Introduction: Effective treatment of brain disorders remains a major clinical challenge due to the blood-brain-barrier (BBB). Surface modification of nanoparticles (NPs) with targeting ligands has been shown to improve delivery and efficacy of encapsulated drugs in the brain. However, whether this improvement reflects transport of NPs across the BBB remains under active debate. We recently observed that delivery of a small molecule from brain-targeted NPs varied by as much as 80% across brain regions, which was driven by differences in regional blood flow for both control (CTR) and targeted NPs[1]. Here, we developed a multispectral labeling strategy to test the hypothesis that payload delivery from brain-targeted NPs occurs in absence of NP movement across the BBB.
Methods: NPs were produced by single emulsion, and post-modified with rabies virus glycoprotein (RVG) or the transactivator of transcription of HIV (TAT). Nile red (NR) was encapsulated to measure payload delivery by fluorescence in brain homogenates of healthy mice. NH2-quantum dots (QD) were linked to carboxy-poly(lactide)-b-poly(ethylene glycol) by EDC chemistry and blended with parent polymer (QD-NP) for NP tracking by confocal microscopy. NP size and zeta potential were measured by dynamic light scattering. Cell viability was measured by Cell TiterGlo. Healthy or intracranial GL261 tumor bearing C57 mice were perfused by cardiac puncture 0.5, 2, 6, or 24 hrs after tail vein injection of NPs.
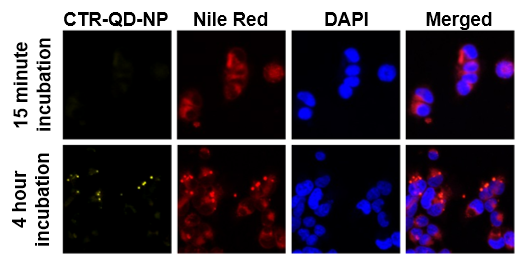
Results: TAT and RVG increased NR delivery to the brain by 79% and 51% relative to CTR NPs at 2 hrs, demonstrating ligand functionality. QD-NPs were confirmed to be nontoxic in HEK cells (up to 5 mg/ml NP) after 24 hr incubation.NP size did not significantly change across formulations (p=0.96, 1-way ANOVA), and all formulations had zeta potentials between -2 and -7 mV. In vitro NR leached rapidly into cells, whereas punctate QD signal was only observed after several hours (Fig 1).
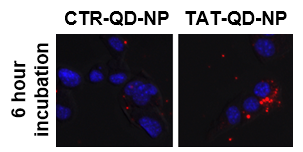
Targeting increased NP uptake by HEK cells in vitro (Fig 2); however, exhaustive imaging analysis failed to reveal TAT or RVG QD-NPs in BBB cells or parenchyma of healthy mice at any time point (not shown).
In contrast, QD-NPs were readily visualized in peripheral organs. For example, RVG and CTR QD-NPs co-administered to single mice could both be detected in spleen at 2 hrs but only RVG-QD-NPs were observed at 24 hrs (Fig 3A). QD-NPs administered to intracranial tumor bearing mice were also easily detected in the malformed vasculature of the tumor core at 2 hrs, presumably due to the enhanced permeation and retention effect (Fig 3B), but did not enter the parenchyma, even at later time points.
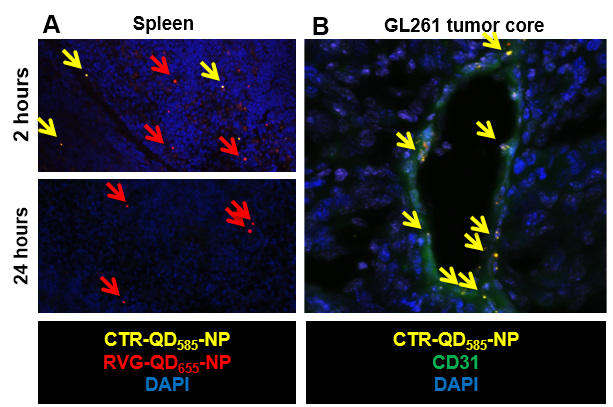
Conclusions: QD-NPs are stable, nontoxic, have reproducible biophysical properties, and can be used to track NP distribution with subcellular resolution in vitro and in vivo. Our data confirm that ligand modification improves payload delivery to the brain, but we observed no evidence for NP transport across an intact BBB. NPs were, however, able to access the leaky core of intracranial tumors. These results demonstrate discordance between delivery of payload vs intact NPs and support a model for CNS-targeted delivery based on transfer of drug from NP to cells in absence of significant NP internalization.
References:
[1] Cook et al., in revision