Introduction :
Collagen membrane is currently used for guided bone regeneration. Human amniotic membrane (hAM) is a highly abundant and readily available tissue that may be helpful as a support for bone regeneration. hAM contains two different cell types: human Amnion Epithelial Cells (hAECs) and human Amnion Mesenchymal Stem Cells (hAMSCs) that have a strong osteoinductive potential in vitro[1][2]. Lyophilized hAM has the same efficacy than collagen membrane to improve clinical periodontal parameters in the treatment of intrabony defect[3]. The aim of this project was to analyze bone regeneration potential of hAM implanted in mice calvarial bone defect. We have investigated i) the role of epithelial and mesenchymal layers on bone regeneration efficiency in a model of calvarial critical defect, ii) its efficacy compared to collagen membrane and iii) the consequences of cryopreservation.
Materials and methods:
hAM cryopreservation vs fresh membranes: hAM were recovered after elective cesarean surgery, cut in pieces of 6x6 mm and either used as fresh tissue or cryopreserved.
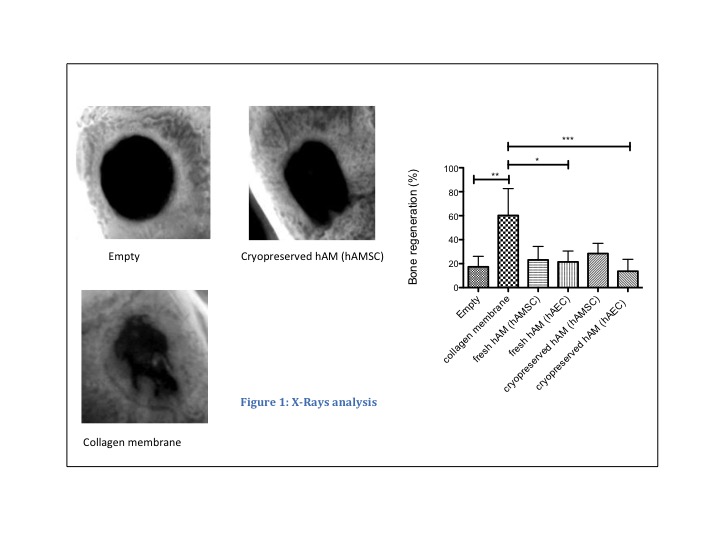
In vivo procedure: Critical bone defects (3.3mm diameter) were performed in adult mice calvaria. Defects remained free or were covered either by a fresh or cryopreserved hAM fragment in each orientation, or the defect was covered by a collagen membrane (Geistlich Bio-Gide®) (n=8). Sacrifice was performed after 8 weeks and bone regeneration was quantified by X-rays (faxitron). Decalcified histological analysis was done using trichrome Masson’s staining to analyze bone formation and to assess the amount of residual hAM. Kruskal & Wallis comparisons were used.
In vitro : Fresh and cryopreserved hAM fragments were cultived in basal medium during two weeks. hAM cell viability was analyzed with live/dead staining.
Results:
In vivo, X-Rays analysis showed that no defect was regenerated ad integrum. Quantitative analysis established that collagen membrane induced bone formation with a higher efficiency as compared with fresh or cryopreserved hAM when the epithelial side was on contact of the bone.
. These results were confirmed by histological analysis from which we could observe bone formation in the periphery of the defect. Histological analysis also showed that hAM was almost entirely resorbed 8 weeks after implantation. 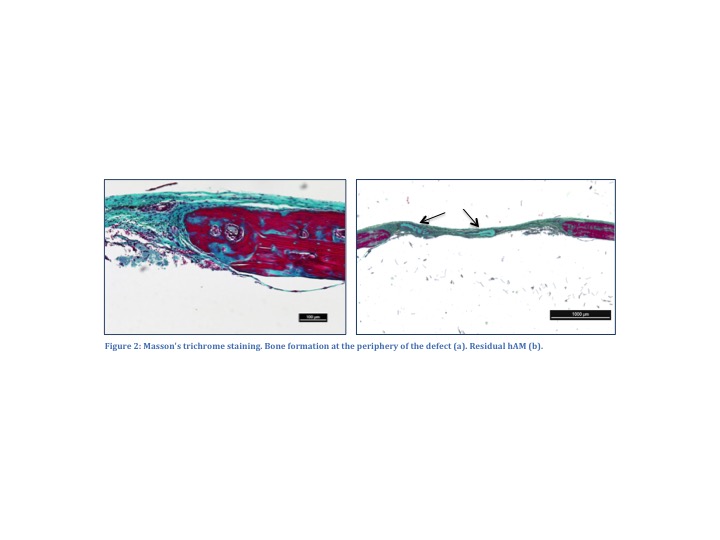
In vitro, Live/Dead staining showed significant heterogeneity regarding the viability of cells within the same piece of membrane. Cell viability assays also showed very few hAM cells alived after thawing, especially in the epithelial side. However, after 7 days, dividing cells were detected (AECs and hAMSCs).
Discussion-Conclusion:
hAM alone did not allow regeneration ad integrum of critical calvaria bone defect in mice and collagen membrane induced bone formation with a higher efficiency.
We propose now to investigate in the same model i) the osteogenic potential of cryopreserved hAM associated with hydroxyapatite or hydroxyapatite and BMP-2 and ii) to compare its efficacy with the same collagen membrane.
Fondation des Gueules Cassées; Fédération de Recherche TecSan; Etablissement Français du Sang Aquitaine Limousin
References:
[1] Soncini M et al., J Tissue Eng Regen. 1:296–305, 2007
[2] Lindenmair A et al., Biomaterials. 31:8659-8665, 2010
[3] Kiany F and Maloudy F, Int j oral maxillofac implants ;30:639–647, 2015