2018) 391:2236–71. doi: 10.1016/S0140-6736(18)30994-2
38. Zhang J, Jin Y, Jia P, Li N, Zheng Z-J. Global gender disparities in premature death from cardiovascular disease, and their associations with country capacity for noncommunicable disease prevention and control. Int J Environ Res Public Health. (2021) 18:10389. doi: 10.3390/ijerph181910389
39. Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. (2014) 371:818–27. doi: 10.1056/NEJMoa1311890
40. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
41. Dickman SL, Himmelstein DU, Woolhandler S. Inequality and the health-care system in the USA. Lancet. (2017) 389:1431–41. doi: 10.1016/S0140-6736(17)30398-7
42. Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, Mola E, et al. Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. (2010) 6:297–305. doi: 10.2147/VHRM.S9252
43. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 17 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. (2017) 390:2549–58. doi: 10.1016/S0140-6736(17)32478-9
44. Dorans KS, Mills KT, Liu Y, He J. Trends in Prevalence and Control of Hypertension According to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. (2018) 7:e008888. doi: 10.1161/JAHA.118.008888
45. Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. (2017) 317:2515–23. doi: 10.1001/jama.2017.7596
46. OECD. Cardiovascular Disease and Diabetes: Policies for Better Health and Quality of Care.(2015).
Keywords: prevalence, risk factors, country-level disparity, dominance analysis, cardiovascular disease(s)
Citation: Zhang J, Fang Y, Yao Y, Zhao Y, Yue D, Sung M, Jin Y and Zheng Z-J (2022) Disparities in cardiovascular disease prevalence among middle-aged and older adults: Roles of socioeconomic position, social connection, and behavioral and physiological risk factors. Front. Cardiovasc. Med. 9:972683. doi: 10.3389/fcvm.2022.972683
Received: 18 June 2022; Accepted: 26 September 2022;
Published: 14 October 2022.
Edited by:
Sebhat Erqou, Brown University, United StatesReviewed by:
Jaejin An, Kaiser Permanente Southern California, United StatesCopyright © 2022 Zhang, Fang, Yao, Zhao, Yue, Sung, Jin and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yinzi Jin, eXpqaW5AYmptdS5lZHUuY24=; Zhi-Jie Zheng, emhlbmd6akBiam11LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.